
Unexpected false-positive uptake of 131I on the right eye in a patient with differentiated thyroid cancer: a case description
Introduction
Differentiated thyroid cancer (DTC), including papillary and follicular thyroid cancer, comprises over 90% of all thyroid cancer cases (1). Iodine-131 (131I) is the most specific radionuclide for DTC imaging, and it plays an important role in depicting metastatic disease after 131I treatment. The accumulation of 131I outside the thyroid bed and areas of physiological uptake is strongly suggestive of a distant functioning metastasis. Therefore, it is essential to distinguish physiologic radioiodine activity from metastatic disease. This report describes a case of false-positive uptake of 131I on the right eye of a patient with DTC. We aimed to contribute to the information available about the false-positive uptake of 131I and improve nuclear medicine physicians’ understanding of this to avoid diagnostic errors which may lead to unnecessary administration of 131I therapeutic doses or surgical procedures.
Case presentation
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was provided by the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
A 58-year-old female patient underwent a total thyroidectomy and neck lymph node dissection due to thyroid nodules in her bilateral thyroid lobes. The histological examination showed a bilobular thyroid with papillary cancer that was 10 mm (right lobe) and 2 mm (left lobe) in diameter. The tumor in the right thyroid lobe was a hobnail cell subtype with infiltration of the thyroid capsule, but the tumor in the left thyroid lobe did not infiltrate the thyroid capsule. The central compartment lymph nodes were not involved (0/13). The BRAF-V600E was wild type.
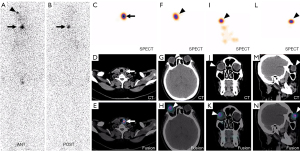
The patient was admitted to the Department of Nuclear Medicine, the Affiliated Hospital of Qingdao University for radioiodine therapy without thyroid hormone for 4 weeks after thyroid surgery. Her serum thyroglobulin (Tg) level was 3.28 ng/mL (reference range, 1.4–78 ng/mL), her serum antithyroglobulin antibody (TgAb) level was 10.15 IU/mL (reference range, 0–115 IU/mL), and her thyroid-stimulating hormone (TSH) level was >100 mIU/L. Her risk stratification when predicting persistent or recurrent disease before 131I treatment was intermediate. Six days after oral administration of 3.7 GBq (100 mCi) of 131I, the post-therapeutic 131I whole-body scan (WBS) showed two foci of 131I (Figure 1A,1B). Single-photon emission computed tomography/computed tomography (SPECT/CT) revealed one lesion in the thyroid bed, which was residual thyroid tissue (Figure 1C-1E). Another lesion was noted in the right eye (Figure 1F-1N).
Further inquiries into the patient’s medical history were unremarkable, and there was no discomfort in her right eye. She refused to undergo an ophthalmic examination. She was followed up on an outpatient basis with determinations of serum Tg and TgAb and neck ultrasonography during TSH-suppressive treatment. At the 5-year follow-up, her inhibitory Tg was less than 0.04 ng/mL, her serum TgAb level was less than 10 IU/mL, and her TSH level was less than 2.0 mIU/L. Follow-up examinations showed no signs of metastatic disease. The outcome showed that she had experienced an excellent response to thyroidectomy and radioiodine therapy.
Discussion
The accumulation of 131I outside the thyroid bed and areas of physiological uptake is strongly suggestive of a distant functioning metastasis. The false-positive uptake of 131I may lead to unnecessary 131I therapy or surgery. The mechanism of false-positive uptake of 131I can be summarized as follows (2): (I) the uptake of 131I is related to the expression of the sodium iodide symporter (NIS) in ectopic thyroid tissue, which can be localized, for example, at the root of the tongue, the thyroglossal duct, or in the subdiaphragmatic organs. (II) The nonthyroidal tissues which can express NIS, such as the salivary gland and the lacrimal gland, can also uptake 131I (3). (III) Retention of 131I in physiological secretions accumulates in dilated ducts or cavities. (IV) Since inflammatory diseases can increase vascularity and capillary permeability, they can also lead to false-positive 131I uptake.
To date, there have been many case reports of false-positive 131I whole-body scans (4-8), but very few reports have detailed the false-positive uptake of 131I in the eyes. As far as we know, eye metastasis from thyroid cancer is rare (9). Bakheet et al. (10) reported the case of a 33-year-old man with an artificial eye who showed 131I uptake, but the uptake completely disappeared after washing of the artificial eye. The mechanism underlying the abnormal collection of radioiodine was also not clear. The authors speculated that it could have been secondary to the accumulation of nasal or lacrimal secretions in the frontal sinuses or lacrimal drainage system or to the nonspecific concentration of iodine in inflamed tissues. Bakheet et al. (10) also reported that some inflammatory conditions, such as dacryocystitis or uveitis, may appear as 131I uptake on scintigraphy. In our case, we were able to rule out this possibility as the patient did not experience any optical symptoms suggestive of inflammation. The CT images did not show swelling or thickening of the lacrimal sac. Since NIS expression is one of the primary mechanisms for false-positive findings on radioiodine scintigrams, reports have indicated that the eye’s ciliary body can have functional NIS expression (11). The patient in our case did not accept any surgery or treatment for her right eye. We speculated that the “hot spot” of 131I on her right eye may have been a false-positive uptake caused by functional NIS expression on her right ciliary body.
In conclusion, our interesting case highlights the potential for false-positive uptake of 131I to be shown on a scan of a normal right eye in a DTC patient. Recognizing false-positive cases is essential to avoid diagnostic errors. The case also illustrated that SPECT/CT could improve imaging specificity for patients after undergoing 131I ablation.
Acknowledgments
We thank the patient and her family for their collaboration.
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-22-247/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was provided by the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, Pacini F, Randolph GW, Sawka AM, Schlumberger M, Schuff KG, Sherman SI, Sosa JA, Steward DL, Tuttle RM, Wartofsky L. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 2016;26:1-133. [Crossref] [PubMed]
- Triggiani V, Moschetta M, Giagulli VA, Licchelli B, Guastamacchia E. Diffuse 131I lung uptake in bronchiectasis: a potential pitfall in the follow-up of differentiated thyroid carcinoma. Thyroid 2012;22:1287-90. [Crossref] [PubMed]
- Glazer DI, Brown RK, Wong KK, Savas H, Gross MD, Avram AM. SPECT/CT evaluation of unusual physiologic radioiodine biodistributions: pearls and pitfalls in image interpretation. Radiographics 2013;33:397-418. [Crossref] [PubMed]
- Shao F, Tang J, Lan X. Variable 131I Activity in Multiple Hepatic Cysts in a Patient With Thyroid Cancer. Clin Nucl Med 2019;44:324-6. [Crossref] [PubMed]
- Shen G, Qi Z, Huang R, Liu B, Kuang A. False-Positive Uptake of Radioiodine in Renal Hamartoma in a Patient With Differentiated Thyroid Cancer. Clin Nucl Med 2017;42:709-10. [Crossref] [PubMed]
- Tong J, Jin Y, Liu M, Lv Z, Chen L. False-Positive Uptake of 131I Due to Tubal Ligation in a Patient With Papillary Thyroid Cancer. Clin Nucl Med 2018;43:375-6. [Crossref] [PubMed]
- Chowdhary AW, Kavanal AJ, Sood A, Prashar S, Upadhyay R, Bhattacharya A, Mittal BR. Posttraumatic Scab on 131I Whole-Body Scan-A False-Positive Finding. Clin Nucl Med 2021;46:512-4. [Crossref] [PubMed]
- Wang A, Fu W, Deng Y, He L, Zhang W. False-Positive 131I Uptake After Transareola Endoscopic Thyroidectomy in a Patient With Papillary Thyroid Carcinoma. Clin Nucl Med 2022;47:324-5. [Crossref] [PubMed]
- Durante C, Haddy N, Baudin E, Leboulleux S, Hartl D, Travagli JP, Caillou B, Ricard M, Lumbroso JD, De Vathaire F, Schlumberger M. Long-term outcome of 444 patients with distant metastases from papillary and follicular thyroid carcinoma: benefits and limits of radioiodine therapy. J Clin Endocrinol Metab 2006;91:2892-9. [Crossref] [PubMed]
- Bakheet SM, Hammami MM. False-positive radioiodine whole-body scan in thyroid cancer patients due to unrelated pathology. Clin Nucl Med 1994;19:325-9. [Crossref] [PubMed]
- Riesco-Eizaguirre G, Santisteban P. A perspective view of sodium iodide symporter research and its clinical implications. Eur J Endocrinol 2006;155:495-512. [Crossref] [PubMed]


