Are there any novel radiological diagnostic clues in magnetic resonance imaging for vertebrobasilar insufficiency?
Introduction
Vertebrobasilar insufficiency (VBI) is an enigmatous disorder with an obscure underlying pathophysiology. While some authors suggest that thromboembolism is the main cause, others advocate that there is a hemodynamic phenomenon which resources from the compromise of blood flow velocity in vertebral arteries (1-3).
Evaluation and quantitative analysis of blood flow in vertebrobasilar system may be useful for establishing diagnosis. Flow, volume, peak systolic or end diastolic flow rates and vascular diameter are among radiological parameters used in this purpose. However, the diagnosis of VBI still constitutes a diagnostic challenge because its manifestations are subjective and difficult to quantify (4).
Owing to the non-tapered and plain configuration of vertebral arterial system in the cervical segment, flow measurements seem to be reliable (4). However, validation of normal values and reference data for radiological standards of blood flow is troublesome and further assessment of the vertebrobasilar circulation by means of noninvasive studies may hopefully provide further insight into the pathophysiological process of VBI.
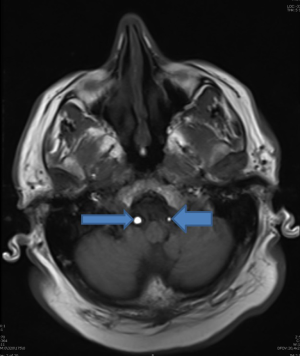
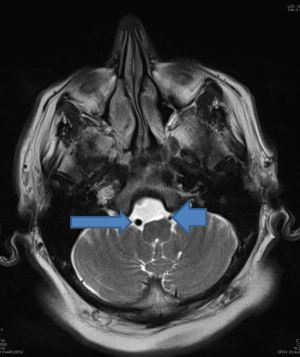
Doppler ultrasonography and magnetic resonance imaging (MRI) are two important measures for diagnosis of VBI (5,6). On T2 weighted noncontrast axial MRI sequences, “slice-entry phenomenon” can exist due to the variability of blood flow in vertebral arteries (3). Accelerated blood flow results in failure of detection of protons leading to hypointense (black) appearance of intravascular structures. In contrast, decreased blood flow allows coding of protons and resulting in hyperintense (white) images in T2 weighed sequences (7).
The main aim of this case-control study was to compare the radiological features of blood flow of VBI under Doppler ultrasonography and MRI views. In this purpose, blood flow, vessel diameter, mean, peak systolic and end diastolic velocities, resistive and pulsatility indices were evaluated in VBI patients and healthy controls. Any association between signal intensities in T2 weighted axial MRI views of vertebrobasilar systems and radiological characteristics of blood flow in Doppler ultrasonography were sought to explore any novel diagnostic clues.
Materials and methods
Study design
Subsequent to obtaining written informed consent from all participants, 18 VBI patients, and 58 controls were enrolled. The whole group consisted of 54 women (71.1%) and 22 men (28.9%) with an average age of 46.86±13.53 (range, 20-76).
Patients have initially admitted with clinical signs of VBI such as vertigo, drop attacks, tinnitus, and ataxia. They were referred to the radiology department with the presumable diagnosis of VBI. Confirmation of diagnosis was made based on Doppler ultrasonography and MRI/magnetic resonance angiography (MRA). MRI and MRA were performed in one sitting (Figures 1,2). Signals of T2 weighted noncontrast MRI on signals of both vertebral arteries were examined to compare the radiological features to data derived from Doppler ultrasonography (Figures 3,4). Radiological evaluation was made by the same staff radiologist (EC) having 5 years of experience in neuroradiology. MRI was made on circular head and neck sequences using Philips 0.5T Gyroscan T5-NT device (MagNET, South Kensington, London, UK).
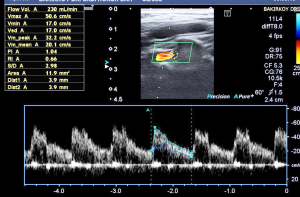
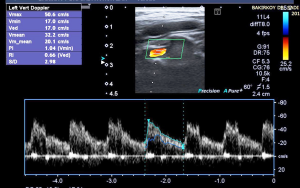
Diagnosis of VBI was set if the total blood flow through bilateral vertebral arteries was less than 200 mL/minute in Doppler ultrasonography (8). Toshiba SSA 270A colour Doppler ultrasound was used together with 5 and 7.5 mHz transducers (Toshiba Medical Systems Corp., Otawara-shi, Tochigi-ken, Japan). The blood flow and velocity of vertebral arteries were assessed by a single measurement performed by the same radiologist (EC) between 3rd and 4th cervical vertebrae with a Doppler angle of 45-65°.
MRA was carried out using 2D cine phase device on a 1.5 T machine for quantitative evaluation of blood flow. Flow encoding was encoding in a caudal to cranial direction and sequence parameters, imaging plane and pixel intensities were adjusted as described by Kato et al. (5). Sequence parameters were as follows: 40/11.8/2 (TR/TE/NEX); flip angle, 30 degrees; matrix, 256×192; field of view, 18 cm; section thickness, 5 mm; interpolated phases per RR interval, 32. Velocity encoding was adjusted to a maximum value of 150 cm/s. Flow encoding direction was from caudal to cranial. Exclusion criteria included uncontrolled hypertension, cardiac failure, subclavian steal phenomenon, hypoplastic vertebral artery, patent posterior communicating arteries or segmental stenosis of vertebral artery.
Outcome parameters
Descriptive parameters (age, gender) and radiological features of vertebral arterial blood flow in Doppler ultrasonography and MRI views were noted in both VBI and control groups. Characteristics of blood flow consisted of peak systolic and end diastolic flow rates, resistance and pulsatility indices, mean velocities, flow rates and diameter.
Pulsatility index was defined as the difference between peak systolic and minimum diastolic velocities divided by the mean velocity during cardiac cycle (9). Resistance index indicates is a measure of pulsatile blood flow that reflects the resistance to blood flow due to microvascular bed distal to the measurement site (10).
Signal appearances on MRI sequences on both sides were classified as either hypo- or hyperintense according to the speed of the blood flow which constitutes the basis of “slice entry phenomenon”.
Statistical analysis
Data were analyzed using the IBM Statistical Package for Social Sciences (SPSS) Statistics 20 software (SPSS Inc., Chicago, IL, USA). Frequency distribution was calculated for categorical variables, while descriptive statistics were established for continuous variables. Normal distribution of continuous variables was evaluated with Kolmogorov Smirnov test. Comparison of two independent groups was made with Independent-Samples T test and Mann-Whitney U test. Categorical variables were compared using exact method for Pearson Chi Square test. Quantitative data were shown as mean, standard deviation, median, minimum and maximum values. Confidence interval was 95% and level of significance was set at P<0.05.
This case-control study was carried out in the radiology department of our tertiary care center after the approval of the local Institutional Review Board.
Results
Descriptive parameters (age and gender) did not display any significant difference between VBI and control groups (Table 1). Comparative overview of variables under investigation is shown on Table 1 and interestingly, only blood flow and vessel diameter were significantly decreased in VBI patients for both left and right sides (P<0.001). Other parameters did not exhibit any remarkable difference between VBI and control groups. Presence of lacunar infarcts in both cases and control groups also did not show significant difference.
Full table
Distribution of signals in VBI and control groups did not reveal any noteworthy differences (Table 2). In other words, the alteration of blood flow in VBI seemed not to result in any alterations of signal intensities on T2 weighted MRI sequences that may possess diagnostic value in the current series.
Full table
Blood flow characteristics in cases revealing either dark or opaque signals on MRI images are demonstrated in Table 3. No significant differences could be observed for any parameters between cases presenting with different signal patterns.
Full table
Discussion
In this study, we attempted to assess whether signal intensities on T2 weighted noncontrast MRI views and radiological findings derived from Doppler ultrasonography may have a diagnostic value for VBI.
VBI constitutes a diagnostic challenge and determination of absolute and clear-cut definitions cannot be made for thresholds of VBI. Furthermore, even non-vascular factors such as osteophytic spurs of cervical vertebra may mimick VBI even if vertebral arterial blood flow is normal. It has been postulated that VBI symptoms maya rise due to microcirculation problems in the presence of completely normal looking vertebral arteries (4,11).
Color Doppler ultrasonography is commonly for evaluation of the obstructive disease of the arteries (12-14). Attributed to technical difficulties, vertebral arteries have not been considered frequently in terms of both clinical and radiological aspects (12,15). However, increased awareness on VBI has changed this tendency especially in the last decade.
Visualization studies showed that imaging of the vertebrobasilar arteries can be extremely complex and variable. During the MR experiments, the same segment of a vessel could appear very different depending on the pulse sequence (16). The findings in MRI were classified with respect to the degree of ventricular dilatation, callosal degeneration, and lacunar infarction (2,17). Assessment with MRA was made according to the degree of pathological changes in the blood vessels (5). Not only a significant difference was observed in lacunar infarction on the MRI findings between VBI cases and normal controls, but also there were significant differences in side differences in the vertebral artery between VBI cases and peripheral vertigo and normal controls. Nakagawa et al. compared the MRA results of middle-aged and older VBI cases with those of age-matched peripheral disorder cases (6). In their study, MRA results were quantitatively assessed by scores determined on the basis of the severity of stenosis in the vertebral arteries and basilar artery. The severity of stenosis and the MRA score of VBI cases were significantly higher than those of peripheral cases. They concluded that MRA can be of value as a screening examination for estimating vertebrobasilar blood flow and can provide helpful information for diagnosing VBI. Nakagawa et al., in another study, assessed the usefulness of evaluating basilar arterial flow by MRA (18). MRA results for patients with VBI were compared with those for age-matched individuals with no vestibular disorders. Their findings suggested that MRA is valuable for the estimation of vertebrobasilar hemodynamics. MRA evaluation of basilar artery stenosis appears to be suitable for identifying a high-risk group among VBI patients, since basilar artery stenosis can result in serious disabilities. We propose an etiology for hemodynamic VBI: a functional cerebral circulation disorder causes ischemia of the basal ganglia and leads to lacunar infarctions; furthermore, the side difference between the two vertebral arteries causes a circulation disorder in the vertebrobasilar system (2).
The slice entry phenomenon arises in MRI when blood with unsaturated spins flows in the observed slices. These spins will emit a strong signal attributed to their unsaturated status. The number of slices affected depends on the velocity of flow and the thickness of the slice, while the direction of the flow determines the slices are affected (17).
Our results have demonstrated that only blood flow and diameter of vertebral arteries seem to possess diagnostic potential to rule in VBI. Other parameters including peak systolic or end diastolic flow velocities, resistive and pulsatility indices seem not to provide any additional contribution. Moreover, signal intensities achieved from T2 weighted noncontrast MRI sequences are unlikely to have a remarkable value or any association with clinical or sonographic findings. Limitations of this study include relatively small sample size and performance of measurements by the same radiologist. Therefore, extrapolations and interpretations must be made with caution.
To conclude, results of the present study indicate that assessment of blood flow and vascular diameter may be important for ruling in VBI. On the other hand, signal intensity patterns of vessels in MRI seem not reveal any data of diagnostic significance in these cases. Further studies on larger populations may allow development and exploration of newer diagnostic techniques and clues for VBI.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Bruyn GW. Vertigo and vertebrobasilar insufficiency. A critical comment. Acta Otolaryngol Suppl 1988;460:128-34. [PubMed]
- Fujita N, Yamanaka T, Ueda T, Miyahara H, Matsunaga T. Magnetic resonance imaging (MRI) test in hemodynamic vertebro-basilar insufficiency. Acta Otolaryngol Suppl 1998;533:57-9. [PubMed]
- Kikuchi S, Kaga K, Yamasoba T, Higo R, O'Uchi T, Tokumaru A. Slow blood flow of the vertebrobasilar system in patients with dizziness and vertigo. Acta Otolaryngol 1993;113:257-60. [PubMed]
- Kizilkilic O, Hurcan C, Mihmanli I, Oguzkurt L, Yildirim T, Tercan F. Color Doppler analysis of vertebral arteries: correlative study with angiographic data. J Ultrasound Med 2004;23:1483-91. [PubMed]
- Kato T, Indo T, Yoshida E, Iwasaki Y, Sone M, Sobue G. Contrast-enhanced 2D cine phase MR angiography for measurement of basilar artery blood flow in posterior circulation ischemia. AJNR Am J Neuroradiol 2002;23:1346-51. [PubMed]
- Nakagawa T, Yamane H, Nakai Y, Shigeta T, Takashima T. Evaluation of the vertebrobasilar artery system by magnetic resonance angiography in the diagnosis of vertebrobasilar insufficiency. Acta Otolaryngol Suppl 1998;538:54-7. [PubMed]
- Hurley MC, Soltanolkotabi M, Ansari S. Neuroimaging in acute stroke: choosing the right patient for neurointervention. Tech Vasc Interv Radiol 2012;15:19-32. [PubMed]
- Pellerito J, Polak JF. Introduction to Vascular Ultrasonography. 6 ed. Philadelphia: Elsevier Saunders, 2012.
- Available online: http://medical-dictionary.thefreedictionary.com/pulsatility+index, accessed on Dec 27, 2014.
- Available online: http://en.wikipedia.org/wiki/Arterial_resistivity_index, accessed on Dec 27, 2014.
- Cloud GC, Markus HS. Diagnosis and management of vertebral artery stenosis. QJM 2003;96:27-54. [PubMed]
- Kuhl V, Tettenborn B, Eicke BM, Visbeck A, Meckes S. Color-coded duplex ultrasonography of the origin of the vertebral artery: normal values of flow velocities. J Neuroimaging 2000;10:17-21. [PubMed]
- Seidel E, Eicke BM, Tettenborn B, Krummenauer F. Reference values for vertebral artery flow volume by duplex sonography in young and elderly adults. Stroke 1999;30:2692-6. [PubMed]
- Bendick PJ, Glover JL. Vertebrobasilar insufficiency: evaluation by quantitative duplex flow measurements. A preliminary report. J Vasc Surg 1987;5:594-600. [PubMed]
- Schöning M, Walter J, Scheel P. Estimation of cerebral blood flow through color duplex sonography of the carotid and vertebral arteries in healthy adults. Stroke 1994;25:17-22. [PubMed]
- Chong BW, Kerber CW, Buxton RB, Frank LR, Hesselink JR. Blood flow dynamics in the vertebrobasilar system: correlation of a transparent elastic model and MR angiography. AJNR Am J Neuroradiol 1994;15:733-45. [PubMed]
- Nagahata M, Abe Y, Ono S, Hosoya T, Uno S. Surface appearance of the vertebrobasilar artery revealed on basiparallel anatomic scanning (BPAS)-MR imaging: its role for brain MR examination. AJNR Am J Neuroradiol 2005;26:2508-13. [PubMed]
- Nakagawa T, Shigeta T, Takashima T, Tomiyama K. Magnetic resonance angiography evaluation of basilar artery stenosis in patients with vertebrobasilar insufficiency. Eur Arch Otorhinolaryngol 2000;257:409-11. [PubMed]


