Concurrent central odontogenic fibroma (WHO Type) and traumatic bone cyst: report of a rare case
Introduction
The central odontogenic fibroma (COF) was introduced into the World Health Organisation (WHO) classification of odontogenic tumors in 1971 (1). Thereafter, further attempts were contemplated to simplify and classify this tumor. Wesley et al. 1975 and Gardner in 1980 attempted to clarify the diagnostic criteria of COF. However, COF still remains somewhat controversial, causing confusion due to its nature and definition. Even the 2005 WHO definition cannot specifically distinguish COF from other similar lesions (1,2).
COF is a slow and persistent growing benign odontogenic tumor with 2.8:1 female predilection (1,3). Clinically, it ranges from patients among the second and sixth decade of life (mean 40 years). Lesions are similarly found in maxilla and mandible (2,3). It tends to manifest as an asymptomatic swelling although larger lesions can appear in a more aggressive way provoking pain, localized bony expansion, loosening of teeth, dental displacement and rhizolysis (1,2). It is a rare tumor representing less than 1.5% of all odontogenic tumors (2). Histologically, it is defined as fibroblastic neoplasia that ranges from poorly cellular and myxoid without significant odontogenic epithelial component, to cellular with abundant odontogenic epithelium and occasional foci of calcifications. The terms simple (epithelium-poor) type and complex or WHO (epithelium-rich) type, have been, respectively, designated to those lesions (1).
A traumatic bone cyst (TBC) is a pathological bone cavity of complex etiology (4). TBC was first described in 1929 by Lucas and Blum as a separate disease entity. Rushton in 1946 elaborated the diagnostic criteria of this cyst (5). TBC is classified by the World Health Organization as a non-neoplastic lesion related to bone, and is grouped together with the ossifying fibroma, fibrous dysplasia of bone, central giant cell lesions, aneurysmatic bone cysts, and cherubism. It is defined as “an intraosseous cyst having a tenuous lining of connective tissue with no epithelium” (6,7). Apart from the term TBC, these have been referred to in different ways: hemorrhagic bone cyst, simple bone cyst, hemorrhagic TBC, progressive bone cavity, unicameral bone cyst, extravasation cyst, and idiopathic bone cavity (4). Various causal factors have been proposed for the pathogenesis of the TBC. The myriad of different proposed mechanisms and multiple terminologies provide some insight that the underlying etiopathogenesis is still not clear (5).
TBCs are rare lesions, accounting for 1% of all jaw cysts, commonly found in the metaphysis of long bones (6,7). Facial TBCs are considered almost exclusively mandibular lesions, with a preference for the posterior areas (angulus-ramus). Rarely, they may be found in maxilla and are mainly located in the frontal part (4). A higher prevalence is noted in young patients (approximate mean age of 20 years), and it is rarely diagnosed after 25 years of age. The cysts tend to be asymptomatic, being accidentally diagnosed in routine radiographic studies. It classically presents as a well-defined unilocular radiolucent lesion in the posterior portion of the mandible, often having characteristic scalloped superior margin extending between the roots of teeth (5,7). Histopathology reveals absence of an epithelial lining, characteristic of pseudocysts. A final diagnosis of a TBC is almost invariably made at the time of surgery; wherein identification of an empty air-filled cavity serves as a valuable diagnostic tool (6).
The purpose of this report is to present a rare case of co-occurrence of COF (WHO type) with simple bone cyst in a young Asian woman. A thorough search of literature had revealed that no such co-occurrence has been reported. In addition, we discuss relevant issues about the origin, diagnosis and management of these lesions.
Case report
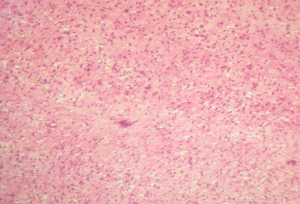
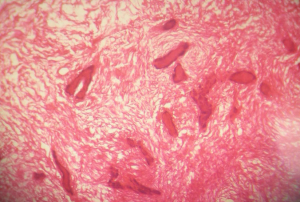
An 18-year-old female presented with a painless gingival swelling in the area of the maxillary right third molar. The patient reported slow growth of the lesion during the last two months, with moderate discomfort during mastication as the only relevant symptom. Her medical and surgical history was noncontributory. The extraoral examination showed swelling on the right cheek causing some facial asymmetry. The intraoral examination revealed a 2 cm sessile tumor on the right side of the maxillary alveolar ridge, posterior to the first molar (Figure 1). There was no relevant mobility of the teeth in the area, which were positive to thermal testing; percussion and palpation tests were within normal limits. The lesion had a firm consistency and was covered by a normal overlying mucosa. There were no clinical signs of inflammation in spite of surface indentations caused by their opposing mandibular teeth. Radiographic evaluation showed the presence of a solitary mixed radiolucent radiopaque lesion with partially ill-defined borders and with epicenter coronal to impacted maxillary right third molar. It caused a superior displacement of the tooth. There was no evidence of rhizolysis of adjacent teeth. Incidentally, a unilocular radiolucent lesion with well corticated border involving the left angle and body of the mandible was found (Figure 2). The lower left first, second, third molars and second premolar were involved but were sound and vital. The lesion extended up to the lower border of mandible and marginal scalloping was noted. The lesion had been asymptomatic. Computed Tomographic examination (Figure 3) showed a large expansile lesion with complex attenuation involving the entire right maxilla, measuring around 4.4 cm × 3.4 cm × 3.0 cm. A retained molar tooth near the floor of the orbit was also noted. Floor of the maxilla was eroded by the lesion. It also revealed a well-defined predominantly cystic lesion in the left mandible, measuring 1.5 cm × 1.8 cm × 2.3 cm with sclerotic rim and cortical scalloping. Histopathological examination revealed a hypercellular fibroblastic proliferation in a mature collagenous stroma (Figure 4) showing inactive appearing odontogenic epithelial islands throughout the lesion (Figure 5). Focal areas of calcification resembling cemento-osseous material are evident interspersed between the epithelial cells (Figure 5). Correlation of clinical, radiographic and histopathological features confirmed the diagnosis of COF, and it was subclassified as epithelium rich (WHO) type. The lesion was then entirely removed by curettage under general anesthesia. Surgical exploration revealed an empty cavity in the left mandible, confirming the diagnosis of TBC. The cavity was curetted. The case was followed with no signs of recurrence after two and a half year, and the lesions appeared to be healing well.



Discussion
Intra-osseous fibromas are rare, and can be further classified depending on the presence or absence of odontogenic epithelium into odontogenic fibroma or non-odontogenic (desmoplastic) fibroma (8). COF is considered to be derived from the dental mesenchymal tissues (dental papilla, periodontal ligament, or dental follicle), and therefore is invariably related to the coronal or radicular portion of teeth. The epithelial component has been described as inactive looking (3,9). It is believed that the epithelium poor type of COF is derived from the dental follicle, whereas the epithelium-rich type arises from the periodontal ligament (10).
Clinically, this indolent tumor usually evolves asymptomatically. Radiologically, they commonly present as unilocular or multilocular radiolucencies (10,11). The radiographic presentation seemingly depends on the dimension of the lesion, small fibromas (about 2 cm) having a unilocular appearance, whereas large lesions (about 4 cm) showing multilocularity. Thus, the multilocular lesions are more likely to be associated with complications such as root resorption of adjacent teeth, teeth displacement and expansion of the cortical bones (1,12). Radiological presentation of our case was significantly different from the classical descriptions. It exhibited a mixed radiolucent-radiopaque appearance with poorly defined borders, which indeed is a rare presentation (10). Even though the size of the lesion was large (>4 cm), it did not provoke any significant complication. Our patient claimed the lesion after two months, complaining only the discomfort caused by that mass, without mobility or pain. The only significant complication was the erosion of the floor of the maxillary sinus, as evident on the CT scan. Radiological diagnosis of the lesion is extremely difficult, which was further complicated in our case due to its association with the unerupted maxillary right third molar, wherein it resembled a dentigerous cyst (10). Histologically, in addition to two main subtypes (simple type and complex type), COF has following variants: granular cell, pleomorphic fibroblast and giant cell granuloma-like variants (2). Our case was compatible with odontogenic fibroma complex (WHO) type. Presently, COF is considered to be a rare odontogenic tumor with only 70 reported cases in the literature. Not long ago, however, it was considered to be one of the most common odontogenic tumors due to incorrect diagnosis of dental follicle as COF (1). Due to its non-exclusive histological features, coupled with great variability of clinical and radiological characteristics, wide range of pathosis should be considered to make a safe diagnosis. At the same time, its correct histologic identification is necessary to avoid the diagnostic pitfall of overdiagnosis of similar-appearing follicular sacs and dental pulps (13). Differential diagnosis includes ameloblastoma ameoloblastic fibroma, odontogenic myxoma, desmoplastic fibroma, calcifying odontogenic cysts, follicular cysts, juvenile aggressive fibromatosis or fibrosarcoma (3,10). This highlights the importance of clinicopathological as well as radiological correlation in the correct diagnosis of odontogenic fibromas. Diagnosis of COF should be well conducted because different surgical approach may be required for other similar appearing lesions. COF is a benign tumor and responds well to surgical curettage with no malignant transformation potential. It is usually easily removed, not showing any adherence to bone and/or to tooth structure (2). Lesions like myxoma, desmoplastic fibroma and ameloblastic fibroma have shown recurrence tendency, thus necessitating a more aggressive surgical approach (3). Rare cases of COF recurrence have been reported, which gets identified only after several years due to their benign slow growth characteristics. The recurrences are mostly related to insufficient curettage and not to the histological type (1,12).
TBC is an interesting lesion which has been coined differently by many authors. For lesions affecting the jaws, terms like TBC, hemorrhagic cyst or extravasation cyst are widely used whereas extragnathic lesions are termed as solitary bone cyst or unicameral cyst. This multiplicity in names is indicative of the divergent views regarding its pathogenesis (14). Traumatic-hemorrhagic theory is the most widely accepted theory, although many other possible causes and mechanisms have been discussed in the literature. The major difficulty with this theory however, is the absence of a clear history of orofacial traumatism in many cases, as seen in the present case (6). Furthermore, the incidence of trauma in TBC patients is no greater than in the general population (15). This traditional view and the importance of trauma in the development of TBCs may thus appear questionable. The recent orthopedic literature review has suggested venous obstruction and blockage of interstitial fluid drainage, in an area of rapidly growing and remodelling cancellous bone may be the cause of all forms of simple bone cyst (7). However, there is still no definitive evidence available that could explain the formation of these lesions, and its etiology remains obscure. Its correct diagnosis and treatment may help to elucidate the pathophysiology, which relies on clinical, radiographic, and ultimately, surgical findings (15).
TBC occurs frequently in the posterior mandible, which could explain the trauma-hemorrhage theory. The reason for lesser incidence of maxillary lesions may be the presence of maxillary sinus, making radiographic visualization of this asymptomatic lesion inherently more difficult. Clinically, they are usually asymptomatic and appear as casual findings on routine radiographies. It is in stark contrast to orthopedic TBCs, 80% of which are discovered following pathologic fracture. This may be due to the fact that asymptomatic long bones in children do not routinely undergo radiography, unlike the annual dental radiographic screenings (15). Rarely, TBC can cause fracture of the mandible (4). Characteristically, TBCs present as radiolucent areas on the radiograph. This radiographic pattern may vary, which includes multilocular presentation, association with impacted teeth, and multiple occurrences in the same patient (6). Usually, computed tomography and magnetic resonance imaging are not required for diagnosis of jaw TBCs. Unusual radiographic features, however, may warrant these advanced imaging techniques for further evaluation (15,16). Most cases of TBCs are noted in young patients, where they present with classic clinical and radiographic features. Variations from these classic descriptions occur more often in patients of the older age group (7). Reduced prevalence of TBCs in older age group has led to the speculation that this lesion may be self-repairing (6). However, considering the possibility of a diagnostic error, an expectant approach to management is not recommended. Moreover, it may lead to complications such as pathological mandibular fracture. The treatment of choice for TBC is careful curettage of the lesion which favors progressive bone regeneration after formation of a stable blood clot, offering a good prognosis (5). Recurrences are rare, and usually occur within three months of surgery. Thus, follow-up examinations should be carried out at short intervals in the early period after surgery (7). Other treatment options only would be justified in cases of relapse. Alternate treatment options such as filling of the cavity with bovine lyophilized bone or the introduction of autologous blood with bone from the patient or hydroxyapatite may be particularly useful when osseointegrated implant rehabilitation of the affected zone is considered. However, diagnosis of possible lesion relapse may get complicated due to radiopaque materials in the cavity (5). Recurrence rates are higher in the cases of multiple cysts or those associated with florid cemento-osseous dysplasia (6,7). Intralesional injection of methylprednisolone has been described as a treatment modality for TBCs in the long bones. Corticosteroid has a complex mechanism of action, with both anti-inflammatory properties and significant attenuation of cellular metabolism. The use of corticosteroid injection for jaw TBCs may warrant further evaluation, which would greatly simplify the current approach to this lesion (15). A final diagnosis of a TBC is almost invariably made at the time of surgery, during which empty bone cavity is usually found. Thus, identification of an empty air-filled cavity on aspiration may serve as a valuable diagnostic tool. Originally though, this cyst was identified by the presence of clear cystic fluid at surgery. The reasons for this apparent dichotomy are unclear, although it has been speculated that this may simply represent different stages in cyst development (6,15). Adequate diagnosis and treatment of TBCs are complicated by the broad palette of other pathological processes in the area of the jaw. Because of a lack of unique clinical and radiographic features, it is important to establish the differential diagnosis between TBCs and other radiolucent lesions of the jaws. The authors believe that the possibility of unusual radiographic and clinical presentation should be kept in mind when formulating the differential diagnosis. For differential diagnostics the following can be considered: dentigerous cysts, keratocystic odontogenic tumors, ameloblastomas, odontogenic myxomas, aneurysmatic bone cysts, calcifying epithelialodontogenic tumor, adenomatoid odontogenic tumor, focal osteoporotic bone marrow defect, intraosseous vascular malformations, central giant cell lesions, early stage of cementoma (periapical cemental dysplasia), fibrous dysplasia and cherubism, among others (4,7).
COF and TBC are two independent disease processes that run entirely different courses with varying treatment options and differing prognosis. These two distinctively different lesions occurring simultaneously in the same patient are exceptionally rare and never reported in literature. In summary, the authors have presented an unusual case of non-syndromic coincidental co-occurrence of COF (WHO type) and TBC in a young patient. Current knowledge regarding the concept, pathophysiology and diagnosis of these lesions, which still remain a matter of debate, are reviewed.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Hrichi R, Gargallo-Albiol J, Berini-Aytés L, et al. Central odontogenic fibroma: retrospective study of 8 clinical cases. Med Oral Patol Oral Cir Bucal 2012;17:e50-5. [PubMed]
- Younis RH, Scheper MA, Lindquist CC, et al. Hybrid central odontogenic fibroma with giant cell granuloma-like component: case report and review of literature. Head Neck Pathol 2008;2:222-6. [PubMed]
- Brazão-Silva MT, Fernandes AV, Durighetto-Júnior AF, et al. Central odontogenic fibroma: a case report with long-term follow-up. Head Face Med 2010;6:20. [PubMed]
- Kim KA, Koh KJ. Recurrent simple bone cyst of the mandibular condyle: a case report. Imaging Sci Dent 2013;43:49-53. [PubMed]
- Cortell-Ballester I, Figueiredo R, Berini-Aytés L, et al. Traumatic bone cyst: a retrospective study of 21 cases. Med Oral Patol Oral Cir Bucal 2009;14:E239-43. [PubMed]
- Martins-Filho PR, Santos Tde S, Araújo VL, et al. Traumatic bone cyst of the mandible: a review of 26 cases. Braz J Otorhinolaryngol 2012;78:16-21. [PubMed]
- Tong AC, Ng IO, Yan BS. Variations in clinical presentations of the simple bone cyst: report of cases. J Oral Maxillofac Surg 2003;61:1487-91. [PubMed]
- Ikeshima A, Utsunomiya T. Case report of intra-osseous fibroma: a study on odontogenic and desmoplastic fibromas with a review of the literature. J Oral Sci 2005;47:149-57. [PubMed]
- Tosios KI, Gopalakrishnan R, Koutlas IG. So-called hybrid central odontogenic fibroma/central giant cell lesion of the jaws. A report on seven additional cases, including an example in a patient with cherubism, and hypotheses on the pathogenesis. Head Neck Pathol 2008;2:333-8. [PubMed]
- Nah KS. Central odontogenic fibroma: a case report. Imaging Sci Dent 2011;41:85-8. [PubMed]
- Daskala I, Kalyvas D, Kolokoudias M, et al. Central odontogenic fibroma of the mandible: a case report. J Oral Sci 2009;51:457-61. [PubMed]
- Covani U, Crespi R, Perrini N, et al. Central odontogenic fibroma: a case report. Med Oral Patol Oral Cir Bucal 2005;10 Suppl 2:E154-7. [PubMed]
- Regezi JA. Odontogenic cysts, odontogenic tumors, fibroosseous, and giant cell lesions of the jaws. Mod Pathol 2002;15:331-41. [PubMed]
- Kumar ND, Sherubin JE, Raman U, et al. Solitary bone cyst. Indian J Dent Res 2011;22:172-4. [PubMed]
- Kuhmichel A, Bouloux GF. Multifocal traumatic bone cysts: case report and current thoughts on etiology. J Oral Maxillofac Surg 2010;68:208-12. [PubMed]
- Mupparapu M, Singer SR, Milles M, et al. Simultaneous presentation of focal cemento-osseous dysplasia and simple bone cyst of the mandible masquerading as a multilocular radiolucency. Dentomaxillofac Radiol 2005;34:39-43. [PubMed]


