Transcatheter embolization of a large aberrant systemic artery to an intralobar pulmonary sequestration using an Amplatzer vascular plug in an adolescent
Introduction
Pulmonary sequestration is a rare congenital malformation. It consists in the existence of an aberrant systemic artery, responsible for the blood supply of a lung area, instead of its functional pulmonary feeding (1). The sequestrated parenchyma in not functional and may lead to different complications, such as infections, dyspnea, chest pain or bleeding. A treatment is necessary to reduce this risk. The aim of this case report is to show the possibility of endovascular embolization procedure with Amplatzer vascular plug (AVP) for the treatment of this condition.
Case presentation
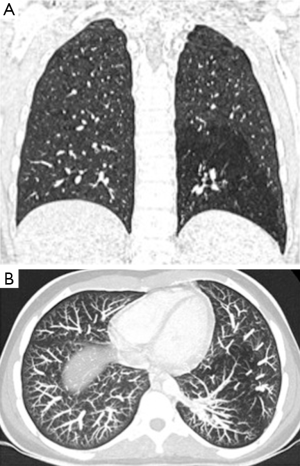
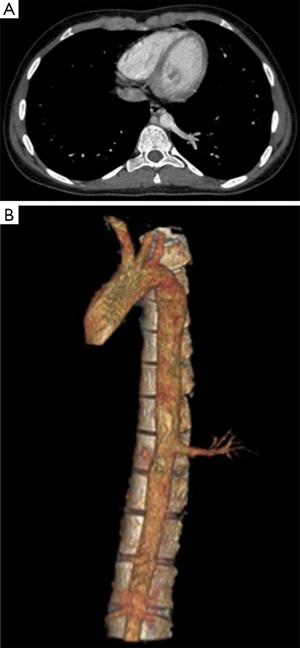
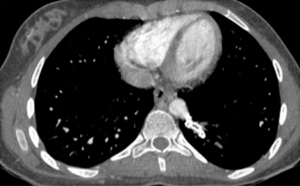
A 14-year-old girl was referred to our radiology department to perform thoracic contrast-enhanced multidetector computed tomography (MDCT) after the occurrence of unexplained basal left chest pain. She had no other medical history and her clinical exam was normal. She did not report any episode of lung infection or hemoptysis. MDCT showed in her left lower pulmonary lobe a large hypointense area of consolidation, contrasting with the rest of the parenchyma (Figure 1). It also highlighted an abnormal systemic artery arising from the thoraco-abdominal aorta and supplying the area of consolidated lung with the venous drainage via the inferior pulmonary vein (Figure 2). The diagnosis of intralobar pulmonary sequestration was done. No other feature was seen on the exam, especially no condensation and no cyst. After discussion between the pediatric surgeon and the interventional radiologist, an endovascular treatment was decided. The patient underwent digital subtraction angiography (DSA) after a femoral catheterization of the aorta. It confirmed the existence of a large aberrant artery arising from the left side of the thoraco-abdominal aorta (Figure 3).
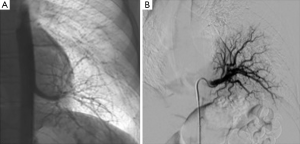
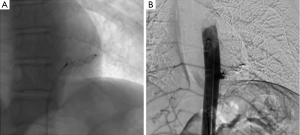
Selective occlusion of this feeding artery was performed by placing two AVPs IV and II of 8 and 10 mm (30% of oversize) (St. Jude Medical, Zaventem, Belgium), respectively, at the trunk and the proximal portion of the artery. A few minutes after their deployment, complete vessel occlusion was obtained (Figure 4). Post-operative CT scan was performed to confirm the absence of residual blood supply in the sequestration or any complication (Figure 5). There was no pulmonary necrosis. The patient was discharge 24 h after intervention. Follow-up CT scan at 3 months showed no recurrence and the patient was asymptomatic.
Discussion
Despite it is a rare condition, pulmonary sequestration is the most frequent lung congenital malformation. It is separated into two categories. Intralobar sequestration (about 75%) is located into the normal lung, with a pulmonary venous drainage. Extralobar sequestration (about 25%) is separated from normal lung by its own pleura, with a systemic venous drainage in the azygos or inferior vena cava (1). The systemic artery may come from the thoracic aorta or from the abdomen, especially from the celiac trunk. Usually, the communication with the bronchial tree is absent or abnormal but it might be normal in some intralobar sequestration cases (2). Patients frequently suffer from recurrent bronchopulmonary infections. Sometimes, sequestration is responsible for hemoptysis and rarely hemothorax, due to high-pressure systemic blood supply in inflammatory lung tissue (3). Some patients are asymptomatic, explaining that sequestration may be discovered in adulthood. Many radiological features may reveal the sequestration on chest X-ray or CT scan. The most frequent lesion is a mass or parenchyma consolidation, especially in the lower lobes. Sometimes, the sequestration is represented by a hypointense area, due to trapping phenomenon. We can also see cysts, bronchiectasia or pleural effusion. Finally, the most important feature is the existence of an abnormal systemic artery (4). To avoid complications, surgery was the commonly admitted treatment, with removal of the segment or lobe containing the sequestration. In the last few years, less invasive endovascular procedures have represented an alternative treatment. It consists in the occlusion of abnormal artery with endovascular devices, to decrease the risk of bleeding and induce an involution of the sequestrated parenchyma (4-6). Metallic coils represent the preferred embolization material in most of the previously reported cases (6). The AVP family (divided into four types of devices) is particularly suited for embolization of large, short and high-flow vessels where coil migration is possible or multiple coils may be needed (7,8). AVPs seemed to us the optimal tool in order to achieve a complete proximal occlusion of the vessel minimizing the risk of regurgitation and distant embolization. Endovascular treatment is sometimes performed before surgery to reduce the bleeding operative risk (5). Finally, interventional radiology offers a possibility of fast treatment in emergency in cases of massive symptomatic hemoptysis (3). Endovascular treatment represents a less invasive alternative option to surgery for the management of pulmonary sequestration. The present report is the first on the use of AVP in adolescents for this condition. Our patient is totally asymptomatic since embolization was performed three months previously. Nonetheless, the sequestered area was just moderately reduced in size. A longer follow-up is needed to answer the question if regression may occur and, above all, if this has clinical significance. In conclusion, pulmonary sequestration in adolescents may be successfully managed by means of percutaneous endovascular treatment, resulting in satisfactory mid-term clinical results. AVPs should be used, in our opinion, in order to minimize complications. The endovascular procedure can be used as first choice or in patients who are not suitable for surgery and/or refuse the operation. Finally, wider experience and lasting follow-up are needed to propose the embolization as an alternative to surgery in the treatment of pulmonary sequestration in adolescents.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this Letter to the Editor and any accompanying images.
References
- Ragusa M, Vannucci J, Lenti M, Cieri E, Cao P, Puma F. Pulmonary sequestration supplied by giant aneurysmal aortic branch. Ann Thorac Surg 2010;89:e7-8. [Crossref] [PubMed]
- Avsenik J, Štupnik T, Popovič P. Endovascular embolization prior to surgical resection of symptomatic intralobar pulmonary sequestration in an adult. Eur J Radiol Open 2015;3:12-5. [Crossref] [PubMed]
- Kim TE, Kwon JH, Kim JS. Transcatheter embolization for massive hemoptysis from an intralobar pulmonary sequestration: a case report. Clin Imaging 2014;38:326-9. [Crossref] [PubMed]
- Ahn SJ, Kim EY, Kim JH, Byun SS, Kim HS, Choi HY, Sun YH. Successful endovascular treatment of bilateral intralobar pulmonary sequestration with a bridging isthmus in a child. Pediatr Pulmonol 2014;49:E126-9. [Crossref] [PubMed]
- Saxena P, Marshall M, Ng L, Sinha A, Edwards M. Preoperative embolization of aberrant systemic artery in sequestration of lung. Asian Cardiovasc Thorac Ann 2011;19:357-9. [Crossref] [PubMed]
- Ganeshan A, Freedman J, Hoey ET, Steyn R, Henderson J, Crowe PM. Transcatheter coil embolisation: a novel definitive treatment option for intralobar pulmonary sequestration. Heart Lung Circ 2010;19:561-5. [Crossref] [PubMed]
- Leoncini G, Rossi UG, Ferro C, Chessa L. Endovascular treatment of pulmonary sequestration in adults using Amplatzer® vascular plugs. Interact Cardiovasc Thorac Surg 2011;12:98-100. [Crossref] [PubMed]
- Hwang HK, Tsai YS, Lin SM, Chen MR. Occlusion of an aberrant artery to an intralobar pulmonary sequestration using an Amplatzer Vascular Plug. Pediatr Pulmonol 2008;43:933-5. [Crossref] [PubMed]


