
Precise visualization of cricopharyngeal dysfunction after radiation therapy for nasopharyngeal carcinoma using ultrasound-guided balloon catheter dilatation: a case description
Introduction
Swallowing disorder is the most common adverse effect of radiotherapy for nasopharyngeal cancer (NPC). The most common causes of postradiotherapy dysphagia in patients with NPC are fibrosis of the upper esophageal sphincter (UES) caused by the direct destructive effect of radiotherapy and lower cranial nerve dysfunction (1).
The destruction of the UES after radiotherapy for nasopharyngeal carcinoma is irreversible. Nonsurgical treatments are not as effective as are surgical treatments because they are not targeted, while surgical treatments are more invasive than are non-surgical approaches, with risks such as postoperative bleeding, restenosis, and mediastinitis (2). We report for the first time on the application of ultrasound-guided balloon catheter dilation to precisely visualize cricopharyngeal (CP) dysfunction in patients with NPC postradiotherapy.
Case presentation
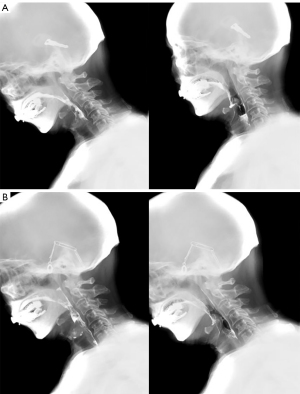
A 72-year-old man was diagnosed with stage I nasopharyngeal cancer (T1N0M0) 13 years ago and underwent radical radiotherapy [gross tumor target volume (GTVnx) 240*30 F/7,200 centigray (cGy), planning gross target volume (PGTVnx) 230*30 F/6,900 cGy, planning target volume 1 (PTV 1) 205*30 F/6,150 cGy, planning target volume 2 (PTV2) 180*28 F/5,400 cGy] for nasopharyngeal malignancy. He developed severe dysphagia 2 years ago. He was subsequently treated for aspiration pneumonia and dysphagia at several hospitals. The dysphagia treatments included oral facial myofunctional training, oropharyngeal sensory training and feeding guidance, and retrograde balloon catheter dilation and traction therapy; however, this produced little progress. Therefore, he could only partially eat small amounts of semiliquid food paste by mouth and required an indwelling feeding tube for eating. When he was referred to our hospital, he relied on tube feeding, showed minimal attempts to consume semifluids, required more than an hour to eat, and produced a large number of moist bubble sounds after swallowing. Flexible endoscopic examination of his swallowing showed swollen mucosa of the root of the tongue, a normal epiglottis, normal bilateral vocal cord activity, and secretions attached to the bilateral piriform recess. Videofluoroscopy (Figure 1) showed severe hypocontractility of the middle and inferior pharyngeal constrictor muscle, inadequate hyolaryngeal excursion, and nonrelaxation of the cricopharyngeal muscle (CPm), placing him at risk of aspiration during swallowing when eating liquid and aspiration after swallowing when eating semifluids with a large amount of residue. After discussion, the patient received ultrasound-guided balloon catheter precise visualization dilatation treatment.
Ethical approval
The research was approved by the Medical Ethics Committee of Zhejiang Provincial People’s Hospital (No. 2017KY024). All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Treatment
The sonographer first performed ultrasonic localization. Grayscale images were obtained on a Resona7S (Mindray Medical International Ltd, Shenzhen, China) ultrasound machine equipped with a linear array transducer with a bandwidth of 5 to 14 MHz. Imaging was performed in the pseudo-color mode using the following image parameters: mode, muscle bone; frequency, 12 MHz; thermal index, 0.2; mechanical index, 1.2; frame rate, 62 frames per second; and dynamic range, 120 dB. The sonographer had 15 years of clinical experience in musculoskeletal ultrasound examinations. After the representative organ was selected on the grayscale images, we marked the picture for location identification and saved images taken as pictures or a video clip for each patient at the following locations: (I) horizontal plane of the vocal cord (Figure 2A), (II) horizontal plane of the sixth cervical vertebra and cricoid cartilage (Figure 2B), (III) horizontal plane of the seventh cervical vertebra and esophagus (Figure 2C), (IV) sagittal plane of the esophagus (Figure 2D), (V) sagittal plane of the esophageal and cricoid cartilage (Figure 2E), and (VI) sagittal plane of the cricopharyngeal muscle (Figure 2F).
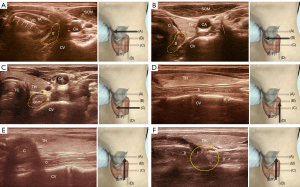
The ultrasound localization procedure comprised the following steps (noting that the probe arrow position on the skin represents the left side of the sonogram in Figure 2A-2F): (I) First, the probe was placed in the transverse section, and the vocal cord was completely displayed (with the vocal cord marked by a small arrow, and the esophagus marked by a yellow dotted segment in Figure 2A); (II) the probe was further inserted into the transverse section of the esophagus (represented by the solid yellow line, with the arrow representing the anterior node of the transverse process of the sixth cervical vertebra in Figure 2B); (III) the probe was advanced until the cricoid cartilage was no longer visible in the cross-section and a clear horizontal surface of the seventh cervical vertebra and the esophagus was visible (outlined by the yellow dashed line in Figure 2C); (IV) the probe was then rotated 90° clockwise to fully display the esophageal sagittal plane (Figure 2D); (V) the probe was panned upward to reveal the cricoid cartilage in the third image (Figure 2E) where hyperechoic calcification can often be seen in older adults, and here, the cricopharyngeal muscle was found at the bottom of the parallel cricoid cartilage wrapped vertically around the esophagus; (VI) in some populations, a slight laterally moving probe could reveal the cricopharyngeal muscle perpendicular to the esophagus (outlined by the yellow line in Figure 2F), and the passage of hypoechoic droplets or food contents through the hypopharynx during normal swallowing could be used to determine the degree of cricopharyngeal muscle opening (see additional Video 1 for details).
The rehabilitation physician began balloon catheter dilation with ultrasound positioning after the ultrasonographer finished positioning the cricopharyngeal muscle in the longitudinal position (Figure 3). The procedure was performed without local anesthesia, and the patient was able to tolerate any associated pain. The steps were as follows: (I) the rehabilitation physician orally inserted a 16-G catheter into the patient’s esophagus. The catheter was seen to pass completely through the cricopharyngeal muscle while being placed under ultrasound guidance (Figure 3A,3B; see additional Video 2 for details); (II) 3–5 mL of ice water was injected into the catheter balloon. When the catheter was lifted, the ultrasound revealed the balloon at the lower edge of the cricopharyngeal muscle, causing a sense of entrapment. The catheter was then lifted upward under ultrasound guidance until the balloon was completely encapsulated by the cricopharyngeal muscle (Figure 3C,3D); (III) 2–4 mL of ice water continued to be injected into the balloon, on top of the initial amount of water contained in the balloon, and the dilatation of water in the balloon was held for 1 minute. Then, the water in the dilated balloon was pumped back until the balloon contained only the initial amount of water, which was held for another minute. Following that, the water was injected and pumped back 5–8 times, depending on the patient’s tolerance level, with a maximum amount of 10 mL water pumped to and from the balloon. The patient kept his head fixed and did not swallow during the procedure; (IV) finally, the balloon was deflated, and the catheter was removed. The frequency of therapy was once a day, 5 days a week. Routine swallowing rehabilitation training was performed after accurate visualization of balloon catheter expansion therapy guided by ultrasound.

After 10 ultrasound-guided balloon catheter treatments, which supported the precise visualization of CP dysfunction, the patient was able to eat a variety of textures and reported that the time spent eating (about 15 minutes each time) was significantly less than that before the treatments. Furthermore, swallowing was easier than before, the sensation of a foreign body in the throat was improved, and pronunciation occurred without a wet bubble sound after swallowing. We assessed the patient before and after treatment (Tables 1,2 and Figure 1). After 10 treatments, swallowing videofluoroscopy demonstrated improved pharyngeal advancement and UES opening and less residue after multiple swallows. The dynamic imaging grade of swallowing toxicity (DIGEST) score indicated that the severity of dysphagia changed from severe to mild. The functional oral intake scale (FOIS) grade and the MD Anderson Dysphagia Inventory (MDADI) score indicated better swallowing function and better quality of life.
Table 1
| Variables | FOIS grade | MDADI score |
|---|---|---|
| Pretreatment | 2 | 24 |
| Posttreatment | 5 | 67 |
FOIS, functional oral intake scale; FOIS grade 2 = reliance on tube feeding, with minimal attempts to consume food or liquids; FOIS grade 5 = complete oral consumption of a variety of textures of food, but requires special preparation or compensation. MDADI, MD Anderson Dysphagia Inventory. The higher the MDADI score, the better the swallowing function and the better the quality of life.
Table 2
| Variables | Maximum PAS Score | Maximum % of pharyngeal residue | DIGEST grade | Cricopharyngeal muscle opening | Hyolaryngeal upward excursion | Hyolaryngeal forward excursion |
|---|---|---|---|---|---|---|
| Pretreatment | 7 | >90% “Near complete residue” | 3 | 1.67 mm | 3.80 mm | 2.48 mm |
| Posttreatment | 2 | 10–49% “Less than half residue” | 1 | 6.48 mm | 5.67 mm | 6.97 mm |
PAS, penetration-aspiration scale; PAS score 7 = material enters the airway, passes below the vocal folds, and is not ejected from the trachea despite effort; PAS score 2 = material enters the airway, remains above the vocal folds, and is ejected from the airway; DIGEST, Dynamic Imaging Grade of Swallowing Toxicity; DIGEST grade 3 = severe; DIGEST grade 1 = mild.
Discussion
Balloon dilation, cricopharyngeal myotomy, and botulinum toxin injection are the most common treatments for postoperative dysphagia after NPC. Myotomy, as an invasive procedure, is typically used when balloon dilation is ineffective after multiple treatments. While myotomy is more effective for CP dysfunction in general, our rationale for not doing so in this case was because of the associated risks. Clary et al. advocated CP dilation as the first step in myotomy (3). Botulinum toxin injections, on the other hand, appear to be effective only in functional muscle tissue and ineffective in fibrotic muscle. As a result, improving the effectiveness of balloon dilatation remains an important research topic.
The dilatation procedure used in previous reports has consisted of blind tube placement with reverse pulling and dilatation (4,5). This has resulted in complications, such as mucosal edema and bleeding, and has failed to achieve effective uniform dilatation of the cricopharyngeal muscle.
One study has reported on the administration of botulinum toxin injection for cricopharyngeal dysfunction, guided by a combination of catheter balloon and ultrasound in patients with stroke (6). However, ultrasound-guided balloon catheter dilation has not been reported in patients with nasopharyngeal carcinoma or stroke.
For the first time, we used ultrasound-guided balloon catheter dilation to provide precise visualization of the cricopharyngeal muscle to treat cricopharyngeal dysfunction after NPC radiotherapy. With ultrasound-guided localization, we were able to target the muscle group more precisely. The precise positioning of continuous, slow, vertical balloon catheter dilation was used to reduce the number of dilation times by extending the dilation time, thus improving the efficiency and reducing the pain of the operation.
Our recommendations for the ultrasound localization procedure are as follows. The normal cricopharyngeal muscle is very thin and not readily visualized with ultrasound. Hence, the point of localization on the transverse section is to show both the cricopharyngeal cartilage and the sixth cervical vertebra (Figure 2B), between which lies the slightly compressed esophagus. The superficial layer of the esophagus is composed of the cricopharyngeal muscle, and, if a probe is moved down to the seventh cervical vertebra, the esophagus can be pushed out of alignment with the cricopharyngeal muscle. In a longitudinal section showing both the long axis of the esophagus and the lower edge of the cricoid cartilage, it can be seen that we can gently move the probe laterally to show the cricopharyngeal muscle circumferentially surrounding the esophagus. When displaying the long-axis view of the esophagus, it is important to make sure that the catheter in the esophagus is also clearly visible on the ultrasound. The balloon portion of the catheter (indicated by the arrow in Figure 3A) should be located, and the catheter should be withdrawn so that it can be positioned in the middle of the lower edge of the cricoid cartilage (where the cricopharyngeal muscle is wrapped). The injection of water into the balloon at this time allows for precise positioning and prevents the uncertainty of blind pulling.
The ultrasound-guided protocols described in this report offer novel approaches for future ultrasound-guided balloon catheter dilation and the localization of botulinum toxin injections in cricopharyngeal dysfunction caused by a variety of etiologies.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-22-63/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The research was approved by the Medical Ethics Committee of Zhejiang Provincial People’s Hospital (No. 2017KY024). All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kong L, Lu JJ, Liss AL, Hu C, Guo X, Wu Y, Zhang Y. Radiation-induced cranial nerve palsy: a cross-sectional study of nasopharyngeal cancer patients after definitive radiotherapy. Int J Radiat Oncol Biol Phys 2011;79:1421-7. [Crossref] [PubMed]
- Kocdor P, Siegel ER, Tulunay-Ugur OE. Cricopharyngeal dysfunction: A systematic review comparing outcomes of dilatation, botulinum toxin injection, and myotomy. Laryngoscope 2016;126:135-41. [Crossref] [PubMed]
- Clary MS, Daniero JJ, Keith SW, Boon MS, Spiegel JR. Efficacy of large-diameter dilatation in cricopharyngeal dysfunction. Laryngoscope 2011;121:2521-5. [Crossref] [PubMed]
- Zhou H, Zhang P, Chen L, Liang P, Liu J, Guan Z. Surface anesthesia and assisted balloon dilatation to treat dysphagia caused by radiotherapy for nasopharyngeal carcinoma. Chin J Phys Med Rehabil 2015;37:921-5.
- Luo Z, Lin G, Chen Z, Yuan L, Xu Y, Jin R. The effect of sEMG biofeedback combined with routine swallow training in treatment of dysphagic patients caused by upper esophageal sphincter stenosis after radiotherapy for nasopharyngeal carcinoma. Chin J Rehabil Med 2020;35:278-82.
- Xie M, Dou Z, Wan G, Zeng P, Wen H. Design and implementation of botulinum toxin on cricopharyngeal dysfunction guided by a combination of catheter balloon, ultrasound, and electromyography (BECURE) in patients with stroke: study protocol for a randomized, double-blinded, placebo-controlled trial. Trials 2021;22:238. [Crossref] [PubMed]


