
The association of cervical sagittal alignment with anterior bone loss following single-level anterior cervical surgery
Introduction
Cervical disc replacement (CDR) is an effective non-fusion technique for the treatment of cervical radiculopathy and myelopathy as an alternative to anterior cervical discectomy and fusion (ACDF). Clinical trials with long-term follow-up and meta-analyses have demonstrated that CDR achieves at least equivalent clinical outcomes compared to ACDF (1-3). Anterior bone loss (ABL) is a bone loss phenomenon of the anterior region of the vertebral bodies usually commencing within 3 months after CDR and remaining stable after the first year (4,5). A recent systematic review by Wahbeh et al. (6) highlighted the distinction between non-inflammatory bone loss and osteolysis after CDR, which may have been used interchangeably in previous reports and led to misleading conclusions. They clarified that osteolysis is a less common complication and presents more than a year postoperatively, which is generally progressive and often leads to revision surgery. By contrast, bone loss is regarded as a non-progressive phenomenon that frequently observed after CDR and rarely leads to revision. Nonetheless, ABL could reduce the contact area of the bone-implant interface and probably increase the implant micromotion and the risk for implant subsidence and even implant failure, which could be more evident in multilevel anterior cervical surgery (7). In addition, the occurrence of ABL may be associated with the pain symptoms at the early stage postoperatively and lead to poor surgical efficacy (5,8). However, the exact mechanism and risk factor of bone loss are still unclear; several hypotheses include mechanical stress shielding, implant micromotion, injury of nutrient vessels, reaction to wear debris, and infection (4,5,8-10). Recently, many researchers have proposed that ABL may be a response to global and segmental biomechanical environment of the cervical spine after surgery, which is also intimately related to the cervical sagittal alignment (11-15). Cervical sagittal alignment plays an important role in transmitting axial loads and maintaining biomechanical balance of the cervical spine, and might be related to the bone remodeling process after anterior cervical surgery (16). Studies have suggested that surgical segment slope may influence the intervertebral fusion process after ACDF (17,18). Cervical sagittal vertical axis (SVA) has also been reported to be associated with the anterior bone formation after CDR (19). However, the association between cervical sagittal alignment and ABL has been underinvestigated.
Previous studies have stated that ABL might not occur at the fusion segment after ACDF due to the more evenly distributed loading force at the bone-implant interface (11,20). Interestingly, we found that the ABL was also visible in the postoperative radiographs of patients who underwent ACDF using zero-profile (Zero-P) cage in our clinical practice (21), which has the same anterior surgical approach and some procedures such as removal of anterior longitudinal ligament, disc tissues, posterior longitudinal ligament, and osteophytes with CDR. Kieser et al. (4) also encouraged the evaluation of ABL after ACDF to further clarify its mechanism. However, occurrence of ABL after ACDF has been rarely reported. Whether the incidence and risk factors for ABL in ACDF would be different from those of CDR remains unclear. Therefore, the present study aimed to investigate the incidence and severity of ABL in single-level CDR and ACDF and explore the association of cervical sagittal alignment with ABL. We present this article in accordance with the STROBE reporting checklist (available at https://qims.amegroups.com/article/view/10.21037/qims-23-1338/rc).
Methods
Study population
This is a single-center retrospective cohort study with prospectively collected data. We searched the database for single-level anterior cervical surgery that had been performed in our center before the study and identified the periods with relatively stable and balanced numbers of CDR and ACDF patients. This study reviewed patients who were admitted from January 2014 to December 2018 and underwent single-level CDR using Prestige-LP disc (Medtronic Sofamor Danek, Memphis, TN, USA) and single-level ACDF Zero-P spacer (Synthes GmbH, Oberdorf, Switzerland) in West China Hospital and were followed up for at least 12 months. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study protocol was approved by the Medical Ethical Committee of West China Hospital, Sichuan University (No. 20190946) and informed consent was provided by all the patients. Patients were included if they were diagnosed with 1-level cervical degenerative disc disease between C3 and C7 causing symptomatic cervical myelopathy or radiculopathy and had no response to strict conservative treatment for at least 12 weeks. Preoperative X-ray, computed tomography (CT), and magnetic resonance imaging (MRI) were performed on all the patients to confirm the diagnoses. Patients were diagnosed if their radiological findings such as spinal cord compression or nerve root compression were consistent with their clinical symptoms and signs. The exclusion criteria were as follows: (I) history of trauma or prior cervical spine surgery; (II) spinal deformity: including basilar invagination, Klippel-Feil syndrome, and spinal scoliosis; (III) spinal tumor, infectious disease, and other non-degenerative cervical spine diseases; (IV) follow-up period <1 year. The demographic data and surgical level distribution between patients who underwent CDR and ACDF were compared.
Surgical techniques
All the surgeries were performed by the same senior spine surgeon. The patient was placed in a supine position with the neck in a neutral position after general anesthesia. A standard right-side Smith-Robinson approach was used. After exposure, thorough decompression of indicated levels was routinely performed, including the removal of anterior longitudinal ligament, disc tissue, cartilage, posterior longitudinal ligament, and osteophytes. A high-speed burr was then used to prepare the endplates. For arthroplasty, a rail cutter and bit were used to drill the fixation channels in the endplate, and a proper-sized Prestige-LP Disc was inserted. For fusion, the appropriate Zero-P spacer filled with artificial or local excised bone was inserted into the intervertebral space. A total of four screws were then implanted and locked. The placement of implants was verified using C-arm fluoroscopy. A drainage tube was inserted after thorough irrigation and meticulous hemostasis before closing the incision. Before discharge, patients were asked to come to the outpatient clinic for clinical and radiological evaluations at 3, 6, 12 months, and once a year after surgery.
Clinical and radiological evaluation
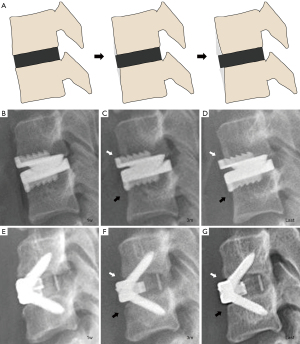
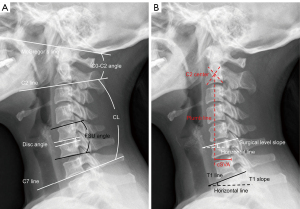
Clinical outcomes of patients were assessed by the Japanese Orthopedic Association (JOA) score (22) and visual analogue scale (VAS) score (23) or the neck at pre-operation and final follow-up. Radiological data were assessed via lateral X-ray at pre-operation, 1 week postoperatively, 3 months postoperatively, and the last follow-up. The stability of the implant was also evaluated regarding implant subsidence and anteroposterior migration. Implant subsidence was defined as a decrease in the average height of anterior and posterior functional spinal unit (FSU) >2 mm (15). Implant anteroposterior migration was defined as the sum of the cranial and caudal translation of anterior border of the implant with respect to the posterior border of the vertebra >3 mm (24). ABL and cervical sagittal alignment parameters were evaluated on the lateral radiographs of the cervical spine, which were obtained with patients in a standing position and maintaining horizontal gaze, with their hips and knees extended. ABL was identified and classified according to the method of Kieser et al. (4,10). The 1-week postoperative X-ray was used as the baseline for ABL assessment and ABL was assessed at last follow-up. The X-ray of last follow-up was compared to that at 1-week postoperatively to determine the decreasing percentage of vertebral endplate length of the surgical level. ABL was classified into three groups: mild (≤5%), moderate (>5% and ≤10%), and severe (>10%). The location of ABL was also recorded based on the position of ABL relative to the implant, and each surgical level was divided into upper ABL (UABL) group and non-UABL group, lower ABL (LABL) and non-LABL group, respectively (Figure 1). The incidence, severity, and location of ABL were compared between the CDR and ACDF groups. In addition, the comparison of demographic data, surgical level distribution, and intraoperative data were performed between patients with and without ABL in CDR and ACDF group, respectively. Cervical sagittal alignment parameters included C0–C2 angle, cervical lordosis (CL), C2–C7 SVA (cSVA), T1 slope, FSU angle, disc angle, and surgical level slope. C0–C2 angle was defined as the angle between McGregor’s line and inferior endplate of C2 vertebral body. CL was recorded through C2–C7 Cobb angle. cSVA was measured by the distance between the posterosuperior corner of C7 vertebra and the plumb line from the center of C2 vertebra. T1 slope was defined as the angle between the superior endplate of T1 and the horizontal line. FSU angle was the angle between the lines from the superior endplate of the cranial vertebra and the inferior endplate of the caudal vertebra of the surgical level. Disc angle refers to the angle formed between the upper and lower endplates of the surgical intervertebral space. Surgical level slope was defined as the angle between the lower endplate of the surgical level and the horizontal line (Figure 2). We compared the differences of sagittal alignment parameters and their changes between patients with and without ABL in the CDR and ACDF groups, respectively. The relationship between sagittal alignment parameters and the severity of ABL was also explored. All the radiological measurements were independently assessed by two spine surgeons, and the means value of their measurements were used for subsequent analysis.
Statistical analysis
Statistical analyses were performed using the software SPSS 25.0 (IBM Corp., Armonk, NY, USA). The interobserver reliability of the radiological measurements was assessed using intraclass correlation coefficient (ICC). Results for continuous variables such as cervical sagittal parameters, clinical outcome score, age, and body mass index (BMI) were presented as mean ± standard deviation. Independent t-test was used to analyze the differences of these data between groups with and without ABL when the data followed normal distribution. Mann-Whitney U test was used for the comparison if the data were non-normally distributed. Categorical variables, including the incidence, degree, location of ABL, gender, implant subsidence, and so on, were presented as case number and percentage. Chi-square or Fisher’s exact test was used for the comparison of above categorical variables between groups according to the requirements. A two-tailed P value <0.05 was defined as statistical significance.
Results
Patient demographics
Initially, 364 patients who underwent single-level CDR and ACDF were identified. Among them, 273 patients met the inclusion criteria and were included in further screening. After excluding other types of implants and patients with previous cervical surgery history, 245 participants were enrolled for data collection. Finally, 212 patients with a minimum of 12-month follow-up and complete clinical and radiological data were enrolled in this study (Figure 3), including 113 patients who underwent single-level CDR and 99 patients who underwent single-level ACDF. There were 46 males and 67 females in the CDR group and 48 males and 51 females in the ACDF group. The mean age of patients at the time of surgery was 42.83±8.53 years in the CDR group and 50.91±11.81 years in the ACDF group (P<0.001), with a mean follow-up period of 27.05±17.27 months. The surgical level distribution in CDR and ACDF group were 5 and 8 cases at C3/4, 18 and 6 at C4/5, 80 and 78 at C5/6, and 10 and 7 at C6/7, respectively. Detailed information on demographic data is summarized in Table 1. No implant and screw loosening happened and none of the patients required a second surgery of the index or adjacent segment in this cohort.
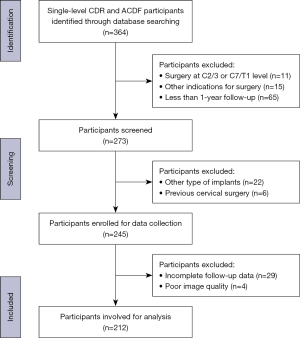
Table 1
| Variable | CDR | ACDF | P value |
|---|---|---|---|
| No. of patients | 113 | 99 | – |
| Age (years) | 42.83±8.53 | 50.91±11.81 | <0.001* |
| Sex (M/F) | 46/67 | 48/51 | 0.25 |
| BMI (kg/m2) | 22.80±2.53 | 23.52±3.19 | 0.10 |
| Follow-up (months) | 29.65±18.84 | 24.09±14.82 | 0.14 |
Data are presented as mean ± standard deviation for continuous variables and presented as case number for categorical variables. *, statistically significant difference. CDR, cervical disc replacement; ACDF, anterior cervical discectomy and fusion; BMI, body mass index; M, male; F, female.
Overview of ABL
The ICC for interobserver reliability of ABL was 0.91. The ICC of cervical sagittal parameters also showed excellent agreement (0.90 for C0–C2 angle, 0.96 for CL, 0.92 for cSVA, 0.94 for T1 slope, 0.90 for FSU angle, 0.95 for surgical level slope, and 0.94 for disc angle, respectively). Among 212 patients, ABL was identified in 75 (66.4%) patients in the CDR group and 57 (57.6%) patients in the ACDF group (P=0.19). For patients in CDR group, mild ABL occurred in 26 (23.0%) segments, moderate ABL occurred in 36 (31.9%) segments, and severe ABL occurred in 13 (11.5%) segments. In the ACDF group, there were 21 cases (21.2%) of mild ABL, 22 cases (22.2%) of moderate ABL, and 14 cases (14.1%) of severe ABL. ABL of the upper adjacent level was found in 67 patients (59.3%) in CDR group and 53 patients (53.5%) in ACDF group, while ABL of the lower adjacent level was detected in 48 patients (42.5%) for CDR and 40 patients (40.4%) for ACDF. 40 patients (35.4%) in the CDR group and 36 patients (36.4%) in the ACDF group had ABL in both upper and lower levels. There were no significant differences in the incidence, degree, and location of ABL between ACDF and CDR groups (Table 2). For patients who underwent CDR, there were no significant differences in age, sex, BMI, blood loss, operative time, and surgical levels between ABL and non-ABL groups. For patients treated with ACDF, significant differences were found in sex and BMI between patients with and without ABL. The proportion of females was significantly higher in the ABL group (P=0.002), whereas the BMI was significantly lower in the ABL group compared to the non-ABL group (P=0.002). When we further analyzed the relationship between age, sex, and BMI with ABL regardless of surgical intervention, the proportion of females was significantly higher in the ABL group (P=0.001), whereas the BMI was significantly lower in the ABL group compared with the non-ABL group (P=0.003) (Table S1). In ACDF and CDR groups, short-term clinical outcomes including JOA and VAS of patients with and without bone resorption showed significant improvement after surgery, and there were no significant differences between patients with and without ABL in the ACDF group and CDR group at pre-operation and last follow-up. No implant migration was observed in this study. The subsidence rate was comparable between the ABL and non-ABL groups (Table 3).
Table 2
| Variable | CDR | ACDF | P value |
|---|---|---|---|
| ABL | 75 (66.4) | 57 (57.6) | 0.19 |
| Degree of ABL | 0.36 | ||
| None | 38 (33.6) | 42 (42.4) | |
| Mild | 26 (23.0) | 21 (21.2) | |
| Moderate | 36 (31.9) | 22 (22.2) | |
| Severe | 13 (11.5) | 14 (14.1) | |
| Location of ABL | |||
| Upper level | 67 (59.3) | 53 (53.5) | 0.40 |
| Lower level | 48 (42.5) | 40 (40.4) | 0.76 |
| Both | 40 (35.4) | 36 (36.4) | 0.88 |
Data are presented as n (%). CDR, cervical disc replacement; ACDF, anterior cervical discectomy and fusion; ABL, anterior bone loss.
Table 3
| Variables | CDR | ACDF | |||||
|---|---|---|---|---|---|---|---|
| Non-ABL | ABL | P value | Non-ABL | ABL | P value | ||
| No. of patients | 38 | 75 | – | 42 | 57 | – | |
| Age (years) | 43.00±9.45 | 42.75±8.10 | 0.88 | 53.19±12.47 | 49.23±11.12 | 0.10 | |
| Sex (M/F) | 19/19 | 27/48 | 0.15 | 28/14 | 20/37 | 0.002* | |
| BMI (kg/m2) | 23.02±2.62 | 22.68±2.50 | 0.50 | 24.60±3.04 | 22.72±3.09 | 0.002* | |
| Blood loss (mL) | 48.29±31.11 | 49.47±32.96 | 0.26 | 49.76±17.87 | 51.58±25.06 | 0.63 | |
| Operative time (min) | 113.68±27.15 | 119.20±23.12 | 0.85 | 120.00±22.95 | 122.11±27.69 | 0.68 | |
| Level distribution | 0.22 | 0.08 | |||||
| C3/4 | 1 | 4 | 3 | 5 | |||
| C4/5 | 4 | 14 | 1 | 5 | |||
| C5/6 | 27 | 53 | 32 | 46 | |||
| C6/7 | 6 | 4 | 6 | 1 | |||
| JOA score | |||||||
| Pre-operation | 12.23±0.93 | 12.04±1.15 | 0.83 | 12.19±0.66 | 11.97±0.67 | 0.28 | |
| Last follow-up | 15.85±0.38 | 16.09±0.85 | 0.33 | 16.06±0.57 | 15.87±0.51 | 0.24 | |
| VAS score | |||||||
| Pre-operation | 5.82±0.65 | 5.81±0.61 | 0.92 | 5.64±0.79 | 5.51±0.80 | 0.41 | |
| Last follow-up | 1.55±0.50 | 1.51±0.50 | 0.64 | 1.31±0.52 | 1.37±0.49 | 0.61 | |
| Implant subsidence | 4 | 6 | 0.73 | 8 | 7 | 0.35 | |
Data are presented as mean ± standard deviation for continuous variables and presented as case number for categorical variables. *, statistically significant difference. CDR, cervical disc replacement; ACDF, anterior cervical discectomy and fusion; ABL, anterior bone loss; BMI, body mass index; JOA, Japanese Orthopedic Association; VAS, visual analogue scale.
Cervical sagittal alignment and ABL
The comparison of cervical sagittal alignment parameters at pre-operation, 1 week, 3 months postoperatively, and last follow-up between patients with and without ABL are shown in Table 4. In the CDR group, no significant differences were found in the cervical sagittal parameters between patients with and without ABL. For patients who underwent ACDF, the CL at 1 week after surgery was significantly lower in the ABL group compared to non-ABL group (11.83°±8.24° vs. 15.25°±8.32°, P=0.04), whereas the T1 slope at this point in the ABL group was also significantly lower than that of non-ABL group (24.06°±6.85° vs. 27.35°±8.19°, P=0.03). Similarly, at the last follow-up, patients with ABL showed significantly smaller T1 slope compared to those without ABL (22.77°±7.08° vs. 25.78°±7.37°, P=0.02), and the CL was lower in the ABL group than that in non-ABL group yet the difference did not achieve statistical significance (11.40°±8.28° vs. 14.76°±8.71°, P=0.05). Notably, the surgical level slope in patients with ABL was constantly lower compared to patients without ABL before surgery and during follow-up, and the differences were statistically significant at pre-operation (12.05°±5.98° vs. 14.71°±6.69°, P=0.02) and last follow-up (13.99°±6.43° vs. 16.97°±5.88°, P=0.02). No significant differences in sagittal parameters of ABL with different severity were observed (Figures S1,S2).
Table 4
| Variables | CDR | ACDF | |||||
|---|---|---|---|---|---|---|---|
| Non-ABL | ABL | P value | Non-ABL | ABL | P value | ||
| No. of patients | 38 | 75 | – | 42 | 57 | – | |
| C0–C2 angle (°) | |||||||
| Pre-operation | 20.69±6.14 | 22.93±8.70 | 0.12 | 22.00±7.00 | 22.30±8.19 | 0.85 | |
| 1 week | 17.42±5.67 | 19.38±7.16 | 0.14 | 20.91±7.14 | 19.38±6.34 | 0.26 | |
| 3 months | 22.02±6.61 | 23.06±6.93 | 0.45 | 25.16±8.25 | 23.30±7.67 | 0.25 | |
| Last follow-up | 20.60±7.17 | 22.94±8.10 | 0.13 | 22.29±8.23 | 21.86±7.71 | 0.79 | |
| CL (°) | |||||||
| Pre-operation | 8.50±9.37 | 8.00±9.06 | 0.79 | 10.08±9.11 | 9.37±11.26 | 0.74 | |
| 1 week | 15.46±8.50 | 12.58±8.70 | 0.10 | 15.25±8.32 | 11.83±8.24 | 0.04* | |
| 3 months | 10.27±9.15 | 8.98±8.16 | 0.45 | 12.73±9.84 | 9.11±9.79 | 0.07 | |
| Last follow-up | 12.64±7.24 | 12.02±8.12 | 0.69 | 14.76±8.71 | 11.40±8.28 | 0.05 | |
| cSVA (mm) | |||||||
| Pre-operation | 19.64±8.86 | 17.48±8.36 | 0.21 | 19.59±12.40 | 15.11±9.29 | 0.12 | |
| 1 week | 19.40±9.43 | 20.95±8.54 | 0.38 | 22.92±10.72 | 19.75±9.81 | 0.13 | |
| 3 months | 18.26±8.76 | 19.43±8.64 | 0.50 | 20.48±10.35 | 19.71±9.74 | 0.70 | |
| Last follow-up | 19.02±8.90 | 18.26±7.58 | 0.64 | 21.31±9.14 | 17.54±9.92 | 0.06 | |
| T1 slope (°) | |||||||
| Pre-operation | 19.07±5.90 | 18.89±7.25 | 0.89 | 22.52±6.91 | 21.74±6.69 | 0.58 | |
| 1 week | 22.45±6.02 | 22.49±6.56 | 0.97 | 27.35±8.19 | 24.06±6.85 | 0.03* | |
| 3 months | 19.36±5.56 | 20.04±6.54 | 0.58 | 23.97±6.88 | 23.28±7.15 | 0.63 | |
| Last follow-up | 20.35±5.28 | 19.80±7.44 | 0.68 | 25.78±7.37 | 22.77±7.08 | 0.02* | |
| FSU angle (°) | |||||||
| Pre-operation | −1.54±5.31 | −1.15±4.49 | 0.68 | 0.71±4.58 | 0.59±5.78 | 0.87 | |
| 1 week | 2.65±3.93 | 2.24±4.34 | 0.62 | 5.15±4.33 | 3.67±3.92 | 0.08 | |
| 3 months | 0±4.71 | −0.03±4.51 | 0.98 | 3.32±3.19 | 2.98±4.05 | 0.66 | |
| Last follow-up | −0.63±3.75 | −0.20±4.59 | 0.62 | 2.32±3.27 | 2.94±4.28 | 0.49 | |
| Surgical level slope (°) | |||||||
| Pre-operation | 13.25±5.90 | 11.50±6.59 | 0.17 | 14.71±6.69 | 12.05±5.98 | 0.02* | |
| 1 week | 17.50±7.92 | 17.99±5.92 | 0.71 | 18.20±7.76 | 15.67±5.78 | 0.08 | |
| 3 months | 15.64±6.58 | 15.74±6.32 | 0.94 | 16.33±6.13 | 15.00±5.95 | 0.21 | |
| Last follow-up | 16.28±8.56 | 15.55±5.92 | 0.60 | 16.97±5.88 | 13.99±6.43 | 0.02* | |
Data are presented as mean ± standard deviation. *, statistically significant difference. ABL, anterior bone loss; CDR, cervical disc replacement; ACDF, anterior cervical discectomy and fusion; CL, cervical lordosis; cSVA, C2–C7 sagittal vertical axis; FSU, functional spinal unit.
Cervical sagittal alignment and ABL of upper and lower adjacent level
The association of postoperative cervical sagittal alignment and ABL of the upper and lower adjacent level is presented in Tables 5,6. In the CDR group, patients with UABL had significantly higher C0–C2 angle at 1 week after surgery compared to those without UABL (19.85°±6.74° vs. 17.07°±6.45°, P=0.03), and no significant differences were found between patients with and without LABL. In the ACDF group, patients with LABL had significantly smaller cSVA at 1 week postoperatively (17.77±10.08 vs. 23.35±9.86 mm, P=0.007) and last follow-up (15.80±9.66 vs. 21.41±9.18 mm, P=0.004). In the CDR group, the change of disc angle during follow-up was significantly smaller in the UABL segments than that of non-UABL segments (−2.73°±3.82° vs. −4.46°±3.78°, P=0.02). No significant correlation of the CL and disc angle changes with ABL was observed in the ACDF group.
Table 5
| Variables | CDR | ACDF | |||||
|---|---|---|---|---|---|---|---|
| Non-UABL | UABL | P value | Non-UABL | UABL | P value | ||
| No. of patients | 46 | 67 | – | 46 | 53 | – | |
| C0–C2 angle (°) | |||||||
| Post-op | 17.07±6.45 | 19.85±6.74 | 0.03* | 21.05±7.34 | 19.14±6.02 | 0.16 | |
| 3 months | 21.44±7.15 | 23.58±6.48 | 0.10 | 25.16±8.01 | 23.16±7.83 | 0.21 | |
| Last follow-up | 20.44±7.26 | 23.33±8.06 | 0.05 | 22.60±8.20 | 21.56±7.67 | 0.52 | |
| CL (°) | |||||||
| Post-op | 14.95±8.90 | 12.58±8.49 | 0.14 | 15.01±8.09 | 11.78±8.46 | 0.06 | |
| 3 months | 9.84±8.89 | 9.13±8.26 | 0.66 | 12.06±9.91 | 9.41±9.86 | 0.19 | |
| Last follow-up | 11.96±7.68 | 12.42±7.95 | 0.76 | 14.38±8.76 | 11.49±8.28 | 0.09 | |
| cSVA (mm) | |||||||
| Post-op | 18.63±9.61 | 21.66±8.11 | 0.07 | 21.97±11.18 | 20.33±9.46 | 0.43 | |
| 3 months | 17.80±8.25 | 19.88±8.89 | 0.21 | 20.43±9.98 | 19.69±10.02 | 0.71 | |
| Last follow-up | 18.82±8.45 | 18.30±7.76 | 0.73 | 20.50±9.48 | 17.97±9.88 | 0.20 | |
| Disc angle (°) | |||||||
| Post-op | 5.02±5.68 | 5.02±4.77 | 0.67 | 1.72±1.67 | 2.20±1.93 | 0.19 | |
| 3 months | 1.44±6.09 | 3.06±4.52 | 0.13 | 1.61±1.39 | 1.54±2.14 | 0.81 | |
| Last follow-up | 0.55±5.66 | 2.29±4.43 | 0.07 | 0.86±1.45 | 1.37±1.69 | 0.06 | |
| ΔCL (°) | |||||||
| Post-pre | 6.65±7.45 | 4.50±8.84 | 0.18 | 5.53±10.30 | 1.94±9.93 | 0.08 | |
| Last-post | −2.99±7.83 | −0.17±8.33 | 0.07 | −0.63±6.94 | −0.29±7.11 | 0.81 | |
| ΔDisc angle (°) | |||||||
| Post-pre | 4.65±6.11 | 5.15±4.34 | 0.52 | 0.64±2.67 | 1.24±3.75 | 0.65 | |
| Last-post | −4.46±3.78 | −2.73±3.82 | 0.02* | −0.85±2.04 | −0.84±2.51 | 0.97 | |
Data are presented as mean ± standard deviation. *, statistically significant difference. CDR, cervical disc replacement; ACDF, anterior cervical discectomy and fusion; UABL, upper anterior bone loss; post-op, values at 1 week postoperatively; CL, cervical lordosis; cSVA, C2–C7 sagittal vertical axis; post-pre, values at 1 week postoperatively minus preoperative values; last-post, values at last follow-up minus values at 1 week postoperatively.
Table 6
| Variables | CDR | ACDF | |||||
|---|---|---|---|---|---|---|---|
| Non-LABL | LABL | P value | Non-LABL | LABL | P value | ||
| No. of patients | 65 | 48 | – | 59 | 40 | – | |
| C0–C2 angle (°) | |||||||
| Post-op | 18.74±5.84 | 18.69±7.85 | 0.96 | 20.53±7.21 | 19.29±5.87 | 0.37 | |
| 3 months | 23.07±6.77 | 22.22±6.91 | 0.51 | 24.71±7.88 | 23.17±8.03 | 0.35 | |
| Last follow-up | 21.82±7.53 | 22.60±8.31 | 0.60 | 21.98±7.96 | 22.14±7.91 | 0.92 | |
| CL (°) | |||||||
| Post-op | 14.59±8.81 | 12.14±8.44 | 0.14 | 14.12±8.73 | 12.04±7.85 | 0.23 | |
| 3 months | 9.83±9.12 | 8.85±7.60 | 0.54 | 11.32±9.94 | 9.64±9.94 | 0.41 | |
| Last follow-up | 12.49±7.40 | 11.87±8.40 | 0.68 | 13.52±8.45 | 11.81±8.79 | 0.33 | |
| cSVA (mm) | |||||||
| Post-op | 20.65±8.78 | 20.12±9.00 | 0.75 | 23.35±9.86 | 17.77±10.08 | 0.007* | |
| 3 months | 19.00±8.64 | 19.08±8.78 | 0.96 | 20.37±10.49 | 19.54±9.22 | 0.69 | |
| Last follow-up | 19.44±8.45 | 17.26±7.29 | 0.15 | 21.41±9.18 | 15.80±9.66 | 0.004* | |
| Disc angle (°) | |||||||
| Post-op | 5.59±5.59 | 4.25±4.37 | 0.33 | 1.73±1.52 | 2.35±2.15 | 0.21 | |
| 3 months | 2.84±5.59 | 1.80±4.75 | 0.30 | 1.55±1.45 | 1.60±2.29 | 0.85 | |
| Last follow-up | 1.86±5.44 | 1.21±4.41 | 0.50 | 0.83±1.52 | 1.58±1.63 | 0.06 | |
| ΔCL (°) | |||||||
| Post-pre | 5.85±7.94 | 4.74±8.89 | 0.49 | 3.12±10.84 | 4.34±9.29 | 0.56 | |
| Last-post | −2.09±7.63 | −0.27±8.92 | 0.24 | −0.60±7.42 | −0.23±6.42 | 0.80 | |
| ΔDisc angle (°) | |||||||
| Post-pre | 5.27±5.64 | 4.50±4.32 | 0.38 | 0.53±2.56 | 1.59±4.09 | 0.24 | |
| Last-post | −3.73±4.15 | −3.03±3.49 | 0.35 | −0.89±1.99 | −0.77±2.70 | 0.80 | |
Data are presented as mean ± standard deviation. *, statistically significant difference. CDR, cervical disc replacement; ACDF, anterior cervical discectomy and fusion; LABL, lower anterior bone loss; post-op, values at 1 week postoperatively; CL, cervical lordosis; cSVA, C2–C7 sagittal vertical axis; post-pre, values at 1 week postoperatively minus preoperative values; last-post, values at last follow-up minus values at 1 week postoperatively.
Discussion
In this study, we found that ABL was common after both CDR and ACDF. Cervical sagittal alignment was closely associated with ABL after ACDF whereas it had less effect on ABL after CDR. We postulated that this might be due to different segmental motion and bone remodeling process at the bone-implant interface between CDR and ACDF. Previous studies had suggested that early osseointegration is feasible in the prosthesis and endplate interface after CDR, which enables a firm fixation between the prosthesis and vertebral endplate (11,25-29); however, such a remodeling process is absent after ACDF using Zero-P spacers (30). In addition, the arthroplasty segment may have the potential to adapt to the cervical sagittal alignment by changing the segmental angle due to its preserved motion. Accordingly, we found that patients without ABL of the upper adjacent level had significantly larger postoperative changes in disc angle. In contrast, the fusion segment had limited ability to change after surgery, thereby being frequently affected by the sagittal alignment. Notably, we only involved patients with single-level cervical degenerative disc disease in the present study, thus their sagittal alignments were less imbalanced and within the relatively normal range. According to the bone physiology feature, disuse-mode remodeling would commence to remove some bone if the bone strain is below the lower threshold of steady state (31). Thus, the biomechanical differences caused by differences in sagittal alignment may not have been significant enough to reach the bone remodeling threshold in this study. The relationship between sagittal alignment and bone loss might be more apparent after multilevel anterior cervical surgery and warrants further studies.
Previous studies have supposed that ABL is a phenomenon unique to CDR and may not occur after ACDF (11,12,20); however, in this study, we found that ABL was also frequently observed in patients treated with ACDF using Zero-P spacer, which is composed of an anterior Zero-P titanium plate and posterior polyetheretherketone (PEEK) cage. In our study, ABL was identified in 66.4% of patients after CDR and 57.6% of patients after ACDF, which is consistent with previous studies. Kieser et al. (4) found that ABL was a common condition identified in 57.1% of segments after CDR, which typically commenced within 3 months after surgery and remained stable after the first year. Chen et al. (11) reported that 43.8% of patients treated with CDR developed ABL of the upper adjacent vertebra, while 44.6% had ABL of the lower adjacent vertebra. A study by Wu et al. (13) suggested that ABL was detected in 56.6% of patients after CDR, most of which occurred within the first 3 months, and no further progression was found after 12 months. Kieser et al. (4) believed that the development of ABL was less affected by implant-related stress shielding but mainly due to the surgical technique used in anterior cervical surgery. The widely used Smith-Robinson approach in anterior cervical surgery includes the resection of anterior longitudinal ligament, which could contribute to decreased stress in the anterior portion of the vertebra and result in bone resorption (32). In this regard, despite the differences in implant and postoperative mobility, ABL could also occur after ACDF surgery using Zero-P implant. In addition, we found that there were no significant differences in the incidence, severity, and location of ABL between CDR and ACDF groups in the current study. However, it must be clarified that the results were likely affected by the differences in age between the CDR and ACDF groups because the patients treated with ACDF were older than those who received CDR due to the different surgical indications. Besides, there were more female patients with ABL than male patients in both ACDF and CDR groups; the difference was significant in the ACDF group yet did not reach statistical significance in the CDR group. We interpreted that this may be related to the postmenopausal bone loss in females because of the generally older ages of patients in the ACDF group (33,34). Furthermore, we found that patients with ABL in the ACDF group had significantly lower BMI, which is consistent with previous reports (35,36). Patients with lower BMI may have higher levels of daily activities that could contribute to micromovement, which is considered another mechanism of bone loss (6,8,35). Interestingly, this study also found that sex and BMI were significantly correlated with ABL independent of surgical intervention, indicating that ABL may be a remodeling process influenced by systemic metabolism. Thus, further study with prospective randomized controlled designs is warranted to compare the incidence and severity of ABL after CDR and ACDF, in which the baseline conditions of patients in the two groups could be more comparable. Alternatively, the evaluation of ABL is supposed to be a routine item in prospective CDR or ACDF study.
In this study, the effects of the occurrence of ABL on clinical outcome scores and implant subsidence or migration were not observed for both ACDF and CDR patients, which was consistent with previous reports (4,11-14). For patients who underwent CDR, Kieser et al. (4) reported that ABL had no effects on the clinical outcomes or the requirement for revision. Wang et al. (14) also concluded that ABL neither influences patient outcomes nor increases the risk of postoperative complications. In addition, Wahbeh et al. (6) summarized the studies of bone loss after CDR in a recent systematic review and concluded that only one study reported the implant failure with severe bone loss (7). In this case, extensive bone loss with deformity was found on the radiographs 52 months postoperatively, and the patient presented with recurrent neck and arm pain with no alleviation until revision (7). In contrast, Heo et al. (5) reported early neck pain in the major bone loss group with long-term improvement. Due to the short-term follow-up of the current study, the mid-term and long-term influences of ABL on ACDF and CDR still need further observation.
Our results suggested that patients with ABL in the ACDF group had significantly smaller postoperative CL and T1 slope. When further analyses according to the location of ABL were performed, it was noted that cSVA was also significantly lower in patients with ABL of the lower adjacent level. cSVA is a parameter that measures the translation of cervical spine in the sagittal plane (16). Due to the inherent trigonometric relationships of the cervical spine, cSVA was considered the function of CL and T1 slope, which has been supported by both theoretical geometrical relationship and radiographic data analysis (37,38). Besides, a biomechanical study showed that increasing cSVA resulted in an increased mechanical burden of the anterior column of the cervical spine (39). Thus, it is assumed that larger SVA could impose more stress on the anterior portion of cervical spine and might prevent the development of bone resorption. For the regional sagittal parameter, postoperative surgical level slope was significantly smaller in the ABL group and had a similar trend with T1 slope. Surgical level slope may be influenced by the T1 slope, which acts like the abutment of the cervical spine. Sheng et al. (18) found an obvious correlation between T1 slope and surgical level slope. They also determined that increasing surgical level slope was a risk factor for non-fusion at postoperative early stage. The increased shear stress caused by the larger segmental slope may be detrimental to the bone remodeling process. However, the underlying mechanism requires further biomechanical study. Furthermore, when further exploring the relationships between cervical sagittal alignment with the severity of ABL, no significant differences were found. There are two possible reasons for this result. First, when categorized into four groups, each group had a limited number of patients compared to the classification of ABL and non-ABL directly. Second, the classification of the ABL severity used in this study was an ordinal classification based on the decreasing percentage of vertebral endplate length of surgical level. The determination of threshold value between each category may also affect the correlation.
In the CDR group, patients with ABL of the upper adjacent level had significantly larger postoperative C0–C2 angle. The cervical spine is responsible for supporting the weight of the head. We hypothesized that an increase in C0–C2 angle may be accompanied with patients lifting their head and transferring more axial load to posterior column of cervical spine, thus reducing the load in the anterior column of the cervical spine. According to the bone physiology feature, the reduction of the load in the anterior portion of vertebral body may promote the development of bone resorption. Furthermore, we found that patients with ABL of the upper adjacent level had larger disc angles at last follow-up in the CDR group. However, the difference did not reach statistical significance (P=0.07), probably attributed to the relatively small number of patients. Similarly, Chen et al. (11) retrospectively reviewed 121 patients who underwent CDR using a Bryan disc and found that a larger shell angle might be the risk factor for ABL. For the segment with a larger shell angle, more loading could be shifted to the posterior components after surgery, thus reducing the loading undertaken by the anterior vertebral body.
There were several limitations to the present study. First, the retrospective nature may have allowed a potential bias. Second, the differences of several sagittal parameters such as FSU angle, disc angle, and surgical level slope were found between patients with and without ABL in the CDR group, yet the differences did not reach statistical significance, probably attributed to the relatively small sample sizes. Third, we used X-rays to detect ABL, which may be less sensitive than CT for ABL. Fourth, since we mainly focused on the relationship between cervical sagittal alignment and ABL, analyses of other factors of ABL were not involved. Fifth, only one type of implant was analyzed in both CDR and ACDF groups, which may undermine the generalizability of the results. Future studies with large sample sizes and different implants may provide more valuable insights into the mechanism of ABL. Despite these limitations, to the best of our knowledge, this is the first study to comprehensively explore the relationship between ABL and cervical sagittal alignment after single-level anterior cervical surgery.
Conclusions
ABL was a common phenomenon after CDR and ACDF. The incidence, severity, and location of ABL were comparable between patients treated with CDR and ACDF. The cervical sagittal alignment was closely related to the occurrence of ABL after ACDF yet had less influence on ABL after CDR, probably due to the preserved motion and the development of osseointegration in the bone-implant interface after CDR. Patients with ABL in the ACDF group had smaller postoperative CL, T1 slope, SVA, and surgical level slope.
Acknowledgments
The abstract of the article has been reported at the 43rd SICOT Orthopedic World Congress.
Funding: This work was supported by
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://qims.amegroups.com/article/view/10.21037/qims-23-1338/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-23-1338/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study protocol was approved by the Medical Ethical Committee of West China Hospital, Sichuan University (No. 20190946) and informed consent was provided by all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Lavelle WF, Riew KD, Levi AD, Florman JE. Ten-year Outcomes of Cervical Disc Replacement With the BRYAN Cervical Disc: Results From a Prospective, Randomized, Controlled Clinical Trial. Spine (Phila Pa 1976) 2019;44:601-8. [Crossref] [PubMed]
- Findlay C, Ayis S, Demetriades AK. Total disc replacement versus anterior cervical discectomy and fusion: a systematic review with meta-analysis of data from a total of 3160 patients across 14 randomized controlled trials with both short- and medium- to long-term outcomes. Bone Joint J 2018;100-B:991-1001. [Crossref] [PubMed]
- Gornet MF, Lanman TH, Burkus JK, Dryer RF, McConnell JR, Hodges SD, Schranck FW. Two-level cervical disc arthroplasty versus anterior cervical discectomy and fusion: 10-year outcomes of a prospective, randomized investigational device exemption clinical trial. J Neurosurg Spine 2019; Epub ahead of print. [Crossref]
- Kieser DC, Cawley DT, Fujishiro T, Tavolaro C, Mazas S, Boissiere L, Obeid I, Pointillart V, Vital JM, Gille O. Anterior Bone Loss in Cervical Disc Arthroplasty. Asian Spine J 2019;13:13-21. [Crossref] [PubMed]
- Heo DH, Lee DC, Oh JY, Park CK. Bone loss of vertebral bodies at the operative segment after cervical arthroplasty: a potential complication? Neurosurg Focus 2017;42:E7. [Crossref] [PubMed]
- Wahbeh JM, Park SH, Campbell P, Ebramzadeh E, Sangiorgio SN. The lexicon for periprosthetic bone loss versus osteolysis after cervical disc arthroplasty: a systematic review. Eur Spine J 2022;31:830-42. [Crossref] [PubMed]
- Hacker FM, Babcock RM, Hacker RJ. Very late complications of cervical arthroplasty: results of 2 controlled randomized prospective studies from a single investigator site. Spine (Phila Pa 1976) 2013;38:2223-6. [Crossref] [PubMed]
- Ren X, Wang W, Chu T, Wang J, Li C, Jiang T. The intermediate clinical outcome and its limitations of Bryan cervical arthroplasty for treatment of cervical disc herniation. J Spinal Disord Tech 2011;24:221-9. [Crossref] [PubMed]
- Kim SH, Chung YS, Ropper AE, Min KH, Ahn TK, Won KS, Shin DA, Han IB. Bone loss of the superior adjacent vertebral body immediately posterior to the anterior flange of Bryan cervical disc. Eur Spine J 2015;24:2872-9. [Crossref] [PubMed]
- Kieser DC, Cawley DT, Fujishiro T, Mazas S, Boissière L, Obeid I, Pointillart V, Vital JM, Gille O. Risk factors for anterior bone loss in cervical disc arthroplasty. J Neurosurg Spine 2018;29:123-9. [Crossref] [PubMed]
- Chen TY, Chen WH, Tzeng CY, Huang CW, Yang CC, Chen HT, Chang CC, Lee CY, Tsou HK. Anterior bone loss after cervical Bryan disc arthroplasty: insight into the biomechanics following total disc replacement. Spine J 2020;20:1211-8. [Crossref] [PubMed]
- Kuo CH, Kuo YH, Wu JC, Chang HK, Ko CC, Tu TH, Chang CC, Yeh MY, Fay LY, Huang WC, Cheng H. Anterior Bone Loss in Cervical Disc Arthroplasty Correlates with Increased Cervical Lordosis. World Neurosurg 2022;163:e310-6. [Crossref] [PubMed]
- Wu TK, Liu H, Wang BY, He JB, Ding C, Rong X, Yang Y, Huang KK, Hong Y. Incidence of bone loss after Prestige-LP cervical disc arthroplasty: a single-center retrospective study of 396 cases. Spine J 2020;20:1219-28. [Crossref] [PubMed]
- Wang XF, Meng Y, Liu H, Wang BY, Hong Y. Incidence and outcomes of anterior bone loss in single-level Prestige LP cervical disc replacement. Chin Med J (Engl) 2020;134:109-11. [Crossref] [PubMed]
- Wang X, Meng Y, Liu H, Hong Y, Wang B. Is Anterior Bone Loss the Opposite of Anterior Heterotopic Ossification in Prestige-LP Cervical Disc Replacement? World Neurosurg 2020;136:e407-18. [Crossref] [PubMed]
- Scheer JK, Lau D, Smith JS, Lee SH, Safaee MM, Fury M, Ames CP. Alignment, Classification, Clinical Evaluation, and Surgical Treatment for Adult Cervical Deformity: A Complete Guide. Neurosurgery 2021;88:864-83. [Crossref] [PubMed]
- Sheng XQ, Meng Y, Liu H, Wang BY, Yang Y, Rong X, Hong Y. Is the fusion order of the cranial and caudal levels different in two-level anterior cervical discectomy and fusion for cervical spondylopathy? A retrospective study. J Orthop Surg Res 2021;16:500. [Crossref] [PubMed]
- Sheng XQ, Ding C, Wang BY, Meng Y, Liu H. Segmental Slope is a Predictor of Fusion Rate in Single Level Anterior Cervical Discectomy and Fusion. Global Spine J 2024;14:657-66. [Crossref] [PubMed]
- Wang X, Meng Y, Liu H, Chen H, Wang B, Hong Y. Cervical sagittal alignment after Prestige LP cervical disc replacement: radiological results and clinical impacts from a single-center experience. BMC Musculoskelet Disord 2021;22:82. [Crossref] [PubMed]
- Kao TH, Wu CH, Chou YC, Chen HT, Chen WH, Tsou HK. Risk factors for subsidence in anterior cervical fusion with stand-alone polyetheretherketone (PEEK) cages: a review of 82 cases and 182 levels. Arch Orthop Trauma Surg 2014;134:1343-51. [Crossref] [PubMed]
- Deng Y, Wang B, Hong Y, Yang Y, Xing R, Wang X, Liu H. Anterior bone loss: A common phenomenon which should be considered as bone remodeling process existed not only in patients underwent cervical disk replacement but also those with anterior cervical diskectomy and fusion. Eur Spine J 2023;32:977-85. [Crossref] [PubMed]
- Yonenobu K, Abumi K, Nagata K, Taketomi E, Ueyama K. Interobserver and intraobserver reliability of the japanese orthopaedic association scoring system for evaluation of cervical compression myelopathy. Spine (Phila Pa 1976) 2001;26:1890-4; discussion 1895. [Crossref] [PubMed]
- Chiarotto A, Maxwell LJ, Ostelo RW, Boers M, Tugwell P, Terwee CB. Measurement Properties of Visual Analogue Scale, Numeric Rating Scale, and Pain Severity Subscale of the Brief Pain Inventory in Patients With Low Back Pain: A Systematic Review. J Pain 2019;20:245-63. [Crossref] [PubMed]
- Walraevens J, Demaerel P, Suetens P, Van Calenbergh F, van Loon J, Vander Sloten J, Goffin J. Longitudinal prospective long-term radiographic follow-up after treatment of single-level cervical disk disease with the Bryan Cervical Disc. Neurosurgery 2010;67:679-87; discussion 687. [Crossref] [PubMed]
- Lou J, Wang B, Wu T, Wu W, Li H, Liu Z, Liu H. In-vivo study of osseointegration in Prestige LP cervical disc prosthesis. BMC Musculoskelet Disord 2018;19:42. [Crossref] [PubMed]
- Cunningham BW, Hu N, Zorn CM, McAfee PC. Bioactive titanium calcium phosphate coating for disc arthroplasty: analysis of 58 vertebral end plates after 6- to 12-month implantation. Spine J 2009;9:836-45. [Crossref] [PubMed]
- Hu N, Cunningham BW, McAfee PC, Kim SW, Sefter JC, Cappuccino A, Pimenta L. Porous coated motion cervical disc replacement: a biomechanical, histomorphometric, and biologic wear analysis in a caprine model. Spine (Phila Pa 1976) 2006;31:1666-73. [Crossref] [PubMed]
- Jensen WK, Anderson PA, Nel L, Rouleau JP. Bone ingrowth in retrieved Bryan Cervical Disc prostheses. Spine (Phila Pa 1976) 2005;30:2497-502. [Crossref] [PubMed]
- McAfee PC, Cunningham BW, Orbegoso CM, Sefter JC, Dmitriev AE, Fedder IL. Analysis of porous ingrowth in intervertebral disc prostheses: a nonhuman primate model. Spine (Phila Pa 1976) 2003;28:332-40. [Crossref] [PubMed]
- He M, Huang Y, Xu H, Feng G, Liu L, Li Y, Sun D, Zhang L. Modification of polyetheretherketone implants: From enhancing bone integration to enabling multi-modal therapeutics. Acta Biomater 2021;129:18-32. [Crossref] [PubMed]
- Frost HM A. 2003 update of bone physiology and Wolff's Law for clinicians. Angle Orthod 2004;74:3-15. [Crossref] [PubMed]
- Leven D, Meaike J, Radcliff K, Qureshi S. Cervical disc replacement surgery: indications, technique, and technical pearls. Curr Rev Musculoskelet Med 2017;10:160-9. [Crossref] [PubMed]
- Zaidi M, Turner CH, Canalis E, Pacifici R, Sun L, Iqbal J, Guo XE, Silverman S, Epstein S, Rosen CJ. Bone loss or lost bone: rationale and recommendations for the diagnosis and treatment of early postmenopausal bone loss. Curr Osteoporos Rep 2009;7:118-26. [Crossref] [PubMed]
- Powell CB, Alabaster A, Stoller N, Armstrong MA, Salyer C, Hamilton I, Raine-Bennett T. Bone loss in women with BRCA1 and BRCA2 mutations. Gynecol Oncol 2018;148:535-9. [Crossref] [PubMed]
- He J, Ding C, Liu H, Wu T, Huang K, Hong Y, Meng Y, Wang B. Does Fusion Affect Anterior Bone Loss in Adjacent Cervical Disc Arthroplasty in Contiguous Two-Level Hybrid Surgery? World Neurosurg 2020;143:e127-35. [Crossref] [PubMed]
- Lübbeke A, Garavaglia G, Barea C, Roussos C, Stern R, Hoffmeyer P. Influence of obesity on femoral osteolysis five and ten years following total hip arthroplasty. J Bone Joint Surg Am 2010;92:1964-72. [Crossref] [PubMed]
- Goldschmidt E, Angriman F, Agarwal N, Trevisan M, Zhou J, Chen K, et al. A New Piece of the Puzzle to Understand Cervical Sagittal Alignment: Utilizing a Novel Angle δ to Describe the Relationship among T1 Vertebral Body Slope, Cervical Lordosis, and Cervical Sagittal Alignment. Neurosurgery 2020;86:446-51. [Crossref] [PubMed]
- Rossanez R, de Rezende Pratali R, Smith JS, Nasreddine MA, Pereira da Silva Herrero CF. Internal Chain of Correlation of Sagittal Cervical Alignment in Asymptomatic Subjects. Global Spine J 2023;13:2439-45. [Crossref] [PubMed]
- Patwardhan AG, Khayatzadeh S, Nguyen NL, Havey RM, Voronov LI, Muriuki MG, Carandang G, Smith ZA, Sears W, Lomasney LM, Ghanayem AJ. Is Cervical Sagittal Imbalance a Risk Factor for Adjacent Segment Pathomechanics After Multilevel Fusion? Spine (Phila Pa 1976) 2016;41:E580-8. [Crossref] [PubMed]


