Massive alveolar haemorrhage: a rare life threatening complication of Wegener’s granulomatosis—report of a rare case
Introduction
Wegener’s granulomatosis (WG) is a multisystem necrotising granulomatous vasculitis affecting small vessels. Diffuse alveolar haemorrhage (DAH) is its rare fatal complication which sometimes can also be the earliest manifestation of this disease and prompt accurate diagnosis with immediate aggressive treatment with cyclophosphamide is essential to improve outcome. Approximately 41 cases have been reported so far of this rare complication (1). We report a similar case of DAH who was later found to be positive for c-antineutrophil cytoplasmic antibodies (c-ANCA) and had evidence of pansinusitis and therefore diagnosed as WG and treated aggressively with pulse steroids and cyclophosphamide.
Case report
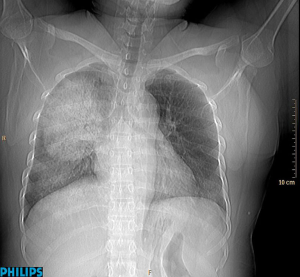
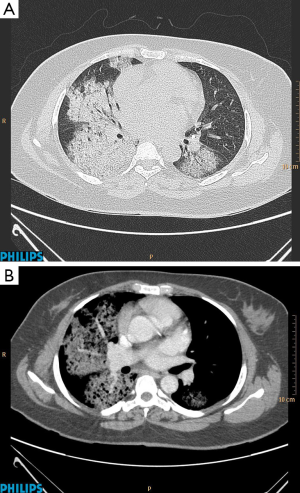
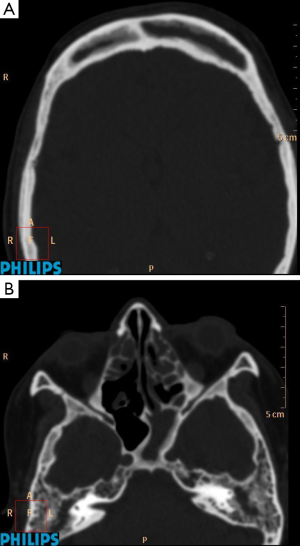
A 45-year-old woman, asymptomatic previously presented with massive haemoptysis and sudden onset of dyspnoea in accident and emergency department. Patient was haemodynamically stable. Plain radiograph of chest frontal view (Figure 1) was done which showed dense alveolar opacification in right upper and mid zone and left lower zone. Contrast enhanced computed tomography (CECT) of chest was then advised for the patient. Diffuse dense areas of consolidation with air bronchograms were seen in right lung and left lower lobe of lung along with areas of ground glass shadowing on the right side (Figure 2A,B). No other positive finding was seen. A diagnosis of DAH was made and patient was further investigated for his coagulation profile and serologically for antinuclear antibodies, c-ANCA and anti-GBM titres. Patient was positive for c-ANCA and detailed history also showed symptoms of sinusitis. A diagnosis of WG was made and patient was treated with high dose steroids and cyclophosphamide. Computed tomography (CT) of paranasal sinuses was also done subsequently and showed evidence of pansinusitis (Figure 3A,B). Symptoms improved gradually over a period of 2 weeks.
Discussion
WG is a small vessel vasculitis and was described by German pathologist Freidrich Wegener in 1939. It is a multisystem disease. Though most commonly lungs (90%) and kidneys (71%) are involved, involvement of joints, eyes, and paranasal sinuses is not uncommon (2). Various manifestations of WG are sinusitis (51%), nasal congestion and epistaxis (36%), conjunctivitis with episcleritis (6%), frank arthritis (32%) and purpuric rash (13%). DAH leading to ARDS is a rare manifestation of disease. Overall 41 cases have been reported so far.
DAH is a rare fatal syndrome and can be manifestation of variety of diseases. The disorders that can cause alveolar hemorrhage include autoimmune diseases (WG, Good Pasteur’s syndrome, SLE, Antiphospholipid antibody syndrome), pulmonary infections (invasive aspergillosis, hantavirus), cardiac disorders (mitral stenosis), coagulation disorders, bone marrow/solid organ transplantation, toxic exposures, drug reactions (amiodarone, methotrexate etc.) and idiopathic pulmonary haemosiderosis. In addition to hemoptysis other clinical features of underlying etiological disorder e.g., haematuria and sinusitis in WG, fever in SLE should be asked for. Chest radiograph and chest CT scan should be done in these patients to look for associated features of various diseases like cavitating nodules in WG apart from alveolar haemorrhage (3).
Regardless of associated symptoms patients with DAH patients should be serologically tested for c-ANCA, p-ANCA, proteinase-3 (PR3), anti-GBM titres, rheumatoid factor (RF), antinuclear antibodies (ANA), complete haematological profile, erythrocyte sedimentation rate (ESR) and urine analysis. The presence of c-ANCA, PR3 antibodies, ANA, p-ANCA, anti-GBM titres with negative RF are diagnostic of WG. Other findings can be anaemia, thrombocytosis, raised ESR, proteinuria, haematuria, raised blood urea nitrogen and serum creatinine. Presence of c-ANCA has sensitivity and specificity of 81% and 99.5% respectively for WG. Combining PR3 and c-ANCA increases specificity close to 100% and reduces sensitivity to 70% (3-5). Lung biopsy, which lacks sensitivity and specificity, is not required in patients of DAH with positive c-ANCA and these patients should be started with early and aggressive treatment with cyclophosphamide and prednisolone. This is due to the fact that patients with ANCA positive vasculitis with DAH have six times higher mortality rate than patients of WG who don’t have alveolar hemorrhage, but early accurate diagnosis with immediate treatment has shown significant reduction in mortality rate (3).
Conclusions
WG should be excluded as possible cause in patients presenting with alveolar hemorrhage with or without glomerulonephritis, and these patients should be evaluated serologically for c-ANCA without the need for histological confirmation. Immediate and aggressive treatment with pulse steroids and high dose cyclophosphamide should be initiated in ANCA positive patients, which significantly reduces mortality and induces remission.
Disclosure: The author declares no conflict of interest.
References
- Schwarz MI, Brown KK. Small vessel vasculitis of the lung. Thorax 2000;55:502-10. [PubMed]
- Cardenas-Garcia J, Farmakiotis D, Baldovino BP, Kim P. Wegener’s granulomatosis in a middle aged woman presenting with dyspnoea,rash, hemoptysis and recurrent eye complaints: a case report. J Med Case Rep 2012;6:335. [PubMed]
- Ioachimescu OC, Stoller JK. Diffuse alveolar hemorrhage: diagnosing it and finding the cause. Cleve Clin J Med 2008;75:258-260, 264-5 passim. [PubMed]
- Lin Y, Zheng W, Tian X, Zhang X, Zhang F, Dong Y. Antineutrophil cytoplasmic antibody associated vasculitis complicated with diffuse alveolar hemorrhage: a study of 12 cases. J Clin Rheumatol 2009;15:341-4. [PubMed]
- Thickett DR, Richter AG, Nathani N, Perkins GD, Harper L. Pulmonary manifestations of antineutrophil cytoplasmic antibody (ANCA) positive vasculitis. Rheumatology (Oxford) 2006;45:261-8. [PubMed]


