Correlation between imaging features of Pneumocystis Jiroveci Pneumonitis (PCP), CD4+ T lymphocyte count, and plasma HIV viral load: A study in 50 consecutive AIDS patients
Abstract
Purpose: To investigate the imaging manifestations of Pneumocystis Jiroveci Pneumonitis (PCP) in AIDS patients, and the correlation between imaging features, CD4+ lymphocyte count, and plasma HIV viral load.
Material and methods: A total of consecutive 50 AIDS patients with PCP were review retrospectively. Chest CT manifestations, CD4+ lymphocyte count, and plasma HIV viral load were analyzed to investigate their correlation.
Results: PCP chest CT manifestations included ground-glass opacities dominated in 28 cases (28/50, 56%), lung cysts dominated in 10 cases (10/50, 20%), consolidation dominated in 6 cases (6/50, 12%), interstitial lesion dominated in 3 cases (3/50, 6%), and mixed lesions in 3 cases (3/50, 6%). In these 50 patients, CD4+ lymphocyte count ranged from 2~373 cells/μL. Plasma HIV viral load ranged from 500~5.28×107 copies/mL. CD4+ lymphocyte count in ground-glass opacities dominated patients was higher than that of lung cyst dominated patients (P<0.05). Plasma virus load of lung cysts dominated PCP patients was higher than that of consolidation dominated patients (P<0.05).
Conclusions: The typical chest imaging features of PCP in AIDS patients included lung ground-glass opacities and lung cysts. The chest imaging features were correlated with CD4+ T lymphocyte count and plasma HIV viral load.
Key words
Acquired Immunodeficiency Syndrome (AIDS); Pneumocystis Jiroveci Pneumonitis; Tomography; X-ray computed; CD4+ lymphocyte counts; Virus load
Acquired immunodeficiency syndrome (AIDS) patients have low immune function, with CD4+ lymphocyte count progressively decreases as disease progresses. When the CD4+ count falls below 200 cells/μL, AIDS patients gradually present with clinical symptoms (1,2). Plasma HIV virus load and CD4+ lymphocyte count are two important biomarkers for assessing clinical course of HIV-infected patients, predicting clinical progress and evaluating therapy of anti-HIV drugs (3). CD4+ lymphocyte count provides information of the status of the compromised immune system of HIV-infected patients. Because of severe cellular immune disfunction, AIDS patients can have a variety of fateful opportunistic infections. Pneumocystis Jiroveci Pneumonia (PCP) is one of the most common opportunistic lung infections that threat the life of AIDS patients (4). Vigilance for PCP, early diagnosis and early treatment are crucial to reduce the resulting mortality. In this study, the CT lung manifestations of 50 consecutive AIDS patients complicated with PCP were retrospectively analyzed. The chest imaging manifestation, and the correlation between imaging features, CD4+ lymphocyte count, and plasma virus load were investigated.
Materials and methods
Study subjects
Between March 2007 and July 2009, 50 consecutive AIDS patients complicated with PCP, who were all treated at the Shenzhen Third People’s Hospital, were retrospectively analyzed. There were 33 males and 17 females. The mean age was 34 years (age range, 19~57 years). All these patients were confirmed HIV positive by western blotting technique, and were classified as AIDS stage IV. Risk behaviors for HIV infection of these patients were as follow: sex contact 35, i.v. drug usage 7, blood transfusion 2, illegal blood sampling 1, unknown reason 5. The AIDS diagnosis was according to the Centers for Disease Control and Prevention of USA (5) and the Guidelines for diagnosis and treatment of HIV/AIDS in China (2005) (6). The criteria for the diagnosis of PCP include: (I) sputum, bronchoscopic biopsy or bronchoalveolar lavage tested Pneumocystis jirovecii postive; (II) consistent with diagnosis standards of AIDS or other severe immunosuppression; (III) CD4+ ≤200 /μL; (IV) dry cough, dyspnea, fever, chest pain or body weight loss, but without obvious chest sign; (V) typical chest X-ray characteristics; (VI) responsive to anti-PCP therapy; (VII) Serum lactate dehydrogenase (LDH) increase continuously by three consecutive testings. The diagnosis of AIDS complicated with PCP was made when a patient had the first item and any 4 items of the rest 6 items. Among these patients 3 cases had lung biopsy and the diagnosis was confirmed by Gomori methenamine silver staining. All these patients had various degrees of body weight loss. 34 patients had fever (range 37.2~39.5 ℃); 31 had dry cough; 3 had cough with sputum. 31 patients had short breath and progressive dyspnea. With auscultation, 29 cases had coarse breath sounds, 5 had interspersed fine moist crackles, and 1 had dry crackles in both upper lungs.
CD4+ T lymphocyte count and HIV virus load RNA Quantification
The percentage of CD4+ T lymphocytes in the peripheral blood was tested using Coulter Epics XL flow cytometry (FLM, Beckman Coulter Co. USA.) and triad-color fluorescence labeled monoclonal antibody kit (Immunotech Co. France). All the CD4+ T lymphocytes tests were carried out before or within one month after initial clinical diagnosis. HIV virus load was quantified in plasma by RT-PCR according to the manufacturer’s instruction (Amplicor HIV-1 Monitor test, Roche Diagnostic Systems, Madrid, Spain).
Chest CT examination and observation
All the patients underwent chest CT. The interval between the CD4+ T lymphocyte count and HIV virus load RNA quantification and CT examination was within 48 hours. Scan coverage was from the pulmonary apices to the diaphragm. Scan parameters included 120 kV, 200 mA, 10 mm collimation and 1.2 pitch. Lung parenchyma, as well as hilum and pleural space were inspected by two experienced radiologists, and consensus was reached in all cases.
Statistics analysis
All the data was analysed by the SPSS 11.13 statistics package. The logarithmic value of HIV virus load, mean and standard deviation (SD) of the CD4+ T lymphocyte count were evaluated. A P value less than 0.05 was considered statistically significant.
Results
Chest CT manifestations of PCP in AIDS patients
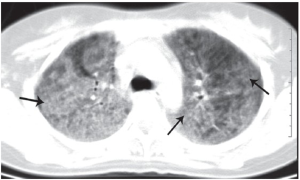
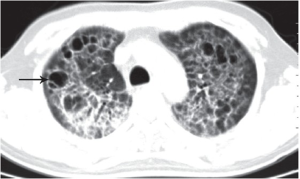
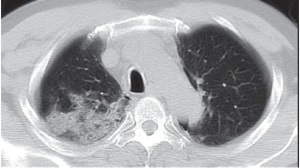
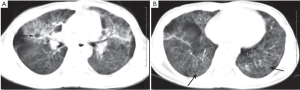
The imaging findings in our series of 50 cases included: (I) Ground-glass opacities dominated (Figure 1, 28/50, 56%), these patients often had extensive distribution in bilateral lungs (27 cases), with a predilection for the central and peihilar regions of the lungs. Aerial bronchogram was seen in some cases. In one case ground-glass opacities was limited to left lower lung. 13 cases had well defined crescent-shaped clear areas in subpleural region. (II) Lung cysts dominated (Figure 2, 10/50, 20%), lung cysts varied in appearance, with size ranging from 1.2 to 26 mm. Cysts tended to have thin wall, with inner and outer walls sharply defined. Around the lung cysts existed various extents of ground-glass opacities and patchy infiltrations. All these 10 cases had multiple lobes distribution, with 7 cases involved the upper lung lobes, and the remaining 3 cases involved all lobes of the lungs. (III) Consolidation dominated (Figure 3, 6/50, 12%), patchy consolidation presented with opacification of the parenchyma with obscuration of the underlying vessels. Aerial bronchogram was seen within consolidation. These consolidations occurred at pulmonary segments and subsegment level, with inhomogeneous density, and in bilateral lungs (5/50, 10%). In one case one solitary patchy shadow was observed on the upper lobe of right lung (1/50, 2%). (IV) Interstitial lesions dominated (3/50, 6%), lesions presented with coarsened pulmonary markings, reticular opacities and linear opacities in both lung fields, and thickened septal and subpleural lines. These lesions mostly had lower lobe distribution. There was one case had honeycombing pattern change and another case had diffuse interstitial fibrosis. (V) Mixed lesions pattern (Figure 4, 3/50, 6%), lesions presented with four types of above mentioned imaging findings. Overall, ground-glass opacities (28/50, 56%) and lung cysts (10/50, 20%) were the main image manifestations of PCP in AIDS patients.
Other imaging signs included mediastinal and hilar lymph node enlargement (17/50), which located predominantly in aortic-pulmonary window and behind the superior vena cava and upper carina, and minimal pleural effusion (bilateral in 4/50 and right sided in 2/50).
The correlation between chest CT features, CD4+ lymphocyte count, and Plasma HIV viral load
In the patients CD4+ lymphocyte count ranged from 2 cells/μL to 373 cells/μL. In 40 cases (80%) CD4+ lymphocyte count was less than 50 cells/μL; in 4 cases (8%) CD4+ lymphocyte count ranged from 50~100 cells/μL; in 3 cases (6%) CD4+ lymphocyte count ranged from 100~200 cells/μL; and in 3 cases (6%) CD4+ lymphocytes count was more than 200 cells/μL. Plasma HIV viral load ranged from 500~5.28×107 copies/mL (highest measureable value). Three cases (6%) were less than 103 copies/mL; 3 cases (6%) were 103 copies/mL; 8 cases (16%) were 104 copies/mL; 25 cases (50%) were 105 copies/mL; 9 cases (18%) were 106 copies/mL; and 2 cases (4%) were 107 copies/mL. CD4+ lymphocyte count and plasma HIV virus load of patients with different lung imaging manifestations are shown in Table 1. CD4+ lymphocyte count in ground-glass opacities dominated patients was higher than that of lung cyst dominated patients (P<0.05). Plasma virus load of lung cysts dominated PCP patients was higher than that of consolidation PCP patients (P<0.05).
| Table 1 CD4+ lymphocytes count and plasma virus load in 50 AIDS patients with PCP | |||||||
| Imaging classification | CD4+ lymphocyte count | Log HIV | Number of patients | ||||
| Mean±SD | Median(range) | Mean±SD | Median(range) | ||||
| ground-glass opacities dominated | 58±85 | 25(2-373) | 5.17±1.06 | 5.55(2.70-6.52) | 28 | ||
| lung cysts dominated | 12±12 | 6(2-36) | 6.01±0.90 | 5.76(5.04-7.72) | 10 | ||
| Consolidation dominated | 76±107 | 19(3-266) | 4.50±1.26 | 5.17(2.70-5.81) | 6 | ||
| interstitial lesion dominated | 15±11 | 15(4-25) | 5.66±0.24 | 5.91(5.42-5.91) | 3 | ||
| mixed lesions | 22±30 | 5(5-57) | 5.54±0.41 | 5.32(5.28-6.01) | 3 | ||
| total | 45±76 | 15(2-373) | 5.31±1.07 | 5.49(2.70-7.72) | 50 | ||
Discussion
The CD4+ T lymphocyte count is an explicit biomarker that provides assessment of immune system status of HIV-infected patients, while plasma HIV virus load reflects activity of HIV virus (7). PCP remains the most common and important complication of AIDS. Its occurrence and progress, and treatment response are closely related to the level of CD4+ lymphocyte count. Further investigation on PCP, particularly its imaging feature, and understanding the relation between PCP lung manifestations, CD4+ lymphocyte counts and HIV plasma viral load can be important.
In our series of 50 cases of PCP in AIDS patients, the chest CT manifestations in 28 (56%) were ground-glass opacities, presented with patchy and diffuse distribution in lobes and segments of lungs, and corresponded to early stage of pulmonary alveolus infiltration of Pneumocystis Jiroveci induced inflammation. Lung cysts of PCP in AIDS patients were once considered uncommon, however, with the increased detection sensitivity using modern imaging techniques such as helical high resolution CT, incidence rate of lung cyst in PCP was reported to be 10~34% (8,9), therefore now considered a typical manifestation of this infection. Our data showed the incidence rate of lung cyst was 20% (10/50), which agrees with literature data. In our study, lung cysts were of thin wall, inner and outer walls were sharply defined and there was no fluid in the cyst cavity. Cysts could be solitary, multiple or honeycomb appearance. Although an upper lobe predominance was seen, cysts could involve any portion of the lungs. They could also be found in either a subpleural or intraparenchymal location. Rupture of subpleural cysts may cause spontaneous pneumothorax. Identification of ground-glass opacities, lung cysts and spontaneous pneumothorax in AIDS patient are highly suggestive of PCP.
It is known that 90% of AIDS complicated PCP patients have CD4+ lymphocyte count below 200 cells/μL (10,11). As CD4+ lymphocyte count drops further, disseminated fungus and virus infections can occur. CD4+ lymphocyte counts <100 cells/μL is an important sign of disease further progression or deterioration. WHO recommended CD4+ lymphocyte count drop as an indicator of AIDS disease deterioration. In the meantime, plasma virus load is also directly related to decreased immune function and AIDS complications. In our series, 43 cases (43/50, 86%) had CD4+ lymphocyte count <100 /μL and were determined to be at advanced stage of AIDS disease. CD4+ lymphocyte cells count in ground-glass opacities pattern was higher than that of lung cysts pattern, with the difference reached statistical significance (P<0.05). The level of CD4+ lymphocyte count was relatively higher in ground-glass opacities dominated PCP patients, which suggested that they were in the relative early stage of the disease. Together with experimental biomarkers and clinical status, with ground-glass opacities dominated PCP patients, effective treatment may be installed. While CD4+ lymphocyte count in lung cysts dominated PCP patients and mixed lung patients were generally lower, suggesting severe compromised immune function of these patients, and these patients might have a longer disease course and poorer prognosis. Plasma virus load of lung cysts dominated PCP patients was generally higher, and that of consolidation PCP patients were relatively lower. Plasma virus load in lung cysts dominated patients and consolidation dominated patients groups had significant difference (P<0.05). CD4+ lymphocytes can be influenced by many factors including infection, complicated hepatic cirrhosis, and other diseases that may affect autoimmune system of the body. Therefore CD4+ T lymphocyte count is more likely to fluctuate, and some authors suggested that HIV virus load may be more accurate in reflecting clinical condition (12,13).
In conclusion, this current study suggested that ground-glass opacities and lung cysts are the main chest CT features of PCP in AIDS patients. CD4+ lymphocyte count in ground-glass opacities dominated patients is higher than that of lung cyst dominated patients. Plasma virus load of lung cysts dominated PCP patients is higher than that of consolidation PCP patients.
Acknowledgements
This study was supported by a grant from Science and Technology Funding projects of Shenzhen Health Bureau (No.200607).
Disclosure: The authors declare no conflict of interest.
References
- Onyancha OB, Ocholla DN. An informetric investigation of the relatedness of opportunistic infections to HIV/AID. Inform Proc Manag 2005;41;1573-88.
- Pachl C, Todd JA, Kern DG, et al. Rapid and precise quantification of HIV-1 RNA in plasma using a branched DNA signal amplification assay. J Acquir Immune Defic Syndr Hum Retrovirol 1995;8:446-54.
- Mellors JW, Muñoz A, Giorgi JV, et al. Plasma viral load and CD4+ lymphocytes as prognostic markers of HIV-1 infection. Ann Intern Med 1997;126:946-54.
- Lu PX, Yang GD, Liu JQ, et al. Imaging Diagnosis of Pneumocystis Carinii Pneumonia in Patients with Acquired Immunodeficiency Syndrome. Chinese J Med Imaging 2003;11:166-8.
- 1993 revised classification system for HIV infection and expanded surveillance case definition for AIDS among adolescents and adults. MMWR Recomm Rep 1992;41:1-19.
- Chinese Medical Association; Chinese Center for Disease Control and Prevention. Guidelines for diagnosis and treatment of HIV/AIDS in China (2005). Chin Med J (Engl) 2006;119:1589-608.
- Chin JW, Grotzfeld RM, Fabian MA, et al. Methodology for optimizing functional miniature proteins based on avian pancreatic polypeptide using phage display. Bioorg Med Chem Lett 2001;11:1501-5.
- Lipkens B, Blackstock DT. Model experiment to study sonic boom propagation through turbulence. Part II. Effect of turbulence intensity and propagation distance through turbulence. J Acoust Soc Am 1998;104:1301-9.
- Lee SA. A Review of Pneumocystis Pneumonia. Journal of Pharmacy Practice 2006;19;5-9.
- Hartman TE, Primack SL, Müller NL, et al. Diagnosis of thoracic complications in AIDS: accuracy of CT. AJR Am J Roentgenol 1994;162:547-53.
- Tokuda H, Sakai F, Yamada H, et al. Clinical and radiological features of Pneumocystis pneumonia in patients with rheumatoid arthritis, in comparison with methotrexate pneumonitis and Pneumocystis pneumonia in acquired immunodeficiency syndrome: a multicenter study. Intern Med 2008;47:915-23.
- Beck EJ, Kupek EJ, Gompels MM, et al. Correlation between total and CD4 lymphocyte counts in HIV infection: not making the good an enemy of the not so perfect. Int J STD AIDS 1996;7:422-8.
- Stebbing J, Sawleshwarkar S, Michailidis C, et al. Assessment of the efficacy of total lymphocyte counts as predictors of AIDS defining infections in HIV-1 infected people. Postgrad Med J 2005;81:586-8.


