Correlation of normal thyroid ultrasonography with thyroid tests
Introduction
Abnormalities of the thyroid function and its structure are commonly seen and many factors like environmental factors and genetics, age, sex may influence these abnormalities (1). US has been used for a long time in the diagnosis and follow-up of thyroid diseases (2). US is an ideal imaging modality in the evaluation of thyroid gland as an easy to perform, non-expensive, non-invasive method free from ionized radiation. It is not only used in nodular thyroid diseases, but in the detection of autoimmune thyroid diseases (AITD), as well (3,4).
In AITD, decrease in thyroid echogenicity due to lymphocyte infiltration and the disruption of normal tissue structure occurs and the presence of decreased echogenicity in US may assist in the early diagnosis of AITD (2,5-7).
Kim et al., reported that real time US is helpful in the differentiation of diffuse thyroid disease from normal thyroid parenchyma (8).
The relationship between decreased echogenicity or, irregular echo pattern in US with thyroid dysfunction is well known (9). However, data showing correlation of normal US with thyroid tests is limited. In our study, we have excluded nodular thyroid diseases and aimed to compare parenchyma echogenicity of thyroid gland with the laboratory parameters.
Methods
The patients were selected consecutively among the patients who were directed to our hospital for thyroid evaluation regardless of the US examination carried out in other hospitals and who were for the first time subjected to US in our hospital. A total of 681 subjects (552 females, 129 males) were included in the study. Subjects (i) with known thyroid diseases and on related medication, (ii) with thyroid nodules, (iii) undergone thyroid surgery, (iv) received radiotherapy at the head-neck region, (v) undergone radioactive iodine therapy and, (vi) pregnant women were excluded from the study. Subjects were separated into two groups as US normal (group 1) and hypoechoic (group 2) according to US echogenicity. Thyroid stimulating hormone (TSH), free T4 (fT4), thyroid peroxidase antibody (TPOAb), anti-thyroglobulin antibody (TgAb) values of all subjects and thyroid stimulating hormone receptor antibody (TRAb) results of subjects with low TSH were recorded. US examinations were performed with two endocrinologists who have been performing more than 1,000 USs per month (AAT, CK). Intra and inter-observer disagreement was less than 5% in evaluation of the thyroid hypoechogenicity.
Hypoechogenicity was examined within both thyroid lobes. Hypoechogenicity was revealed by comparison of thyroid parenchyma with the echo distribution of surrounding neck muscles. Echogenicity was categorized in three groups: (I) mild (n=119); (II) moderate (n=139); (III) marked (n=120). US was performed with 12-MHz linear probe (Hitachi EUB 7,000 HV). Blood samples following overnight fasting were collected for thyroid tests. TSH: (0.27-4.2 µ IU/mL) (Roche Cobas Elecsys 601), fT4: (0.9-1.7 ng/dL), TgAb (0-40 IU/mL), TPOAb: (0-35 IU/mL) were measured by immunochemiluminescence assay and TRAb (0-14 µ/L) by RIA (Radioimmunoassay) (Zentech Ref. no:R-CT100).
Data obtained from the study was evaluated in SPSS 15.0 statistics package program. Quantitative data were given as average, standard deviation, lowest and highest values, and qualitative values were given as numbers and percentages. Student’s t test was used in the comparison of the means; chi-square test was used in the evaluation of categorical data. Kruskal Wallis test was applied for comparisons of medians among more than two independent groups. Degrees of association between continuous variables were evaluated by Spearman’s Rank Correlation analyses. Categorical data were analyzed by Pearson’s chi-square or Fisher’s exact test, where applicable. Values at the level of P<0.05 were considered to be statistically significant in the analyses. However, all possible multiple comparisons, the Bonferroni Correction was applied for controlling Type I error.
Results
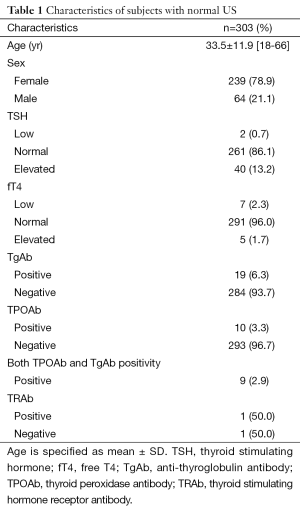
Group 1 involved 303 subjects, 239 (78.9%) females and 64 (21.1%) males; mean age was 33.5±11.9 (range, 18-66) years. In 86.1% (261/303) of group 1 subjects TSH was normal, and fT4 was normal in 96% (291/303). Among 42 TSH altered subjects, 40 (13.2%) had elevated TSH while remaining 2 (0.7%) had low TSH values. Among 12 fT4 altered subjects, 5 (1.7%) had elevated fT4 while remaining 7 (2.3%) had low fT4 values. Nineteen (6.3%) out of 20 subjects with positive thyroid antibodies had TgAb positivity, 10 (3.3%) had TPOAb and 9 (2.9%) had both TgAb and TPOAb positivity. Thyroid antibodies were negative in 93.7% of the group. TRAb was checked in two subjects with low TSH and one of them was found to be positive (Table 1). One subject has overt hyperthyroidism, two subjects had overt hypothyroidism. All thyroid tests were normal in 77.6% of the subjects in group 1.
Full table
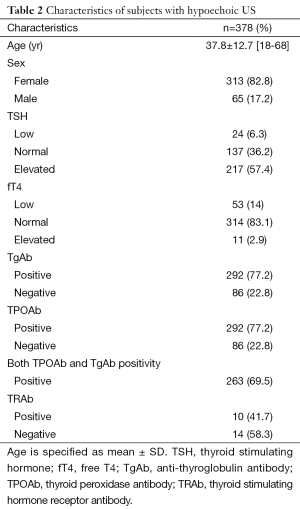
Group 2 involved 378 subjects; 313 (82.8%) females and 65 (17.2%) males; mean age was 37.8±12.7 (range,18-68) years.
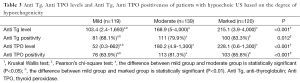
Among group 2 subjects, 63.8% (241/378) showed altered TSH and 16.9% (64/378) showed altered fT4 values. Eleven had elevated fT4 (2.9%) while 53 (14%) had low TSH. 77.2% of the patients had TgAb and 77.2% (292/378) had TPOAb positivity; in 263 (69.5%) subjects both TgAb and were TPOAb positive. TRAb was positive in 10 out of 24 subjects with low TSH who are tested for TRAb. In this group, in 84.9% of the subjects at least one thyroid antibody was positive. 137 had normal TSH (36.2%) while 217 (57.4%) had elevated TSH and 24 (6.3%) had low TSH (Table 2). All thyroid tests were normal in 6.9% of the group 2. Nine subjects have overt hyperthyroidism, 49 subjects had overt hypothyroidism. Individuals were evaluated in three categories depending on their degree of hypoechogenicity as mild, moderate and marked. The more the degree of heterogenecity increased, the more anti-thyroglobulin (Anti Tg) and thyroid peroxidase (Anti TPO) level increased to be statistically significant (respectively r=0.211, r=0.337 and P<0.001) (Table 3). Moreover, while the heterogenecity increased in those with heterogeneous US and hyphothyroidism, TSH levels increased as well (r=0.339 and P<0.001).
Full table
Full table
There was no significant difference based on the Bonferroni correction with regards to median TSH and ST4 levels among the subgroups with Anti Tg negative and Anti Tg positive in group 1 (respectively P=0.992 and P=0.041). There was also no significant difference with regards to TSH and ST4 levels among the subgroups with Anti TPO negative and Anti TPO positive (respectively P=0.940 and P=0.100).
While there was no statistically significant difference based on the Bonferroni correction with regards to median TSH and ST4 levels among the subgroups with Anti Tg negative and Anti Tg positive in group 2 (respectively P=0.368 and P=0.044), the TSH level of the Anti TPO positive group had a higher statistical significance and median ST4 level had a lower statistical significance compared to Anti TPO negative group (respectively P<0.001 and P=0.012).
Among the cases with low level of TSH, median TSH levels were statistically similar between group 1 and group 2 (P=0.812). Among the cases with high level of TSH on the other hand, median TSH level of group 2 had a higher statistical significance compared to group 1 (P<0.001).
There was a significant difference in group 2 compared to group 1 in terms of thyroid antibody-positivity (P<0.001).
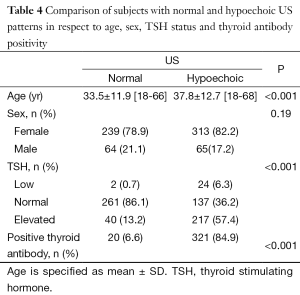
When both groups were compared, while correlation of normal US with normal thyroid tests was 77.6% in group 1 and it was 6.9% in group 2 (P<0.001). In addition, mean age was significantly higher in the group 2 (P<0.001) (Table 4).
Full table
Discussion
US is a valuable tool in the diagnosis of thyroid diseases (2,10). With US, it is possible to detect abnormalities in the thyroid echo structure like thyroid hypoechogenicity (11). Ultrasonographic tissue echogenicity of the thyroid gland depends on the cellularity and vascularization of the organ (12). In a study performed with histologically confirmed, however untreated 53 Hashimoto thyroiditis patients, thyroid hypoechogenicity was reported to be associated with severe follicular degeneration and the disappearance of thyroid follicles (13). Reduced low thyroid echo levels are related to functional disorders like hyperthyroidism or hypothyroidism (12).
When AITD is present with thyroid dysfunction symptoms, it can easily be diagnosed with thyroid hormone levels and with the measurement of thyroid antibodies. In addition, if the symptoms are absent or non-specific and thyroid antibodies are negative, the disease may remain undiagnosed (14). In addition, thyroid antibodies might be present in normal euthyroid individuals (15). In NHANES III study, 11.3% and 10.4% of subjects without known thyroid disease were TPOAb and Anti Tg positive, respectively (16). Hypoechogenicity is an early finding of thyroid autoimmunity and might be seen before the detection of TPOAb (5). In this context, US is quite a convenient tool in the management of these patients.
Nordmeyer et al. reported in their prospective study that autoimmune thyroiditis can be excluded with a ratio of 84% with the use of sonography alone (3).
The relationship between pathological US and thyroid tests is well known, however there are few studies establishing the relationship between normal US and thyroid tests.
Trimboli et al., reported that US had a sensitivity of 90% in the prediction of normal TSH and negative thyroid antibodies and has a sensitivity of 81% in the prediction of normal thyroid tests. In this study, 78.4% of the patients with pathological US had elevated TSH while 76.3% were thyroid antibody positive. 9.5% of the patients with pathological US had normal thyroid tests (17). In another study by the same authors with a smaller sample size, normal US was shown to predict normal TSH and negative thyroid autoantibodies with a sensitivity of 85% and 90%, respectively (18).
Vejbjerg et al. found positive TPOAb in 9.6% and positive TPOAb in 11% of subjects (n=2,851) without thyroid disease and thyroid nodules in US with normal echogenicity. They demonstrated the correlation between reduced echogenicity and elevated TSH values in their studies, despite thyroid hormones in the serum were within the reference range (19).
In their study evaluating the value of US in the prediction of AITD, Pedersen et al., found elevated TSH, low TSH and positive TPOAb in 64.4%, 17.6% and 66.8% of the patients with reduced thyroid echogenicity in US, respectively. They also found positive TPOAb, elevated TSH and low TSH in 10.2%, 2% and 7% of the patients with normal US, respectively (14).
In our study, TSH was normal in 86.1% of the subjects with normal US and thyroid antibodies were negative in 93.4%. All thyroid tests were normal in 77.6% of the subjects. In the heterogeneous US group, all thyroid tests were normal in 6.9% of the individuals. Normal US was significantly correlated with normal thyroid tests. A significant difference was observed between the US homogeneous group and heterogeneous group with regards to thyroid laboratory tests. The combination of normal US with serum TSH will provide substantial information about the thyroid function.
Abnormal thyroid gland pattern on US is not only a diagnostic predictor in the diagnosis of asymptomatic diffuse thyroid disease, but it can also be a good diagnostic predictor in the progression from subclinic to overt hypothyroidism (20,21). Rosário et al. followed-up 117 patients with subclinic hypothyroidism for 3 years. They reported that progression to overt hypothyroidism in patients with positive TPOAb and/or heterogeneous US was higher compared patients with normal US and negative TPOAb (31.2% and 9.5%, respectively), and also TSH normalization ratio was lower (15.6% and 43%, respectively) (22).
Development of hypothyroidism in patients with thyroid autoimmunity is closely related with the extent of thyroid hypoechogenicity. In our study, TSH levels increased with the increase of degree of heterogenecity in the individuals with heterogeneous US and hypothyroidism available. Moreover, while the degree of heterogenecity increased in US, Anti TG and Anti TPO level also significantly increased. Mazziotti et al. reported that hypothyroidism occurred when at least 48.3% of the thyroid parenchyma was hypoechogenic in Hashimoto thyroiditis and hypothyroidism did not develop when at least 38% of the thyroid gland was hyperechogenic. In addition, they detected hypothyroidism in all patients with more than 68% hypoechogenic thyroid parenchyma (10).
In conclusion, our study also indicates that US is beneficial in predicting the normal thyroid tests as well as determining the autoimmune thyroid disease. The sonography of the thyroid gland is a useful, simple and non-invasive modality and provides valuable information about the function of thyroid gland besides evaluating its morphology.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Bülow Pedersen I, Laurberg P, Knudsen N, Jørgensen T, Perrild H, Ovesen L, Rasmussen LB. A population study of the association between thyroid autoantibodies in serum and abnormalities in thyroid function and structure. Clin Endocrinol (Oxf) 2005;62:713-20. [PubMed]
- Rotondi M, Cappelli C, Leporati P, Chytiris S, Zerbini F, Fonte R, Magri F, Castellano M, Chiovato L. A hypoechoic pattern of the thyroid at ultrasound does not indicate autoimmune thyroid diseases in patients with morbid obesity. Eur J Endocrinol 2010;163:105-9. [PubMed]
- Nordmeyer JP, Shafeh TA, Heckmann C. Thyroid sonography in autoimmune thyroiditis. A prospective study on 123 patients. Acta Endocrinol (Copenh) 1990;122:391-5. [PubMed]
- Kim I, Kim EK, Yoon JH, Han KH, Son EJ, Moon HJ, Kwak JY. Diagnostic role of conventional ultrasonography and shearwave elastography in asymptomatic patients with diffuse thyroid disease: initial experience with 57 patients. Yonsei Med J 2014;55:247-53. [PubMed]
- Prummel MF, Wiersinga WM. Thyroid peroxidase autoantibodies in euthyroid subjects. Best Pract Res Clin Endocrinol Metab 2005;19:1-15. [PubMed]
- Raber W, Gessl A, Nowotny P, Vierhapper H. Thyroid ultrasound versus antithyroid peroxidase antibody determination: a cohort study of four hundred fifty-one subjects. Thyroid 2002;12:725-31. [PubMed]
- Döbert N, Balzer K, Diener J, Wegscheider K, Vaupel R, Grünwald F. Thyroid sonomorphology, thyroid peroxidase antibodies and thyroid function: new epidemiological data in unselected German employees. Nuklearmedizin 2008;47:194-9. [PubMed]
- Kim DW, Eun CK, In HS, Kim MH, Jung SJ, Bae SK. Sonographic differentiation of asymptomatic diffuse thyroid disease from normal thyroid: a prospective study. AJNR Am J Neuroradiol 2010;31:1956-60. [PubMed]
- Shin DY, Kim EK, Lee EJ. Role of ultrasonography in outcome prediction in subclinical hypothyroid patients treated with levothyroxine. Endocr J 2010;57:15-22. [PubMed]
- Mazziotti G, Sorvillo F, Iorio S, Carbone A, Romeo A, Piscopo M, Capuano S, Capuano E, Amato G, Carella C. Grey-scale analysis allows a quantitative evaluation of thyroid echogenicity in the patients with Hashimoto's thyroiditis. Clin Endocrinol (Oxf) 2003;59:223-9. [PubMed]
- Rago T, Chiovato L, Grasso L, Pinchera A, Vitti P. Thyroid ultrasonography as a tool for detecting thyroid autoimmune diseases and predicting thyroid dsfunction in apparently healthy subjects. J Endocrinol Invest 2001;24:763-9. [PubMed]
- Schiemann U, Gellner R, Riemann B, Schierbaum G, Menzel J, Domschke W, Hengst K. Standardized grey scale ultrasonography in Graves' disease: correlation to autoimmune activity. Eur J Endocrinol 1999;141:332-6. [PubMed]
- Hayashi N, Tamaki N, Konishi J, Yonekura Y, Senda M, Kasagi K, Yamamoto K, Iida Y, Misaki T, Endo K, et al. Sonography of Hashimoto's thyroiditis. J Clin Ultrasound 1986;14:123-6. [PubMed]
- Pedersen OM, Aardal NP, Larssen TB, Varhaug JE, Myking O, Vik-Mo H. The value of ultrasonography in predicting autoimmune thyroid disease. Thyroid 2000;10:251-9. [PubMed]
- Feldt-Rasmussen U. Analytical and clinical performance goals for testing autoantibodies to thyroperoxidase, thyroglobulin, and thyrotropin receptor. Clin Chem 1996;42:160-3. [PubMed]
- Hollowell JG, Staehling NW, Flanders WD, Hannon WH, Gunter EW, Spencer CA, Braverman LE. Serum TSH, T(4), and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). J Clin Endocrinol Metab 2002;87:489-99. [PubMed]
- Trimboli P, Rossi F, Thorel F, Condorelli E, Laurenti O, Ventura C, Nigri G, Romanelli F, Guarino M, Valabrega S. One in five subjects with normal thyroid ultrasonography has altered thyroid tests. Endocr J 2012;59:137-43. [PubMed]
- Trimboli P, Rossi F, Condorelli E, Laurenti O, Ventura C, Nigri G, Romanelli F, Guarino M, Valabrega S. Does normal thyroid gland by ultrasonography match with normal serum thyroid hormones and negative thyroid antibodies? Exp Clin Endocrinol Diabetes 2010;118:630-2. [PubMed]
- Vejbjerg P, Knudsen N, Perrild H, Laurberg P, Pedersen IB, Rasmussen LB, Ovesen L, Jørgensen T. The association between hypoechogenicity or irregular echo pattern at thyroid ultrasonography and thyroid function in the general population. Eur J Endocrinol 2006;155:547-52. [PubMed]
- Park M, Park SH, Kim EK, Yoon JH, Moon HJ, Lee HS, Kwak JY. Heterogeneous echogenicity of the underlying thyroid parenchyma: how does this affect the analysis of a thyroid nodule? BMC Cancer 2013;13:550. [PubMed]
- Díez JJ, Iglesias P. Spontaneous subclinical hypothyroidism in patients older than 55 years: an analysis of natural course and risk factors for the development of overt thyroid failure. J Clin Endocrinol Metab 2004;89:4890-7. [PubMed]
- Rosário PW, Bessa B, Valadão MM, Purisch S. Natural history of mild subclinical hypothyroidism: prognostic value of ultrasound. Thyroid 2009;19:9-12. [PubMed]


