
Oral effervescent agent improving magnetic resonance cholangiopancreatography
Introduction
Magnetic resonance cholangiopancreatography (MRCP) is the modality of choice for noninvasive imaging evaluation in patients with known or suspected pancreatobiliary disease (1-6). The two-dimensional (2D) MRCP basically relies on heavily T2-weighted sequences to accentuate fluid within the pancreatobiliary ductal system. Because of the proximity of the stomach and duodenum to the pancreatobiliary tree and the projectional nature of these images, 2D MRCP sequence has the potential technical limitation that the hyperintense intraluminal fluid signal within the adjacent stomach or duodenum may superimpose upon the pancreatobiliary tree, hindering comprehensive evaluation of this system (7-11). To overcome this drawback, some kinds of juice or syrup (including acai, blueberry, pineapple juice, and data syrup) has been proposed as the oral negative contrast agents to effectively decrease the high signal of the gastrointestinal tract (7,8,12-15) and improve MRCP image quality, but it is unfortunately not easy to get in such large volumes for clinical practice. Recently, it has been shown that oral administration of the effervescent agent can improve MRCP images, both qualitatively and quantitatively, for the purpose of biliary anatomy evaluation in the living liver donors (1). In this study, we aimed to validate the improvement of MRCP with oral administration of the oral effervescent agent in the patients with known or suspected pancreatobiliary disease.
Methods
The institutional review board of Kangbuk Samsung Hospital approved this study. Owing to the retrospective nature of the study, the informed patient consent was waived. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Study population
For 21 months, 115 consecutive patients visiting a tertiary hospital were referred for MRCP for the evaluation of alleged or suspected pancreatobiliary tree problems. At our hospital, we obtained MRCP images not only before but also after oral effervescent enhancement, without additional cost, based on the previous studies (1,16) and agreement of hepatobiliary clinicians. Four of these subjects who failed to MRCP imaging with the administration of oral effervescent agent were excluded from the study, as they could not swallow it. Thus, 111 patients [mean age ± standard deviation (SD), 54.0±15.3 years; range, 14–82 years; 54 men (mean age, 56.1±17.3 years; range, 27–82 years) and 57 women (mean age, 52.1±13.0 years; range, 14–76 years)] who underwent successive MRCP imaging before and after oral effervescent enhancement were finally included.
MRCP technique
Patients were fasted for >6 h before the MRCP examinations. MR imaging was performed at 3.0 Tesla scanner (Intera Achieva, Philips, Best, The Netherlands) equipped with dedicated 32-channel phased array coil, providing a gradient strength up to 80 mT/m and a peak slew rate of 200 mT/m/s.
After acquisition of breath-hold T2-weighted fast spin echo, MRCP was successively performed without and with oral effervescent enhancement (conventional-MRCP and enhanced-MRCP, respectively). The scan parameters for routine thick-slab breath-hold 2D MRCP imaging (single-shot rapid acquisition with relaxation enhancement sequence) were as follows: repetition time, 5,634 ms; echo time, 920 ms; refocusing flip angle, 90-degree; field of view, 220×220 mm; matrix size, 224×225; slab thickness, 40 mm. After first conventional-MRCP, the patient took a pack of oral effervescent agent (Top Effervescent-G Granules, Taejoon Pharm., Seoul, Korea) and scanty water (<10 mL). The second enhanced-MRCP imaging was done in the position of slight (30°) left lateral decubitus with same parameters with first MRCP imaging. For both MRCP sets, ten slabs of images were obtained in the coronal oblique planes (rotation in 18° increments).
Image analysis
The MRCP images were first anonymized and uploaded in the Picture Archiving Communication System (PACS). Two subspecialty-trained abdominal radiologists (KAK and HJK), each with 5- and 12-year clinical experience with abdominal MR imaging, independently reviewed MRCP images in two separate reading sessions by using a PACS workstation monitor. Both readers were blinded to any clinical and imaging information. At the first session, a total of 222 sets of MRCP [two image sets (conventional-MRCP and enhanced-MRCP) for each 111 subjects] were displayed in a random order (i.e., patient one with enhanced-MRCP, then patient 38 with conventional-MRCP). Based on the degrees of image artifacts and the visualization of the bile duct and pancreatic duct (PD), overall image quality of each MRCP set was graded as follows: 1 (poor), massive artifacts or image blurring that make the evaluation of the biliary duct and PD impossible; 2 (fair), moderate artifacts and image blurring that substantially interfere with evaluation of those structures; 3 (good), minor artifacts without substantial interference with duct visualization; and 4 (excellent), excellent image sharpness with lack of artifacts. The readers also evaluated the visibility of ductal segments divided as follows: the right and left intrahepatic duct (RHD and LHD), common hepatic duct (CHD), proximal and distal common bile duct (pCBD and dCBD; the upper and the lower half, respectively), PD at head, body, and tail (hPD, bPD, and tPD; the right part of left border of superior mesenteric vein, the part between head and tail, and the left part of left border of the aorta, respectively), cystic duct (CD), and gallbladder (GB). The visibility of segmental ductal structures was graded as follows: 1 (poor), non-visualization (impossible detection); 2 (fair), partial visualization; 3 (good), mostly visualized; and 4 (excellent), perfect visualization of the entire system. Gastroduodenal fluid signal score was determined by assessing whether the fluid signal of any part of the stomach or duodenum overlapped the biliary duct and PD and whether it was hindering the reading, as follows: 1 (poor), high signal intensity of the gastroduodenal fluid affected the reading; 2 (good), gastroduodenal fluid was overlapping part of the biliary duct and PD but did not affect the reading; 3 (excellent), no remarkable overlap. With an interval of 4 weeks and blinded to the results of the first review session, the second independent review session was performed to determine the preference of the reviewers. With a randomized order, conventional- and enhanced-MRCP image sets for each subject were compared side-by-side.
Subsequently, in consensus, the reviewers recorded the presence of gastroduodenal fluids in anatomic segments (fundus, body, and antrum of the stomach, bulb and 2nd portion of the duodenum) on both conventional- and enhanced-MRCP and overlapping of the pancreatobiliary tree. In detail for the ten ductal segments, the number of images where the gastroduodenal fluid overlapped was counted on conventional- and enhanced-MRCP.
Statistical analyses
We used commercially available SPSS software version 24.0 (SPSS, Chicago, IL, USA) and MedCalc version 16.2.1 software for Windows (Medcalc Software, Mariakeke, Belgium) for statistical analyses. The parameters were presented as mean ± SD. Between conventional- and enhanced-MRCP sets, the qualitative values were compared by paired Wilcoxon’s signed-rank and McNemar tests, and quantitative parameters were compared by a paired t-test. Values for P<0.05 were considered to be statistically significant.
Results
Table 1 and Figure 1 present and illustrate the grades of the overall image quality, the scores of the biliary duct and PD visualization for the targeted ten segments (RHD, LHD, CHD, pCBD, dCBD, hPD, bPD, tPD, CD, and GB), and gastroduodenal fluid signal scores on conventional- and enhanced-MRCP. The overall image quality improved after oral effervescent enhancement with a statistically significance (P<0.001 in both readers). The biliary duct and PD visualization scores for targeted ten segments were significantly higher on enhanced-MRCP than on conventional-MRCP for both reviewers (P≤0.02) except for bPD (P≥0.46) and tPD (P≥0.07). The gastroduodenal fluid signal scores on MRCP images increased significantly after oral administration of effervescent agent (P<0.001 in both readers). Between two MRCP images, both readers more often preferred enhanced-MRCP (reader 1: 93/111, 83.8%; reader 2, 96/111, 86.5%; P<0.001).
Table 1
| Parameter | Reader 1 | Reader 2 | |||||
|---|---|---|---|---|---|---|---|
| Conventional-MRCP† | Enhanced-MRCP† | P value | Conventional-MRCP† | Enhanced-MRCP† | P value | ||
| Overall image quality | 2.93±0.747 | 3.37±0.7 | <0.001 | 3.05±0.796 | 3.68±0.590 | <0.001 | |
| Visibility of ten ductal segments | |||||||
| RHD | 3.59±0.609 | 3.83±0.465 | <0.001 | 3.81±0.611 | 3.94±0.411 | 0.004 | |
| LHD | 3.51±0.586 | 3.71±0.578 | 0.001 | 3.85±0.446 | 3.95±0.314 | 0.008 | |
| CHD | 3.69±0.569 | 3.9±0.380 | <0.001 | 3.56±0.670 | 3.92±0.306 | <0.001 | |
| pCBD | 3.69±0.615 | 3.87±0.407 | 0.002 | 3.55±0.806 | 3.86±0.393 | <0.001 | |
| dCBD | 3.62±0.604 | 3.77±0.480 | 0.01 | 3.76±0.508 | 3.89±0.366 | 0.01 | |
| hPD | 3.02±0.853 | 3.29±0.743 | <0.001 | 3.34±0.939 | 3.6±0.778 | 0.006 | |
| bPD | 2.81±1.066 | 2.72±1.138 | 0.46 | 2.93±1.118 | 2.91±1.218 | 0.91 | |
| tPD | 2.33±0.985 | 2.49±1.043 | 0.09 | 2.46±1.234 | 2.68±1.348 | 0.07 | |
| CD | 2.59±0.967 | 2.91±1.036 | 0.001 | 2.94±1.057 | 3.41±1.002 | <0.001 | |
| GB | 3.58±0.729 | 3.72±0.727 | 0.02 | 3.72±0.673 | 3.86±0.593 | 0.005 | |
| Gastroduodenal fluid signal score | 2.08±0.525 | 2.76±0.448 | <0.001 | 1.85±0.618 | 2.76±0.490 | <0.001 | |
†, data are expressed as mean ± SD. Conventional-MRCP, magnetic resonance cholangiopancreatography without oral effervescent agent; Enhanced-MRCP, magnetic resonance cholangiopancreatography with oral effervescent agent; RHD, right intrahepatic duct; LHD, left intrahepatic duct; CHD, common hepatic duct; pCBD, proximal common bile duct; dCBD, distal common bile duct; hPD, pancreatic duct at head; bPD, pancreatic duct at body; tPD, pancreatic duct at tail; CD, cystic duct; GB, gallbladder; SD, standard deviation.
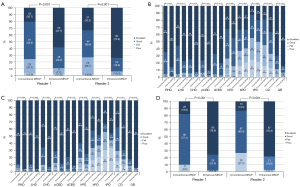
Table 2 shows the locations of gastroduodenal fluids on conventional- and enhanced-MRCP. On enhanced-MRCP images, the gastroduodenal fluids were less detected rather than those on conventional-MRCP, except for gastric fundus. Gastroduodenal fluids overlapping the extrahepatic bile duct were mainly at the gastric antrum, duodenal bulb, and duodenal 2nd portion on conventional-MRCP. And, these fluids were less overlapped on enhanced-MRCP (all P<0.001, Table 3, Figure 2). Gastroduodenal fluids at the gastric body and antrum mainly overlapped the PD on conventional-MRCP, and the fluid in these locations significantly less overlapped the PD on enhanced-MRCP (P≤0.02, Table 3). In detail for the ten targeted ductal segments, numbers of the MRCP images with the gastroduodenal fluid overlapping each duct segments (except for RHD and LHD) and for overall pancreatobiliary duct were significantly different between conventional- and enhanced-MRCP (P≤0.037, Table 4).
Table 2
| Anatomic locations with intestinal fluids distribution | Conventional-MRCP† | Enhanced-MRCP† | P value |
|---|---|---|---|
| Gastric fundus | 98 (88.3) | 105 (94.6) | 0.09 |
| Gastric body | 69 (62.2) | 38 (34.2) | <0.001 |
| Gastric antrum | 54 (48.6) | 7 (6.3) | <0.001 |
| Duodenal bulb | 75 (67.6) | 14 (12.6) | <0.001 |
| Duodenal 2nd portion | 101 (91.0) | 42 (37.8) | <0.001 |
†, data are expressed as number of patient (percentage). Conventional-MRCP, magnetic resonance cholangiopancreatography without oral effervescent agent; Enhanced-MRCP, magnetic resonance cholangiopancreatography with oral effervescent agent.
Table 3
| Overlapping structures | Conventional-MRCP† | Enhanced-MRCP† | P value |
|---|---|---|---|
| Extrahepatic duct | |||
| Gastric fundus | 1 (0.9) | 0 | – |
| Gastric body | 0 | 0 | – |
| Gastric antrum | 38 (34.2) | 3 (2.7) | <0.001 |
| Duodenal bulb | 66 (59.5) | 7 (6.3) | <0.001 |
| Duodenal 2nd portion | 70 (63.1) | 24 (21.6) | <0.001 |
| Pancreatic duct | |||
| Gastric fundus | 8 (7.2) | 9 (8.1) | 1.00 |
| Gastric body | 26 (23.4) | 14 (12.6) | 0.02 |
| Gastric antrum | 17 (15.3) | 2 (1.8) | <0.001 |
| Duodenal bulb | 1 (0.9) | 1 (0.9) | 1.00 |
| Duodenal 2nd portion | 8 (7.2) | 2 (1.8) | 0.07 |
†, data are expressed as number of patient (percentage). PD, pancreatic duct; Conventional-MRCP, magnetic resonance cholangiopancreatography without oral effervescent agent; Enhanced-MRCP, magnetic resonance cholangiopancreatography with oral effervescent agent.

Table 4
| Parameter | Conventional-MRCP† | Enhanced-MRCP† | P value |
|---|---|---|---|
| RHD | 0.09±0.48 | 0.00 | 0.13 |
| LHD | 0.08±0.44 | 0.00 | 0.13 |
| CHD | 2.34±2.85 | 0.29±0.85 | <0.001 |
| pCBD | 4.07±3.34 | 0.61±1.37 | <0.001 |
| dCBD | 0.79±1.63 | 0.41±1.01 | 0.04 |
| hPD | 0.48±1.50 | 0.12±0.48 | 0.003 |
| bPD | 0.79±1.77 | 0.09±0.45 | <0.001 |
| tPD | 1.46±2.17 | 0.58±1.42 | <0.001 |
| CD | 3.29±2.97 | 0.51±1.42 | <0.001 |
| GB | 1.65±2.09 | 0.29±0.92 | <0.001 |
| Total | 6.36±2.72 | 1.56±2.06 | <0.001 |
†, data are expressed as mean ± SD. Conventional-MRCP, magnetic resonance cholangiopancreatography without oral effervescent agent; Enhanced-MRCP, magnetic resonance cholangiopancreatography with oral effervescent agent; RHD, right intrahepatic duct; LHD, left intrahepatic duct; CHD, common hepatic duct; pCBD, proximal common bile duct; dCBD, distal common bile duct; hPD, pancreatic duct at head; bPD, pancreatic duct at body; tPD, pancreatic duct at tail; CD, cystic duct; GB, gallbladder; SD, standard deviation.
Discussion
MRCP is a safe and noninvasive method of evaluating the pancreatobiliary system, providing the similar images of the pancreatobiliary tree to those by endoscopic retrograde pancreatography without the associated complications and morbidity (2,3,17-19). Although MRCP has been shown the high accuracy in the diagnosing of the stone, malignancy, and congenital anomalies in the biliary duct, it is important to be aware of potential pitfalls (9,10). The main limitations of MRCP are breathing artifacts, poor spatial resolution, and superimposition by gastrointestinal tract signals (7,9). Any kind of effort to improve the image quality might be valuable to reduce the indecisive cases on MRCP, particularly because of the high cost and the lack of noninvasive alternative method. Technical development and refinement of MR sequences have reduced the degree of artifacts and improved resolution, thereby overcoming the limitations to a great extent. Nevertheless, signal from the intestinal fluids superimposing on the pancreatobiliary ductal system remains a major problem that interferes with the interpretation. Our results show that oral administration of effervescent agent can allow appropriated evaluation of the pancreatobiliary tree, unimpeded by overlapping signals from the neighboring gastroduodenal fluid-signals.
In our study, enhanced-MRCP showed statistically significant superiority over conventional-MRCP in terms of the overall image quality, most of the visibility of ductal segments except for bPD and tPD, and gastroduodenal fluid signal score by both of the two reviewers. However, in practice, these differences would not be clinically significant because the differences between conventional- and enhanced-MRCP seems not to be considerable. Grossly, overlapping of the pancreatobiliary ductal system by the gastroduodenal fluid obscured the extrahepatic duct, including CHD, CBD, CD, GB, and PD, because of its close relation to the gastric antrum and duodenum, in 4.8–63.6% of conventional-MRCP and in 0.9–15.6% of enhanced-MRCP, indicating statistically significant improvement (P<0.001). On the other hand, because the intrahepatic bile duct is a little bit cranial to the level of the gastric antrum and duodenum, it was less affected by gastroduodenal fluid signal (0.8–0.9% of conventional-MRCP and none of enhanced-MRCP). In case of PD, while the numbers of MRCP images where the gastroduodenal fluid overlapped PD were decreased with enhanced-MRCP compared with conventional-MRCP, the visualization scores decreased on enhanced-MRCP, although there was no statistical significance (P≥0.457). This result is correlated with the result of previous study using oral effervescent agent for MRCP (16). We propose that is maybe due to the distended stomach body compressed the pancreas body, causing the decrease of caliber of PD.
Several negative oral contrast agents for MRCP that render the bowel signal dark on T2-weighted sequences are commercially available [i.e., ferumoxsil (GastroMARK; Mallinckrodt Inc., Raleigh, NC, USA), manganese chloride, barium sulfate, and ferric particles] (20,21). Previous studies using these agents also showed the correlative results with our study for the improvement of visibility of biliary ducts. However, these agents may be expensive, unpalatable, and may have adverse effects (8). Also, there are several studies that fruit juices such as acai, blueberry, or pineapple juices, and data syrup can be used as the oral negative agent with partial decrease of the background noise and improvement of the quality of MRCP (7,8,12-15). However, these fruit juices in its natural pure form are not readily available and commercially available packs contain varying degree of dilutions of juice with variable manganese levels, and the patient may have to drink a lot of it, limiting the clinical application for ill patients (7,8,12,22,23). Data syrup is viscous and a previous study showed that it needed about 30 min of the waiting time to coat the stomach and duodenum after consumption (14). In our study, we used effervescent agent as a negative oral contrast for MRCP, which is routinely used for double-contrast upper gastrointestinal studies with no significant risk of the side effect except for the temporary discomfort during the swallowing. The use of oral effervescent agent is relatively convenient with a fairly low administrating volume to avoid this drawback. Previous studies have shown that it is safe and effective as negative oral contrast agent for MRCP (1,16).
Recently, contrast-enhanced T1 MRCP using gadolinium ethoxybenzyl-diethylenetriamine pentaacetic acid (Gd-EOB-DTPA, Primovist® in Europe and Eovist® in the USA) is highlighted as a useful sequence for evaluating the biliary anatomy (24,25). The 2015 European society of gastrointestinal and abdominal radiology consensus statement recommends obtaining contrast-enhanced MRCP with Gd-EOB-DTPA at 20 min after injection in subjects without significant hepatobiliary dysfunction (26), although the use of Gd-EOB-DTPA demands high cost and has not been permitted in children under 18 years of age. Additionally, T2 MRCP imaging can be performed as part of a contra-enhanced MRI exam. Most MRI contrast agents available for intravenous use contain gadolinium, and several contrasts, such as gadobenate dimeglumine (MultiHance®) or Gd-EOB-DTPA, has biliary excretion. According to the recent study (27), 2D MRCP should be performed before or within short time after intravenous injection of contrast agent, because the biliary excretion of these contrast agent could potentially degrade MRCP image quality, causing significant biliary duct signal degradation due to gadolinium’s shortening of T2 relaxation time in excreted bile.
There are several limitations to our study. The first limitation of this study is its inherent nature of the retrospective study. Concerns remain the possibility of an inevitable patient selection bias due to its retrospective design. Second, as we evaluated the effect of an oral effervescent agent on 2D MRCP only, our results might have some limitations in being generalized to other MRCP imaging protocols, such as intravenous contrast-enhanced MRCP or three-dimensional (3D) MRCP. 3D MRCP is commonly applied due to its advantages including better anatomic depiction and a higher signal-to-noise ratio, compared with 2D MRCP. According to recent study (28), 3D MRCP outperformed 2D MRCP to visualize the CHD and CBD, but compared inferiorly in the RHD and tPD. However, the results of our study might not be generalizable to 3D MRCP because of the difficulty to predict the effect of oral effervescent agent to its main drawback such as motion artifact resulting in unsatisfactory image quality. To evaluate the effect of the effervescent agent on 3D MRCP or other MRCP imaging protocols, further studies would be needed. Third, in some patient, the sufficient amount of air might not be produced because of relatively small amount or slow ingestion of oral agent. However, it could be overcome by adapting the amount of oral agent according to the patient or assuming the agent faster. Forth, for the enhanced-MRCP imaging, the position of the patients was changed to slight left lateral decubitus, which may introduce bias into the results of this study for the evaluation of the effect of the oral effervescent agent and the discomfort in patients caused by decubitus placement. However, this postural change could be helpful in the reduction of the discomfort such as burp or reflux, resulting in the safe and successful MRCP imaging.
In conclusion, oral administration of the effervescent agent provided an effective elimination of the gastroduodenal fluid overlapping the pancreatobiliary ductal system at MRCP and can improve the quality of the examination without significant additional cost in the patients with known or suspected pancreatobiliary disease. Therefore, we propose the use of oral effervescent agent as a strategy for the image quality improvement of MRCP examination, especially in case of the patient with poor MRCP image quality due to the overlapping gastroduodenal fluid signal.
Acknowledgments
Funding: This research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF), funded by the Ministry of Science, ICT and Future Planning (No. 2017R1E1A1A03070961). This work was also supported by the Medical Research Funds from Kangbuk Samsung Hospital.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-22-219/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional board of Kangbuk Samsung Hospital and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kwon HJ, Kim KW, Choi SH, Jung JH, Kim SY, Kim SY, Lee J, Jung DH, Ha TY, Song GW, Lee SG. MR cholangiography in potential liver donors: quantitative and qualitative improvement with administration of an oral effervescent agent. J Magn Reson Imaging 2017;46:1656-63. [Crossref] [PubMed]
- Soto JA, Barish MA, Yucel EK, Siegenberg D, Ferrucci JT, Chuttani R. Magnetic resonance cholangiography: comparison with endoscopic retrograde cholangiopancreatography. Gastroenterology 1996;110:589-97. [Crossref] [PubMed]
- Chan YL, Chan AC, Lam WW, Lee DW, Chung SS, Sung JJ, Cheung HS, Li AK, Metreweli C. Choledocholithiasis: comparison of MR cholangiography and endoscopic retrograde cholangiography. Radiology 1996;200:85-9. [Crossref] [PubMed]
- Fitoz S, Erden A, Boruban S. Magnetic resonance cholangiopancreatography of biliary system abnormalities in children. Clin Imaging 2007;31:93-101. [Crossref] [PubMed]
- Barish MA, Yucel EK, Soto JA, Chuttani R, Ferrucci JT. MR cholangiopancreatography: efficacy of three-dimensional turbo spin-echo technique. AJR Am J Roentgenol 1995;165:295-300. [Crossref] [PubMed]
- Fulcher AS, Turner MA, Capps GW, Zfass AM, Baker KM. Half-Fourier RARE MR cholangiopancreatography: experience in 300 subjects. Radiology 1998;207:21-32. [Crossref] [PubMed]
- Riordan RD, Khonsari M, Jeffries J, Maskell GF, Cook PG. Pineapple juice as a negative oral contrast agent in magnetic resonance cholangiopancreatography: a preliminary evaluation. Br J Radiol 2004;77:991-9. [Crossref] [PubMed]
- Bittman ME, Callahan MJ. The effective use of acai juice, blueberry juice and pineapple juice as negative contrast agents for magnetic resonance cholangiopancreatography in children. Pediatr Radiol 2014;44:883-7. [Crossref] [PubMed]
- Hirohashi S, Hirohashi R, Uchida H, Kitano S, Ono W, Ohishi H, Nakanishi S. MR cholangiopancreatography and MR urography: improved enhancement with a negative oral contrast agent. Radiology 1997;203:281-5. [Crossref] [PubMed]
- Irie H, Honda H, Kuroiwa T, Yoshimitsu K, Aibe H, Shinozaki K, Masuda K. Pitfalls in MR cholangiopancreatographic interpretation. Radiographics 2001;21:23-37. [Crossref] [PubMed]
- David V, Reinhold C, Hochman M, Chuttani R, McKee J, Waxman I, Wang L, Li W, Kaplan R, Edelman RR. Pitfalls in the interpretation of MR cholangiopancreatography. AJR Am J Roentgenol 1998;170:1055-9. [Crossref] [PubMed]
- Hiraishi K, Sagami A, Hisada Y, Yamamoto K, Saika Y, Adachi I, Fujita O, Narabayashi I, Hasegawa H. Contrast enhancement effect of new oral agent (blueberry juice) for upper abdominal MR imaging. Nihon Igaku Hoshasen Gakkai Zasshi 1994;54:539-41. [PubMed]
- Mohabir S, Pitcher RD, Perumal R, Goodier MDM. The efficacy of pineapple juice as a negative oral contrast agent in magnetic resonance cholangiopancreatography. SA J Radiol 2020;24:1875. [Crossref] [PubMed]
- Govindarajan A, Lakshmanan PM, Sarawagi R, Prabhakaran V. Evaluation of date syrup as an oral negative contrast agent for MRCP. AJR Am J Roentgenol 2014;203:1001-5. [Crossref] [PubMed]
- Papanikolaou N, Karantanas A, Maris T, Gourtsoyiannis N. MR cholangiopancreatography before and after oral blueberry juice administration. J Comput Assist Tomogr 2000;24:229-34. [Crossref] [PubMed]
- Chen CW, Liu YS, Chen CY, Tsai HM, Chen SC, Chuang MT. Use of carbon dioxide as negative contrast agent for magnetic resonance cholangiopancreatography. World J Radiol 2011;3:47-50. [Crossref] [PubMed]
- Ong TZ, Khor JL, Selamat DS, Yeoh KG, Ho KY. Complications of endoscopic retrograde cholangiography in the post-MRCP era: a tertiary center experience. World J Gastroenterol 2005;11:5209-12. [PubMed]
- Koito K, Namieno T, Ichimura T, Yama N, Hareyama M, Morita K, Nishi M. Mucin-producing pancreatic tumors: comparison of MR cholangiopancreatography with endoscopic retrograde cholangiopancreatography. Radiology 1998;208:231-7. [Crossref] [PubMed]
- Calvo MM, Bujanda L, Calderón A, Heras I, Cabriada JL, Bernal A, Orive V, Astigarraga E. Comparison between magnetic resonance cholangiopancreatography and ERCP for evaluation of the pancreatic duct. Am J Gastroenterol 2002;97:347-53. [Crossref] [PubMed]
- Polakova K, Mocikova I, Purova D, Tucek P, Novak P, Novotna K, Izak N, Bielik R, Zboril R, Miroslav H. Magnetic resonance cholangiopancreatography (MRCP) using new negative per-oral contrast agent based on superparamagnetic iron oxide nanoparticles for extrahepatic biliary duct visualization in liver cirrhosis. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub 2016;160:512-7. [Crossref] [PubMed]
- Chan JH, Tsui EY, Yuen MK, Szeto ML, Luk SH, Wong KP, Wong NO. Gadopentetate dimeglumine as an oral negative gastrointestinal contrast agent for MRCP. Abdom Imaging 2000;25:405-8. [Crossref] [PubMed]
- Hiraishi K, Narabayashi I, Fujita O, Yamamoto K, Sagami A, Hisada Y, Saika Y, Adachi I, Hasegawa H. Blueberry juice: preliminary evaluation as an oral contrast agent in gastrointestinal MR imaging. Radiology 1995;194:119-23. [Crossref] [PubMed]
- Duarte JA, Furtado AP, Marroni CA. Use of pineapple juice with gadopentetate dimeglumine as a negative oral contrast for magnetic resonance cholangiopancreatography: a multicentric study. Abdom Imaging 2012;37:447-56. [Crossref] [PubMed]
- Kinner S, Steinweg V, Maderwald S, Radtke A, Sotiropoulos G, Forsting M, Schroeder T. Bile duct evaluation of potential living liver donors with Gd-EOB-DTPA enhanced MR cholangiography: Single-dose, double dose or half-dose contrast enhanced imaging. Eur J Radiol 2014;83:763-7. [Crossref] [PubMed]
- Lee Y, Kim SY, Kim KW, Lee SS, Park SH, Byun JH, Lee MG. Contrast-enhanced MR cholangiography with Gd-EOB-DTPA for preoperative biliary mapping: correlation with intraoperative cholangiography. Acta Radiol 2015;56:773-81. [Crossref] [PubMed]
- Neri E, Bali MA, Ba-Ssalamah A, Boraschi P, Brancatelli G, Alves FC, Grazioli L, Helmberger T, Lee JM, Manfredi R, Martì-Bonmatì L, Matos C, Merkle EM, Op De Beeck B, Schima W, Skehan S, Vilgrain V, Zech C, Bartolozzi C. ESGAR consensus statement on liver MR imaging and clinical use of liver-specific contrast agents. Eur Radiol 2016;26:921-31. [Crossref] [PubMed]
- Trunz LM, Guglielmo FF, Selvarajan SK, Naringrekar HV, Alturki A, Dave JK, Mitchell DG. Biliary excretion of gadobenate dimeglumine causing degradation of magnetic resonance cholangiopancreatography (MRCP). Abdom Radiol (NY) 2021;46:562-9. [Crossref] [PubMed]
- Chien CP, Chiu FM, Shen YC, Chen YH, Chung HW. Magnetic resonance cholangiopancreatography at 3T in a single breath-hold: comparative effectiveness between three-dimensional (3D) gradient- and spin-echo and two-dimensional (2D) thick-slab fast spin-echo acquisitions. Quant Imaging Med Surg 2020;10:1265-74. [Crossref] [PubMed]


