
Transcatheter arterial embolization using n-butyl cyanoacrylate–Lipiodol mixture and metallic coils in a patient with biliary hemorrhage after removing a bile duct metallic stent: a case description
Introduction
Although biliary hemorrhage is rare, its frequency has increased in recent years owing to the increasing application of minimally invasive procedures in the hepatobiliary and pancreatic regions (1). The frequency of iatrogenic biliary hemorrhage has been reported to be 65% (1). The main causes of biliary hemorrhage are percutaneous transhepatic treatment, surgical procedures within the hepatic hilum, and endoscopic placement of bile duct stents (2,3). Feng et al. reported that hemorrhage occurred from the hepatic artery in all 30 cases that underwent percutaneous transhepatic treatment or surgical procedure of the hepatic hilum (2). Kim et al. described that hemorrhage occurred from the hepatic artery in 15 of 19 patients who underwent endoscopic bile duct stenting, from the gastroduodenal artery in 3 patients, and from the posterior superior pancreaticoduodenal artery (PSPDA) in 1 patient (3). By contrast, biliary hemorrhage after removing a bile duct stent is extremely rare, and hemostasis was achieved using a covered stent in all prior reports (4). To the best of our knowledge, this is the first reported case of biliary hemorrhage after removing a metallic bile duct stent that was embolized using n-butyl-cyanoacrylate (NBCA)–Lipiodol mixture and metallic coils.
Case presentation
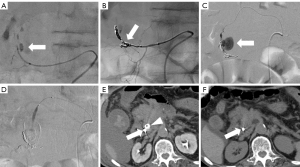
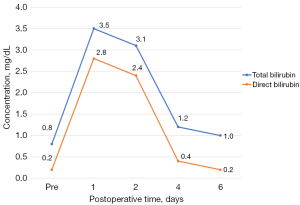
The patient, a male in his 70s, had previously undergone transpapillary implantation of a bare metal stent (BONASTENT® 10 mm/6 cm, MEDICO’S HIRATA Inc., Osaka, Japan) to treat obstructive cholangitis caused by a pancreatic head tumor. Biopsy revealed diffuse large B-cell lymphoma and chemotherapy was performed. Because chemotherapy reduced the size of the pancreatic head tumor by 56%, the stent was removed using forceps 38 days after the end of chemotherapy. There was no obvious hemorrhage immediately after removing the stent. However, 3 hours after stent removal, he developed extensive melena and abdominal pain. Because abdominal contrast-enhanced computed tomography showed a 9 mm pseudoaneurysm in the common bile duct (Figure 1A) and his blood pressure was decreased, transcatheter arterial embolization was performed. A 4 Fr sheath (Radifocus Introducer II H, Terumo Clinical Supply, Gifu, Japan) was inserted via the right femoral artery, and a 4 Fr catheter (Pig tail, Medikit, Tokyo, Japan) was inserted for computed tomography during aortography. The three-dimensional reconstructed images indicated that the posterior pancreaticoduodenal artery was responsible for the pseudoaneurysm (Figure 1B). First, a 4 Fr guiding catheter (RC2, Medikit, Tokyo, Japan or 1CJ, Hanako Medical, Saitama, Japan) was inserted to cannulate the superior mesenteric artery. The posterior inferior pancreaticoduodenal artery was embolized with three metallic coils (Target XL 2 mm/6 cm, Boston Scientific, Natick, MA, USA) as close as possible to the pseudoaneurysm using a microcatheter (Tellus, Asahi intecc, Aichi, Japan; Figure 2A,2B). Next, a 4 Fr guiding catheter was cannulated into the celiac artery, but it was difficult to advance the microcatheter close to the pseudoaneurysm due to spasm of the PSPDA. To avoid proximal embolization, NBCA (Histoacryl®, B. Braun, Melsungen, Germany)–Lipiodol (Ultra-Fluide®, Guerbet, Roissy, France) mixture (NBCA:Lipiodol =1:3) was injected to embolize the PSPDA (Figure 2C,2D). Angiography after embolization showed no obvious extravascular leakage of contrast medium and his blood pressure increased. The immediate postoperative computed tomography showed a high attenuating area in the common bile duct consistent with the NBCA–Lipiodol mixture (Figure 2E). Non-contrast computed tomography on postoperative day 4 showed that the NBCA–Lipiodol mixture had disappeared from the common bile duct and was excreted into the duodenum (Figure 2F). His total bilirubin and direct bilirubin levels were elevated on postoperative day 1, and had decreased to normal levels on postoperative day 4 (Figure 3). Postoperatively, the patient’s anemia and cholangitis improved, and there was no evidence of pancreatitis or organ necrosis. The patient was transferred to another hospital 2 months later.

All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committees and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
The clinical success rate of transcatheter arterial embolization for biliary hemorrhage is high, ranging from 80% to 100%, and it is a treatment that should be actively considered for such events (5). Liquid embolic materials such as NBCA and metallic coils are often used for embolization of biliary hemorrhage (6,7). Advantages of NBCA are that embolization is independent of its coagulation ability and it allows a shorter procedure time. However, because of its liquid property, it is difficult to control the extent of embolization, and there is a risk that liquid embolic materials may inflow into non-target areas. It was reported that NBCA–Lipiodol mixtures with lower concentrations of NBCA are more likely to reach distal sites (8,9). Therefore, in this patient, it was deemed necessary to increase the NBCA concentration in the NBCA–Lipiodol mixture to prevent inflow into the common bile duct. However, in a prior study of aneurysms, it was reported that migration was less likely to occur if the NBCA concentration was ≥30% (10). In other words, if the concentration of NBCA exceeds 30%, polymerization of NBCA can be too fast or too hard (11,12). For these reasons, we used NBCA–Lipiodol mixture comprising 25% NBCA for embolization of the biliary hemorrhage. Excretion of the NBCA–Lipiodol mixture into the duodenum was observed 4 days after embolization. Although a liquid embolic material was chosen due to spasm of the PSPDA, embolization with metallic coils was preferred because of the risk of inflow of the embolic material into the common bile duct.
Conclusions
This rare case of biliary hemorrhage, which occurred after removing a metallic stent from the bile duct, demonstrates that hemostasis can be achieved by transcatheter arterial embolization using NBCA–Lipiodol mixture and metallic coils.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-22-95/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committees and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Zhornitskiy A, Berry R, Han JY, Tabibian JH. Hemobilia: Historical overview, clinical update, and current practices. Liver Int 2019;39:1378-88. [Crossref] [PubMed]
- Feng W, Yue D. ZaiMing L, ZhaoYu L, XiangXuan Z, Wei L, QiYong G. Iatrogenic hemobilia: imaging features and management with transcatheter arterial embolization in 30 patients. Diagn Interv Radiol 2016;22:371-7. [Crossref] [PubMed]
- Kim PH, Kim JW, Gwon DI, Ko GY, Shin JH, Yoon HK. Embolization for delayed arterial bleeding after percutaneous self-expandable metallic stent placement in patients with malignant biliary obstruction. Br J Radiol 2020;93:20190637. [Crossref] [PubMed]
- Fujimori N, Matsumoto K, Murakami M, Suehiro Y, Oono T. Endoscopic tamponade using a fully covered self-expandable metallic stent for massive biliary bleeding from a pseudoaneurysm rupture during metallic stent removal. VideoGIE 2020;6:24-6. [Crossref] [PubMed]
- Choi SH, Gwon DI, Ko GY, Sung KB, Yoon HK, Shin JH, Kim JH, Kim J, Oh JY, Song HY. Hepatic arterial injuries in 3110 patients following percutaneous transhepatic biliary drainage. Radiology 2011;261:969-75. [Crossref] [PubMed]
- Shi Y, Chen L, Zhao B, Huang H, Lu Z, Su H. Transcatheter arterial embolization for massive hemobilia with N-butyl cyanoacrylate (NBCA) Glubran 2. Acta Radiol 2022;63:360-7. [Crossref] [PubMed]
- Hong Duc P, Xuan Dung P, Quang Huy H. Post-Blunt Traumatic Hemobilia From Pseudoaneurysm Successfully Treated With Embolization. Cureus 2020;12:e7961. [Crossref] [PubMed]
- Takasawa C, Seiji K, Matsunaga K, Matsuhashi T, Ohta M, Shida S, Takase K, Takahashi S. Properties of N-butyl cyanoacrylate-iodized oil mixtures for arterial embolization: in vitro and in vivo experiments. J Vasc Interv Radiol 2012;23:1215-21.e1. [Crossref] [PubMed]
- Sonomura T, Kawai N, Ikoma A, Minamiguchi H, Ozaki T, Kishi K, Sanda H, Nakata K, Nakai M, Muragaki Y, Sato M. Uterine damage in swine following uterine artery embolization: comparison among gelatin sponge particles and two concentrations of N-butyl cyanoacrylate. Jpn J Radiol 2013;31:685-92. [Crossref] [PubMed]
- Hama M, Sonomura T, Ikoma A, Koike M, Kamisako A, Tanaka R, Koyama T, Sato H, Tanaka F, Ueda S, Okuhira R, Warigaya K, Murata S, Nakai M. Balloon-Assisted Embolization of Wide-Neck Aneurysms Using a Mixture of n-Butyl Cyanoacrylate, Lipiodol, and Ethanol in Swine: A Comparison of Four n-Butyl Cyanoacrylate Concentrations. Cardiovasc Intervent Radiol 2020;43:1540-7. [Crossref] [PubMed]
- Higashino N, Sonomura T, Fukuda K, Ikoma A, Okuhira R, Ueda S, Kawai N. Feasibility and Safety of n-Butyl Cyanoacrylate-Lipiodol-Iopamidol as an Alternative Liquid Embolic Material. Cardiovasc Intervent Radiol 2021;44:482-8. [Crossref] [PubMed]
- Fukuda K, Higashino N, Sonomura T, Okuhira R, Koike M, Ikoma A, Kawai N, Minamiguchi H. Determination of the optimal ratio and the relationship between viscosity and adhesion of n-butyl cyanoacrylate-Lipiodol-iopamidol for balloon-assisted embolization of wide-neck aneurysms in swine. Cardiovasc Intervent Radiol 2022;45:357-64. [Crossref] [PubMed]


