Comparison of the results of computerized tomographic and diffusion-weighted magnetic resonance imaging techniques in inflammatory bowel diseases
Introduction
The inflammatory bowel diseases (IBD), ulcerative colitis (UC) and Crohn’s disease (CD), are chronic, progressive inflammatory disorders of the GI tract. The pathogenesis of IBD involves environmental, genetic and immunological factors. During the last decades, the incidence of CD has continued to increase worldwide, reaching incidence rates ranging from 3.1 to 14.6/100,000 in North America and from 0.7 to 9.8/100,000 in Europe (1). Incidence rates of UC differ greatly between studies and regions, varying from 1.5 to 24.5 per 100,000 personyears (1,2).
Barium imaging of the gut is now rarely used in the diagnosis of IBD and has been replaced by colonoscopy. Small bowel barium studies are too insensitive and unreliable and have been replaced by enterography (where contrast is swallowed) or enteroclysis (where the contrast is infused via a nasogastric tube) with imaging via computerised tomography (CT) or magnetic resonance (MR) (3,4). Enteroclysis is probably superior, but many patients do not tolerate the nasogastric tube (3). Conventional CT and MRI were modified with the use of oral contrast agents for improved spatial and temporal resolution of the small bowel. So-called computed tomography or magnetic resonance enterography has now widely overtaken the place of small bowel follow through reducing repeated radiation exposure. In this context, CT enterography, which enables global evaluation of the bowels within a short time without using barium and also diffusion-weighted magnetic resonance imaging (DW-MRI) which evaluates movements of bound and free water molecules without any need for contrast agents are gaining important and firm places in the diagnostic armamentarium (5).
Our objective in this study is to compare the findings obtained by CT enterography, which uses oral neutral contrast material and non-contrasted DWI technique and reveal the diagnostic value of DW-MRI in patients with IBD.
Materials and methods
Study design
This prospective study was performed in the radiology department of a tertiary care center between April 2010 and June 2011 after the approval of Institutional Review Board. Written informed consent allowing the use of CT and MRI views for scientific purpose was obtained previously from all patients.
Patients with established or clinically suspect diagnosis of inflammatory bowel disease were included in the study. Pregnants or those suspected to be pregnant, patients with renal failure (serum creatinine >1.5 mg/dL), hemodynamic instability, contraindications for CT or MRI, claustrophobics and cases with known or suspect contrast agent allergy were excluded from the study. CT enterography and DW-MRI were obtained from the patients who were admitted to outpatient clinics or emergency service.
CT enterography protocol
In our clinics as oral neutral contrast material, combination of drinking water to distend bowels and lactulose solution to decrease absorption of intraluminal fluid along the inner layer of the intestinal lumen were used. At least six hours of fasting state is required before radiological examination. The patients were requested to drink a total amount of 1,500 cc water beginning two hours before the examination, at a rate of 250 cc at every 10 minutes during the first hour. During the second hour 250 cc lactulose solution (Osmolak solution 10 g/15 mL, Biofarma, Turkey) had to be added preferably into a 1,000 cc fruit juice (if the patient had not received a definitive or suspect diagnosis of diabetes mellitus) then 1,200 cc of the diluted solution should be completely consumed at a rate of 200 cc per hour. If the patient had received a definitive or suspect diagnosis of diabetes mellitus, 100 cc of this lactulose solution was added into 1,400 cc drinking water and the patients drank this diluted solution at a rate of 250 cc at every 10 minutes amounting to 1,500 cc. Thirty minutes before the radiological examination, 10 mg IM hyoscine-N-butyl bromide (Buscopan vial, Boehringer Ingelheim, Germany) was injected intragluteally. During the preparatory procedure before the examination, the patients did not report any serious complication apart from mild nausea.
Computerized tomography sections were visualized using A Siemens Somatom Sensation (16 detector) device (Siemens Turkey, Istanbul, Turkey). Abdomen and pelvic region were scanned from xyphoid process down to symphysis pubis. For axial pre- and postcontrast image taking, 5 mm collimation, 1.5 pitch and 1mm reconstruction parametres were used.
As intravenous contrast material (IVCM) 100 mL non-ionic iopromide in an iodine concentration of 300 mg/mL [Ultravist, (Schering AG, Berlin, Germany)] was injected IV at a rate of 3 mL/min. Postcontrast axial images were obtained 25 seconds after administration of IVCM during the arterial phase. Axial CT images were sent to a separate workstation (Wizard, Siemens Medical Systems, Erlangen, Germany) via a network. For clearer visualisation of radio pathological findings, from axial images of all cases, axial reformat images with a 1 mm section-thickness, increment of 0.75 mm and collimation at 16×0.75 and also 3-mm thick-coronal MPR images were reconstructed. In addition, evaluations were performed using three-dimensional reformat images reconstructed on workstation monitor for visualisation of potential complications (fistulas etc.). Coronal reformat images were reconstructed which included abdominal skin anteriorly and gluteal skin posteriorly.
Diffusion-weighted MRI protocol
Following CT examination within the same day the patient was transported to the MR unit. Before MRI, no additional preparatory procedure was performed. All radiological examinations were performed using 1.5 Tesla MR device (Signa, General Electric Medical System, Waukesha, WI, USA). Since only diffusion-weighted images were taken, IVCM was not used. An 8-channel body flex coil was used to obtain diffusion images with various b values (b: 400, 600, 800 sec/mm2). All radiological images of the patients were obtained without requiring breath holds.
Detailed parametres: TE, 61; TR, 10,000 msec; Spacing, 0.5; Frequency, 160; Phase, 160; FOV, 48 cm; Nex, 2; Section thickness, 6 mm; Duration, 3.45 min; 160×160 matrix. DW-MRI findings retrieved from axial plane were evaluated and compared.
Outcome analysis
All CT enterography and diffusion-weighted MR images were evaluated by a radiologist blinded to the endoscopic and/or histopathological results. Duodenum, jejunum, ileal loops, ascending, transverse, descending colon and sigmoid colon and rectum were evaluated in that order as for general imaging quality, luminal distension and adequate visualization of the intestinal wall. Image qualities of neutral contrast CT-enterography and DW-MRI were compared.
Statistical analysis
Data were analyzed using the Statistical Package for Social Sciences (SPSS) software (version 11.5 for Windows). In the diagnosis of Crohn’s disease and ulcerative colitis compatibilities between CT-enterography and diffusion weighted imaging were evaluated at following locations: duodenum and then jejunum, ileum, ascending, transverse, descending, sigmoid colon and lastly rectum. In axial plane images obtained from both modalities quality of images, luminal distension and intestinal wall visualization were compared individually. Results were calculated using Kappa statistics and compared with those of gold standard diagnostic techniques as endoscopic/colonoscopic methods. Efficacies, sensitivities and specificities of CT enterography and DW-MRI were calculated and evaluated.
Results
The study included 31 patients (17 men and 14 women). The patients aged between 18-64 years (median, 32.4 years). Mean ages of the male and female patients were 36.8±8.75 and 34.7±9.66 years, respectively.
Sixteen of our patients had Crohn’s disease. Eight cases of them were diagnosed by us using colonoscopic and/or endoscopic techniques. Crohn’s disease of the other patients was already known and they were referred to our gastroenterology polyclinics for the evaluation of activation symptoms. In two patients with known Crohn’s disease, endoscopic techniques revealed diagnosis of duodenitis in addition to ileal involvement. Two patients were diagnosed as ulcerative colitis and referred to our service with suspect intestinal involvement. The remaining 13 patients were referred to our clinics with the intention of making a diagnosis of inflammatory bowel disease by exclusion.
Based on statistical analyses, the best correlation between the results of CT-enterography and DW-MRI were observed in the evaluation of transverse colon (1, P<0.0001), ileum (0.868, P<0.0001) and duodenum (0.817, P<0.0001) in decreasing order and with an almost perfect compatibility. Radiological findings of sigmoid colon (0.795, P<0.0001), jejunum (0.619, P<0.001) and descending colon (0.684, P<0.005) were completely compatible. However, a moderate degree of compatibility was estimated between radiological findings of rectum (0.518, P<0.005) and cecum (0.415, P<0.005).
In our study, sensitivity (88.9% and 100%), specificity (38.4% and 53.9%) of DW-MRI and CT-enterography were also calculated. Although not statistically significant, with diffusion-weighted images obtained at the b value of 600 sec/mm2, better orientation and visualisation were achieved.
Case reports
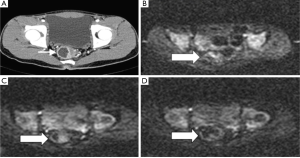
Case 1
A 24-year-old male patient diagnosed as ulcerative colitis and presented with complaints of chronic lower abdominal quadrant pain, malaise and diarrhea. In axial contrasted CT-enterography, in the region indicated by an arrow, increase in rectal thickness consistent with activation and accompanying fixation of the contrast material was observed (Figure 1A). In diffusion-weighted images obtained at the same levels as CT with various b values (b: 400, 600, 800 sec/mm2), increase in signal intensity was compatible with restricted diffusion at these different b values was noted (Figure 1B-D).
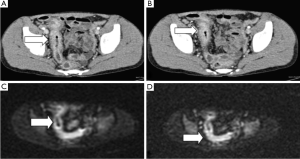
Case 2
A 21-year-old male patient diagnosed as Crohn’s disease and presented with complaints of chronic abdominal pain and recurrent diarrheas. In successively obtained axial contrasted CT-enterography images, increase in the thickness of the terminal ileal wall consistent with activation period, fixation of contrast material and appearance of vascular engorgement: vascular overcrowding in the region indicated by an arrow (Figure 2A,B). In diffusion-weighted images obtained at the same levels as CT with various b values (b: 400, 600, 800 sec/mm2), increase in signal intensity and ileal wall thickness were compatible with restricted diffusion at these different b values (Figure 2C,D).
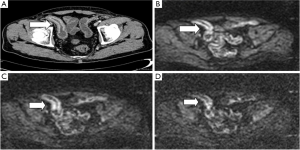
Case 3
A 32-year-old male patient diagnosed as Crohn’s disease and presented with chronic lower right quadrant abdominal pain. On contrasted axial CT-enterograms, increase in the wall thickness of the terminal ileum, fixation of the contrast material and distinct demarcation between pathological and normal ileal wall structure consistent with activation as indicated by an arrow (Figure 3A). In diffusion-weighted images obtained at the same levels as CT with various b values (b: 400, 600, 800 sec/mm2), increase in signal intensity and ileal wall thickness compatible with restricted diffusion at these different b values (Figure 3B-D).
Discussion
In the evaluation of mucosal details and precise localization of the intestinal pathology, superiority of enteroclysis over CT has been demonstrated (6). However, it has many disadvantages such as its inability to directly visualize extramural abnormalities and associated complications, which can accompany endoluminal pathologies. Besides nasojejunal catheterization applied to achieve luminal distension in enteroclysis is a necessary procedure which decreases patient comfort, in addition to higher radiation doses exposed by the patient. In conditions like inflammatory bowel disease where patient population generally consists of younger generation, radiation dose exposure becomes an especially important issue.
Conventional CT examination is used in the diagnosis and monitorization of extraluminal complications, but as for intraluminal involvements, it has some limitations (7). Though capsular endoscopy has a superior role in the visualization of intestinal mucosa and diagnosis of vascular malformation and tumours when compared with CT-enterography, its role in Crohn’s disease is not clear-cut. Though some studies reported that DW-MRI has equivalent effectiveness with enterography in cases with active CD, it is not a first-line imaging modality in cases of stricture development and capsular obstruction and it is selected in a narrow spectrum of patient groups where CT-enterography yields normal results despite persistent clinical suspicion (8).
CT-enterography has become the primary diagnostic modality in intestinal and especially inflammatory bowel diseases with advantages of a higher spatial resolution and superiority in demonstrating both intra- and extraluminal abnormalities. Especially with multi-detector CT technology, number of artifacts originating from respiratory movements decreased. This CT technology also enables visualization of transmural spread of the tumour, intra- and extraperitoneal complications and other systemic signs within the field of vision and provides additional information about vascular structures when used in conjunction with IVCM administration. Also its noninvasive and practical characteristics have recently popularized CT enterographic examinations.
The first studies in the literature which referenced to enteroclysis and intestinal passage graphies with the use of barium, had reported higher degrees of sensitivity (>85%) for CT-enterography in active Crohn’s disease (9,10). However, in studies where endoscopic findings were referenced, sensitivity of CT-enterography for active inflammation was found to be between 77% and 92%, respectively (11,12). However, in our study, sensitivity and specificity of CT-enterography in inflammatory bowel diseases were as 100% and 53.9%, respectively. We thought that specificity of this technique will increase with increasing number of patients and experience.
Oto et al. compared results of contrasted MR and DW-MRI in 18 patients with active Crohn’s disease and detected that when results of DW-MRI were evaluated together with ADC values, the sensitivity of DW-MRI had increased (13). Jensen et al. evaluated MR-enterographic and CT-enterographic examinations performed in 35 symptomatic CD patients and found relatively higher positive, but comparatively lower negative predictive values for DW-MRI (14). Kielar et al., performed low-dose modified intestinal CT examinations in 98 patients diagnosed as CD with newly emerged symptoms using oral contrast material and demonstrated perfect interobserver compatibility in the detection of obstruction and stage of activity (15). However, in our study, the same radiologist, blinded to the identity of the patients evaluated both CT and DW-MRI images and detected relatively higher degrees of sensitivity (88.9%) for DW-MRI.
Kiryu et al. performed DW-MRI on 31 patients diagnosed as CD without breath-holding manoeuvre and got satisfactory results of the image qualities and revealed that evaluation of images obtained, together with assessment of ADC values especially during active phase of the disease would contribute significantly to the quantitative evaluation of the disease (16). In this study, sensitivity and specificity of DW-MRI were found to be 86.0% and 81.4%, respectively. In our study, DW-MR images taken without breath-holding manoeuvres demonstrated optimal visual quality and also the lesions could be adequately localized. Even though, ADC values were not measured in our study, we detected higher degrees of sensitivity (88.9%), but lower degrees of specificity (53.9%) of DW-MRI when compared with the cited study. We did not measure ADC values, which might result in lower degrees of specificity than we had detected in our DW-MRI applications.
Aoyagi et al. performed DW-MRI in seven patients with ulcerative colitis and concluded that measurement of ADC values may play a role in the staging of the disease (17). Kılıçkesmez et al., obtained diffusion-weighted MR images from apparently abnormal pericolonic lymph node adjacent to the affected intestinal wall in a patient diagnosed as ulcerative colitis. The authors also measured ADC values and found that ADC values increased during remission period of the rectal disease and decreased during the active phase. They also noted that ADC estimate of the adjacent pathological lymph node is unrelated to the stage of the disease (18). Oussalah et al. performed DW-MRI in addition to conventional MR on 96 patients (61 CD, 35 UC) with known inflammatory bowel disease and found that bowel preparation before DW-MRI is not required in establishing presence of colonic inflammation in UC (19). We performed firstly bowel preparation and then CT-enterography and diffusion-weighted MR within the same day and possibly because of this approach, sensitivity of our DW-MRI results are higher than those found in the literature.
Small number of patients and failure to measure ADC values are the main limitations of the present study. Clinical diagnosis to include in the study is another limitation. Although, some of the patients had undergone diffusion MR, and CT-enterographic examinations with the indication of clinically suspect IBD with resultant normal findings, not all of the study participants had been definitively diagnosed.
Though conventional enteroclysis is the gold standard method among radiological imaging techniques used for the evaluation of inflammatory small intestinal abnormalities, in diagnosed cases with a suspect recurrence and/or complication, as a first-line method CT enterography should be used with its advantages of relatively easy applicability and tolerability. Finally, especially in children, pregnants, selected patient groups like those experiencing frequent recurrences and in whom history of IBS, drug allergy were elicited during routine controls, in order to avoid radiation risk and potential drug reactions DW-MRI is an alternative method which can be used effectively to obtain useful information. In line with advances cited in the literature and improvements in technical ultrastructure, in patients with proper indications, it is a primary imaging modality to be selected.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Loftus EV Jr. Clinical epidemiology of inflammatory bowel disease: Incidence, prevalence, and environmental influences. Gastroenterology 2004;126:1504-17. [PubMed]
- Farrokhyar F, Swarbrick ET, Irvine EJ. A critical review of epidemiological studies in inflammatory bowel disease Scand J Gastroenterol 2001;36:2-15. [PubMed]
- Moss A, Parrish FJ, Irving PM, et al. Quality, clinical influence and tolerance of computed tomography enteroclysis in patients with suspected small bowel disease. Intern Med J 2009;39:733-43. [PubMed]
- Lawrance IC, Welman CJ, Shipman P, et al. Correlation of MRI-determined small bowel Crohn’s disease categories with medical response and surgical pathology. World J Gastroenterol 2009;15:3367-75. [PubMed]
- Fidler J. MR imaging of the small bowel. Radiol Clin North Am 2007;45:317-31. [PubMed]
- Arslan H, Etlik O, Kayan M, et al. Peroral CT enterography with lactulose solution: preliminary observations. AJR Am J Roentgenol 2005;185:1173-9. [PubMed]
- Nagamata H, Inadama E, Arihiro S, et al. The usefulness of MDCT in Crohn’s disease. Nihon Shokakibyo Gakkai Zasshi 2002;99:1317-25. [PubMed]
- Gay G, Delvaux M, Laurent V, et al. Temporary intestinal occlusion induced by a “patency capsule” in a patient with Crohn’s disease. Endoscopy 2005;37:174-7. [PubMed]
- Mazzeo S, Caramella D, Battolla L, et al. Crohn disease of the small bowel: spiral CT evaluation after oral hyperhydration with isotonic solution. J Comput Assist Tomogr 2001;25:612-6. [PubMed]
- Doerfler OC, Ruppert-Kohlmayr AJ, Reittner P, et al. Helical CT of the small bowel with an alternative oral contrast material in patients with Crohn disease. Abdom Imaging 2003;28:313-8. [PubMed]
- Koh DM, Miao Y, Chinn RJ, et al. MR imaging evaluation of the activity of Crohn’s disease. AJR Am J Roentgenol 2001;177:1325-32. [PubMed]
- Ilangovan R, Burling D, George A, et al. CT enterography: review of technique and practical tips. Br J Radiol 2012;85:876-86. [PubMed]
- Oto A, Kayhan A, Williams JT, et al. Active Crohn’s disease in the small bowel: evaluation by diffusion weighted imaging and quantitative dynamic contrast enhanced MR imaging. J Magn Reson Imaging 2011;33:615-24. [PubMed]
- Jensen MD, Kjeldsen J, Rafaelsen SR, et al. Diagnostic accuracies of MR enterography and CT enterography in symptomatic Crohn’s disease. Scand J Gastroenterol 2011;46:1449-57. [PubMed]
- Kielar AZ, Tao H, McKeever C, et al. Low-Radiation-Dose Modified Small Bowel CT for Evaluation of Recurrent Crohn’s Disease. Gastroenterol Res Pract 2012;2012:598418.
- Kiryu S, Dodanuki K, Takao H, et al. Free-breathing diffusion-weighted imaging for the assessment of inflammatory activity in Crohn’s disease. J Magn Reson Imaging 2009;29:880-6. [PubMed]
- Aoyagi T, Shuto K, Okazumi S, et al. Evaluation of ulcerative colitis using diffusion-weighted imaging. Hepatogastroenterology 2010;57:468-71. [PubMed]
- Kiliçkesmez O, Soylu A, Yaşar N, et al. Is quantitative diffusion-weighted MRI a reliable method in the assessment of the inflammatory activity in ulcerative colitis? Diagn Interv Radiol 2010;16:293-8. [PubMed]
- Oussalah A, Laurent V, Bruot O, et al. Diffusion-weighted magnetic resonance without bowel preparation for detecting colonic inflammation in inflammatory bowel disease. Gut 2010;59:1056-65. [PubMed]


