
Pseudoaneurysm of superior thyroid artery following ultrasound-guided radiofrequency ablation of hyperplastic parathyroid gland: a case report and literature review
Introduction
Dr. Carrafiello and associates reported the successful treatment of secondary hyperparathyroidism by radiofrequency ablation (RFA) in 2006 (1). In recent years, ultrasound-guided percutaneous thermal ablation of hyperplastic parathyroid gland has proven to be an effective method for the treatment of secondary hyperparathyroidism (2-5). Complications of this treatment include cervical nerve injury, neck hematoma (4,5). We report a case of a superior thyroid artery pseudoaneurysm following ultrasound-guided RFA of hyperplastic parathyroid gland for the treatment of secondary hyperparathyroidism.
Case presentation
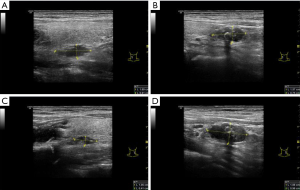
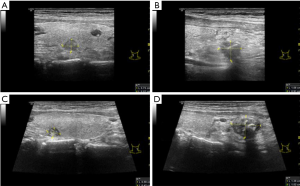
A 36-year-old man with advanced chronic renal disease had been undergoing hemodialysis treatment three times a week for 11 years. In the past 1 year, his parathyroid hormone continued to rise, reaching ≥2,000 pg/L. This patient had the following symptoms: dry mouth, fatigue, lumbar acid, knee pain, hearing loss, occasional blurred vision. He was given him of Rocaltrol and Cinacalcet for treatment, but the curative effect was poor, and the reduction of parathyroid hormone levels was not obvious after repeated examinations. Ultrasonographic image showed that four parathyroid glands in the bilateral neck were hypertrophic and hypoechoic with calcification. The size of the upper and lower parathyroid glands in the left neck was about 1.1×0.4, 1.9×1.0 cm, and that of the upper and lower parathyroid glands in the right neck was about 1.7×0.6, 1.6×0.8 cm (Figure 1).
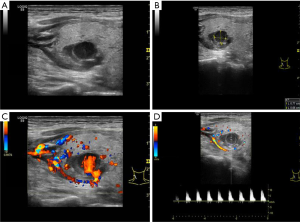
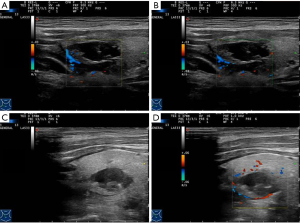
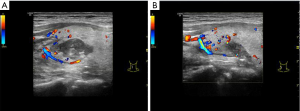
After communicating with the patient fully, we performed ultrasound-guided RFA. Heparin was not used in hemodialysis the day before RFA. RFA was done with a radiofrequency generator (VIVA; STARmed, Goyang, Korea) along with an 18-gauge-0.7 cm monopolar internally cooled electrode on the left two hyperplastic parathyroid glands on January 21, 2019. For this session of RFA treatment, the RF power was 35 W, and the cumulative ablation time was 90 seconds. After the first ablation, the patient had no complications except for mild neck pain for about 3 days, while his parathyroid hormone levels decreased to about 1,100 pg/L. Then we performed ultrasound-guided RFA using the same RF device as the first time on the right two hyperplastic parathyroid glands on February 24, 2019. For this session of RFA treatment, the RF power was 35 W, and the cumulative ablation time was 110 seconds. One day after this second ablation, a pseudoaneurysm of the superior thyroid artery in the right neck of the patient was found by ultrasonography (US). The size of the pseudoaneurysm was about 0.8×0.7 cm (Figure 2). Immediately we took a partial compression treatment on the pseudoaneurysm for 30 minutes under ultrasound monitoring, and then the pseudoaneurysm was found closed and hypoechoic thrombosis formed in the lumen of the aneurysm (Figure 3). One day after partial compression treatment, the ultrasound imaging indicated that the pseudoaneurysm turned into a hematoma with about 1.8×0.9 cm in size. After 1 month, the hematoma size was further reduced, and the size was about 1.2×0.6 cm (Figure 4). In addition, 1 month after two ablation treatments, the parathyroid hormone of the patient decreased to about 120 pg/L, and the volume of four parathyroids also decreased significantly (Figure 5).
We conducted a systematic review searching database PubMed, Embase and Web of Science from inception to April 2019. The base characteristics of the 14 included cases from 7 articles were shown in Table 1 (6-12). There were 8 (57.1%) women and 6 (42.9%) men varying in age from 50 to 72 years. Of these cases, 10 developed pseudoaneurysm shortly or years after US-guided biopsy of thyroid lesions, who finally were treated by receiving RFA or surgery (6,7,9). Other four cases developing pseudoaneurysm underwent coil embolization and resolved (8,10-12).
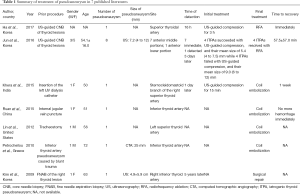
Full table
Discussion
Ablation of hyperparathyroidism and thyroid nodule has been widely used in clinical practice in recent years, especially in Asian countries such as China. Ablation includes RFA, microwave ablation and laser ablation. There is no significant difference of these methods in the efficacy of thyroid nodule ablation (13-15). However, because RFA electrode is sharper than microwave antenna and laser fiber, and the percutaneous puncture operation is more convenient. RFA was selected in this case. The majority of benign thyroid nodules are asymptomatic, remain stable in size, and do not require treatment. However, a minority of patients with growing nodules may have local symptoms or cosmetic concerns, and thus demand RFA or surgical therapy (16). The main purpose of RFA for hyperparathyroidism caused by primary or secondary hyperparathyroidism is to inactivate parts of the parathyroid tissue, making the parathyroid gland shrink and finally reducing the parathyroid hormone, so to reduce clinical symptoms caused by the increase of parathyroid hormone.
Hyperparathyroidism RFA can be completed under the guidance of ultrasound. It is desirable that four hyperplastic parathyroids can be clearly displayed on ultrasound, or a single-gland adenoma become an indication for RFA treatment. Postsurgical recurrent hyperparathyroidism may be a good indication due to difficulty in reoperation (17). RFA of hyperparathyroidism is usually performed under local anesthesia. Compared with surgery, RFA is more minimally invasive, with lower risk and fewer complications. The main complications reported in the literature include cervical nerve injury, neck hematoma, while no paper reports cervical pseudoaneurysms. Our case of pseudoaneurysm was found 1 day after ultrasound-guided RFA of parathyroid gland. The fundamental cause of the formation of pseudoaneurysms would be vascular injury. The formation of pseudoaneurysm in our case may be related to the following factors: (I) the right upper parathyroid gland is adjacent to the posterior branch of the right superior thyroid artery. During RFA, the posterior branch of the right superior thyroid artery could be injured by puncture of the ablation needle; (II) the posterior branch of the superior thyroid artery was too deep, and the pressure hemostasis of the neck was ineffective after ablation; (III) the arterial wall of the patient could be fragile due to chronic kidney disease for 11 years. In addition, the patient underwent hemodialysis treatment with heparin intermittently.
In our case, the pseudoaneurysm of the posterior branch of the superior thyroid artery in the right neck was successfully treated with ultrasound-guided local compression. The steps of treatment in this case were: (I) hemodialysis without heparin before treatment; (II) full-range monitoring with color Doppler ultrasound; (III) local compression with high frequency linear array probe, which was placed on the center of the pseudoaneurysm passage in the right neck of the patient, and moderately compressed to flatten the aneurysm chamber to stope blood flow signal; (IV) after 30 minutes of continuous compression, the hypoechoic thrombosis was observed in the lumen of the tumor after slow decompression, and then gauze and bandage were used for moderate pressure dressing for additional 24 hours.
In 1991, Fellmeth et al. (18) first reported the compression therapy of pseudoaneurysm under the guidance of ultrasound. Four iatrogenic thyroid pseudoaneurysms (ITPAs) were treated with US-guided compression and their mean size was 5.4 (4 to 7.5) mm; while 4 ITPAs failed with US-guided compression and their mean size was 9.0 (6 to 12) mm (7).
In conclusion, we report a case of pseudoaneurysm of the superior thyroid artery due to ultrasound-guided RFA of hyperplastic parathyroid gland in a patient with chronic kidney disease. We used a partial compression therapy under ultrasound monitoring to treat this pseudoaneurysm successfully.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/qims.2020.03.06). The authors have no conflicts of interest to declare.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Carrafiello G, Laganà D, Mangini M, Dionigi G, Rovera F, Carcano G, Cuffari S, Fugazzola C. Treatment of secondary hyperparathyroidism with ultrasonographically guided percutaneous radiofrequency thermoablation. Surg Laparosc Endosc Percutan Tech 2006;16:112-6. [Crossref] [PubMed]
- Zhao J, Qian L, Zu Y, Wei Y, Hu X. Efficacy of ablation therapy for secondary hyperparathyroidism by ultrasound guided percutaneous thermoablation. Ultrasound Med Biol 2016;42:1058-65. [Crossref] [PubMed]
- Zhuo L, Peng LL, Zhang YM, Xu ZH, Zou GM, Wang X, Li WG, Lu MD, Yu MA. US-guided microwave ablation of hyperplastic parathyroid glands: safety and efficacy in patients with end-stage renal disease-a pilot study. Radiology 2017;282:576-84. [Crossref] [PubMed]
- Zhuo L, Zhang L, Peng LL, Yang Y, Lu HT, Chen DP, Li WG, Yu MA. Microwave ablation of hyperplastic parathyroid glands is a treatment option for end-stage renal disease patients ineligible for surgical resection. Int J Hyperthermia 2019;36:29-35. [Crossref] [PubMed]
- Peng C, Zhang Z, Liu J, Chen H, Tu X, Hu R, Ni J, Weng N, Pang H, Xue Z. Efficacy and safety of ultrasound-guided radiofrequency ablation of hyperplastic parathyroid gland for secondary hyperparathyroidism associated with chronic kidney disease. Head Neck 2017;39:564-71. [Crossref] [PubMed]
- Ha EJ, Baek JH, Lee JH, Kim JK, Choi YJ, Sung TY, Kim TY. Complications following US-guided core-needle biopsy for thyroid lesions: a retrospective study of 6,169 consecutive patients with 6,687 thyroid nodules. Eur Radiol 2017;27:1186-94. [Crossref] [PubMed]
- Jun YK, Jung SL, Byun HK, Baek JH, Sung JY, Sim JS. Radiofrequency ablation for iatrogenic thyroid artery pseudoaneurysm: initial experience. J Vasc Interv Radiol 2016;27:1613-7. [Crossref] [PubMed]
- Khera PS, Moses V, Ahmed M, Kakde S. Superior thyroid artery pseudoaneurysm and arteriovenous fistula following attempted internal jugular venous access and its management. Indian J Radiol Imaging 2015;25:15-7. [Crossref] [PubMed]
- Kim HS, Kim J, Kim EY, Lee SK, Kim DI, Chung WY. Pseudoaneurysm of the inferior thyroid artery presenting as a thyroid nodule. Thyroid 2009;19:69-71. [Crossref] [PubMed]
- Lin HW, Reilly BK. Pseudoaneurysm of the superior thyroid artery following revision tracheostomy. Laryngoscope 2012;122:1641-3. [Crossref] [PubMed]
- Petrocheilou G, Myrianthefs P, Evodia E, Vlychou M, Kokkinis CE. Inferior thyroid artery pseudoaneurysm caused by blunt trauma. Vascular 2010;18:242-5. [Crossref] [PubMed]
- Ruan J, Zhang C, Peng Z, Tang DY, Feng Z. Inferior thyroid artery pseudoaneurysm associated with internal jugular vein puncture: a case report. BMC Anesthesiol 2015;15:71. [Crossref] [PubMed]
- Mainini AP, Monaco C, Pescatori LC, De Angelis C, Sardanelli F, Sconfienza LM, Mauri G. Image-guided thermal ablation of benign thyroid nodules. J Ultrasound 2016;20:11-22. [Crossref] [PubMed]
- Tong M, Li S, Li Y, Li Y, Feng Y, Che Y. Efficacy and safety of radiofrequency, microwave and laser ablation for treating papillary thyroid microcarcinoma: a systematic review and meta-analysis. Int J Hyperthermia 2019;36:1278-86. [Crossref] [PubMed]
- Choi Y, Jung SL. Efficacy and safety of thermal ablation techniques for the treatment of primary papillary thyroid microcarcinoma: a systematic review and meta-analysis. Thyroid 2020. Epub ahead of print. [Crossref] [PubMed]
- Cesareo R, Palermo A, Pasqualini V, Cianni R, Gaspa G, Manfrini S, Pacella CM. Radiofrequency ablation for the management of thyroid nodules: a critical appraisal of the literature. Clin Endocrinol (Oxf) 2017;87:639-48. [Crossref] [PubMed]
- Machi J. Radiofrequency ablation for hyperparathyroidism: can it be a new treatment? Surg Laparosc Endosc Percutan Tech 2006;16:116. [Crossref] [PubMed]
- Fellmeth BD, Roberts AC, Bookstein JJ, Freischlag JA, Forsythe JR, Buckner NK, Hye RJ. Postangiographic femoral artery injuries: nonsurgical repair with US-guided compression. Radiology 1991;178:671-5. [Crossref] [PubMed]


