
Can contrast-enhanced ultrasound with perfluorobutane add value in detection of hepatocellular carcinoma in cirrhosis during surveillance?
Ultrasound (US) plays a pivotal role in the recognition of hepatocellular carcinoma (HCC) in cirrhosis (1). HCC represents the sixth most common malignancy and the fourth most frequent cause of cancer-related death in the world (2). Since the early 1980s, the US has described the fundamental findings of the HCC nodules appearing in a cirrhotic liver and significantly contributed to the knowledge of the natural history of this malignancy (3). Subsequently, conventional US has been the unique tool recognized for surveillance of the appearance of HCC nodules in cirrhosis (4). Today, all scientific Societies for the study of liver disease endorsed bi-annual US as a sensitive tool for surveillance (5-10). At the end of 1990s, availability of new US contrast agents represented a true revolution in the field of diagnostic US [also see its treatment application (11)]. Contrast-enhanced ultrasound (CEUS) can be considered a real revolution in the setting of dynamic imaging modalities for liver malignancies (12,13). Like contrast-enhanced computed tomography (CECT) and contrast-enhanced magnetic resonance imaging (CEMRI), CEUS is a dynamic technique able to show rapidly, non-invasively and—most importantly—in real-time the hepatic vasculature. CEUS allows the study of the different phases (arterial, portal and late phase) of blood supply of focal liver lesions and especially of HCC lesions that can be easily characterized (12-14). There are two main US contrast agents on the market: the sulphur-hexafluoride (SonoVue, Bracco Imaging Italia, Milan, Italy) and perfluorobutane (Sonazoid, Daiichi-Sankyo, Tokyo, Japan; GE Healthcare, Milwaukee, WI, USA) (12-15). SonoVue is a pure bloodstream agent; it is widely distributed in Western and Asian countries and has also recently been approved by FDA in USA (16). Sonazoid is available in Japan, South Korea, Denmark, Norway and was recently approved in China (17). Unlike SonoVue, gas-containing microbubbles of Sonazoid has the advantage to allow very stable Kupffer phase imaging for at least 60 minutes in addition to vascular phase imaging (17-19). Sonazoid is phagocytized by the Kupffer cells, which are liver-specific macrophages, amplifying US scattering to generate amplified sound waves (18,19). Thus HCC nodules that have markedly fewer or absent Kupffer cells show a signal defect on US images obtained during the Kupffer phase, appearing hypovascular in this phase (19).
CEUS offers a great advantage in clinical practice: during surveillance of HCC, if a new nodule is detected on conventional US, physicians can immediately perform CEUS of the new nodule and characterize this nodule if it is a HCC, so to shorten the diagnostic and therapeutic work up (20,21). Unfortunately, by using SonoVue, this approach does not allow the detection of further HCC nodules: due to the short duration of the arterial phase (10–30 seconds), only one nodule can be studied at a time (19). Instead, the use of Sonazoid that allows a long-term study (up to 60 minutes) either of the vascular and Kupffer phases, allows such possibility (18). Since the HCC nodules do not contain Kupffer cells, they appear hypovascular in this phase and therefore new nodules can be detected over time (18). Therefore, the possibility of adding CEUS using Sonazoid immediately after conventional US in order to increase detection of new nodules during surveillance could be highly desirable in clinical practice.
The study of Park and colleagues recently appeared on Radiology addresses this issue (15). On the basis of above-mentioned characteristics of Sonazoid, these authors “hypothesized that the detection rate of early-stage HCC (BCLC stage 0 or A) could be improved with fewer false referrals by adding perfluorobutane enhanced US to conventional US” (15). Park and coworkers carried out a prospective multi-center diagnostic trial on 524 consecutive participants enrolled from October 2014 to August 2016 at five tertiary referral Hospitals in Korea. All participants had cirrhosis and underwent conventional US for surveillance. Participants had a mean age of 54 years and were predominantly male. The cirrhosis was mainly hepatitis B virus-related (HBV-related) (94.1% of cases) and most of the participants were or had been treated with antiviral treatment (69.7%). Fifty-seven percent of 56.7% of participants had child A cirrhosis and most of them had an albumin-bilirubin score grade 1. The mean body mass index was 24.1. Diagnosis of HCC was made either with pathologic analysis and CECT and/or CEMRI using gadoxetic acid as contrast medium. The primary end points of the study were the detection rate of early-stage HCC according to the Barcelona clinic liver cancer (BCLC) staging system and false referral rate.
After the conventional US, all participants immediately underwent CEUS using Sonazoid. When a suspected HCC was observed, a Kupffer phase US was subsequently performed for the focal lesion and for the remaining liver parenchyma. When no suspected HCC was detected with conventional US, a Kupffer phase US was immediately performed for the evaluation of the entire liver. If an additional focal lesion was detected during the Kupffer phase, vascular phase US was once again performed for the additional lesion via re-administration of Sonazoid. In case there was no nodule suspected for HCC on either conventional US or Kupffer phase, the examination was completed without vascular phase. Results of the trial showed that there was no improvement in the detection rate of early-stage HCC by adding CEUS with Sonazoid to conventional US. In fact, the detection rate of early-stage HCC with conventional US was 0.8% [4/524; accuracy =95.2%; 95% confidence interval (95% CI), 93.0–96.9%] and it was 1.1% (6/524; accuracy =95.6%; 95% CI, 93.5–97.2%) when CEUS with Sonazoid was added. The false referral rate was significantly reduced by 3% (4/524 vs. 6/524). Table 1 reports the diagnostic test evaluation according to the original data of Park and coworkers.
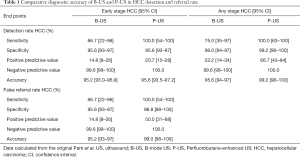
Full table
The results of Park et al. inspired some criticism. Firstly, as said above, 94% of their participants have HBV related cirrhosis, therefore such results can only be applicable in a particular geographic area. Secondly, and not surprisingly, the number of new detected HCC was too low: 8 out of 524 (1.5%) participants were diagnosed with HCC at any stage and only 6 out of 524 (1.1%) at early stage HCC. Authors themselves state that this was due to the antiviral treatment of most of the participants to the study. Maybe if they had found a higher number of nodules, the results could have been positive since they would have had the possibility to add the Sonazoid-CEUS to conventional US. Finally, we would have expected that, during a surveillance program, new detected nodules would be much less than 3 cm and not >3 cm (even up to 6.8 cm) as it happened in a relevant rate of cases in the study of Park and colleagues. This should be due to the fact that very small nodules were not seen at a very early stage or this was the consequence of the direct oncogenetic effect of HBV (22).
The study conducted by Park and colleagues (15), although reporting a negative result, has the merit of being the first to investigate whether adding Sonazoid to conventional US could be useful in the detection of new lesions in a cirrhotic liver during surveillance. There are two considerations that can be made on these results. On the one hand, the negative result for the Sonazoid, with all limits reported above, reduces the high hopes on adding CEUS to conventional US and the prospects of this tool to improve detection and even staging of the HCC, at least in the liver. Therefore, at least according to results of Park et al., CEUS, either using sulfur hexafluoride or perfluorobutane, remains a useful tool only for the characterization of HCC in cirrhosis. On the other hand, the sensitivity of conventional US (resulted in this study being 75.0% with an accuracy of 95.6%) is not questioned and it can continue to be used without fear of low sensitivity as is the case of liver metastases where the add of CEUS to conventional US dramatically improves the detection of further lesions, increasing CEUS sensitivity up to 40% (23).
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Soresi M, Terranova A, Licata A, Serruto A, Montalto G, Brancatelli G, Giannitrapani L. Surveillance program for diagnosis of HCC in liver cirrhosis: role of ultrasound echo patterns. Biomed Res Int 2017;2017:4932759. [Crossref] [PubMed]
- Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018;68:394-424. [Crossref] [PubMed]
- Maringhini A, Cottone M, Sciarrino E, Marcenò MP, La Seta F, Rinaldi F, Pagliaro L. Ultrasonographic and radionuclide detection of hepatocellular carcinoma in cirrhotics with low alpha-fetoprotein levels. Cancer 1984;54:2924-6. [Crossref] [PubMed]
- Harris PS, Hansen RM, Gray ME, Massoud OI, McGuire BM, Shoreibah MG. Hepatocellular carcinoma surveillance: an evidence-based approach. World J Gastroenterol 2019;25:1550-9. [Crossref] [PubMed]
- Omata M, Cheng AL, Kokudo N, Kudo M, Lee JM, Jia J, Tateishi R, Han KH, Chawla YK, Shiina S, Jafri W, Payawal DA, Ohki T, Ogasawara S, Chen PJ, Lesmana CRA, Lesmana LA, Gani RA, Obi S, Dokmeci AK, Sarin SK. Asia-Pacific clinical practice guidelines on the management of hepatocellular carcinoma: a 2017 update. Hepatol Int 2017;11:317-70. [Crossref] [PubMed]
- Korean Liver Cancer Study Group (KLCSG), National Cancer Center, Korea (NCC). 2014 KLCSG-NCC Korea practice guideline for the management of hepatocellular carcinoma. Gut Liver 2015;9:267-317. [PubMed]
- Heimbach JK, Kulik LM, Finn RS, Sirlin CB, Abecassis MM, Roberts LR, Zhu AX, Murad MH, Marrero JA. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology 2018;67:358-80. [Crossref] [PubMed]
- European Association for the Study of the Liver. EASL clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol 2018;69:182-236. [Crossref] [PubMed]
- Raccomandazioni multisocietarie Italiane (AISF, AIOM, IT IHPBA, SIC, SIRM, SITO) per la gestione clinica integrata del paziente con epatocarcinoma (HCC). 2016. Available online: https://www.sirm.org/wp-content/uploads/2019/03/HCC.pdf. [Last accessed on 24 May 2019].
- Claudon M, Dietrich CF, Choi BI, Cosgrove DO, Kudo M, Nolsøe CP, Piscaglia F, Wilson SR, Barr RG, Chammas MC, Chaubal NG, Chen MH, Clevert DA, Correas JM, Ding H, Forsberg F, Fowlkes JB, Gibson RN, Goldberg BB, Lassau N, Leen EL, Mattrey RF, Moriyasu F, Solbiati L, Weskott HP, Xu HX. World Federation for Ultrasound in Medicine. European Federation of Societies for Ultrasound. Guidelines and good clinical practice recommendations for contrast enhanced ultrasound (CEUS) in the liver-update 2012: a WFUMB-EFSUMB initiative in cooperation with representatives of AFSUMB, AIUM, ASUM, FLAUS and ICUS. Ultrasound Med Biol 2013;39:187-210. [Crossref] [PubMed]
- Ma QP, Xu EJ, Zeng QJ, Su ZZ, Tan L, Chen JX, Zheng RQ, Li K. Intraprocedural computed tomography/magnetic resonance-contrast-enhanced ultrasound fusion imaging improved thermal ablation effect of hepatocellular carcinoma: Comparison with conventional ultrasound. Hepatol Res 2019;49:799-809. [PubMed]
- Quaia E, Calliada F, Bertolotto M, Rossi S, Garioni L, Rosa L, Pozzi-Mucelli R. Characterization of focal liver lesions with contrast-specific US modes and a sulfur hexafluoride-filled microbubble contrast agent: diagnostic performance and confidence. Radiology 2004;232:420-30. [Crossref] [PubMed]
- Salvatore V, Gianstefani A, Negrini G, Allegretti G, Galassi M, Piscaglia F. Imaging diagnosis of hepatocellular carcinoma: recent advances of contrast-enhanced ultrasonography with SonoVue®. Liver Cancer 2016;5:55-66. [Crossref] [PubMed]
- Giorgio A, Ferraioli G, Tarantino L, de Stefano G, Scala V, Scarano F, Coppola C, Del Viscovo L. Contrast-enhanced sonographic appearance of hepatocellular carcinoma in patients with cirrhosis: comparison with contrast-enhanced helical CT appearance. AJR Am J Roentgenol 2004;183:1319-26. [Crossref] [PubMed]
- Park JH, Park MS, Lee SJ, Jeong WK, Lee JY, Park MJ, Lee SS, Han K, Nam CM, Park SH, Lee KH. Contrast-enhanced us with perfluorobutane for hepatocellular carcinoma surveillance: a multicenter diagnostic trial (SCAN). Radiology 2019;292:638-46. [Crossref] [PubMed]
- Seitz K, Strobel D. A milestone: approval of CEUS for diagnostic liver imaging in adults and children in the USA. Ultraschall Med 2016;37:229-32. [Crossref] [PubMed]
- Nolsøe CP, Lorentzen T. International guidelines for contrast-enhanced ultrasonography: ultrasound imaging in the new millennium. Ultrasonography 2016;35:89-103. [Crossref] [PubMed]
- Yanagisawa K, Moriyasu F, Miyahara T, Yuki M, Iijima H. Phagocytosis of ultrasound contrast agent microbubbles by Kupffer cells. Ultrasound Med Biol 2007;33:318-25. [Crossref] [PubMed]
- Goto E, Masuzaki R, Tateishi R, Kondo Y, Imamura J, Goto T, Ikeda H, Akahane M, Shiina S, Omata M, Yoshida H, Koike K. Value of post-vascular phase (Kupffer imaging) by contrast-enhanced ultrasonography using Sonazoid in the detection of hepatocellular carcinoma. J Gastroenterol 2012;47:477-85. [Crossref] [PubMed]
- Giorgio A, Gatti P, Matteucci P, Giorgio V. Contrast-enhanced ultrasound with sulphur-hexafluoride in diagnosis of early HCC in cirrhosis. Hepatoma Res 2019;5:20.
- Giorgio A, Montesarchio L, Gatti P, Amendola F, Matteucci P, Santoro B, Merola MG, Merola F, Coppola C, Giorgio V. Contrast-enhanced ultrasound: a simple and effective tool in defining a rapid diagnostic work-up for small nodules detected in cirrhotic patients during surveillance. J Gastrointestin Liver Dis 2016;25:205-11. [PubMed]
- Torresi J, Tran BM, Christiansen D, Earnest-Silveira L, Schwab RHM, Vincan E. HBV-related hepatocarcinogenesis: the role of signalling pathways and innovative ex vivo research models. BMC Cancer 2019;19:707. [Crossref] [PubMed]
- Ferraioli G, Meloni MF. Contrast-enhanced ultrasonography of the liver using SonoVue. Ultrasonography 2018;37:25-35. [Crossref] [PubMed]


