
Ultrasound-guided sacral plexus and sacral nerve root blocks alleviating neuropathic pain caused by sacral plexus injury: a case presentation
Introduction
Neuropathic pain has been defined as “pain caused by a lesion or disease of the somatosensory nervous system” by the international association for the study of pain (1). For fall injuries associated with sacral fractures, injury mechanisms include sacral or pelvic fractures and nerve lacerations. Since neuropathic pain is correlated with complex mechanisms, various drugs have been used to treat neuropathic pain, such as anticonvulsants, antidepressants, opioids, and so on (2). However, the effectiveness of the drugs may be limited for chronic intractable neuropathic pain, especially when they cannot be used at an adequate dose, due to undesirable side effects and the underlying disease. Currently, the optimal treatment of sacral fracture and sacral nerve injury remains controversial, with unsatisfactory results.
Ultrasound has been used for regional blockades for decades. For peripheral nerve blocks, ultrasound guidance allows visualization of target nerves, the advancement of the needle (in-plane technique), and the spread of the local anesthetic (3). Here, we present a case of successful treatment with ultrasound-guided nerve block using glucocorticoid for intractable neuropathic pain. We hope that this treatment technique may provide an excellent and conservative treatment strategy for patients with traumatic and neuropathic pain.
Case presentation
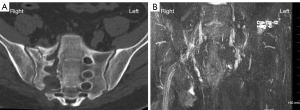
A 27-year-old patient had undergone pelvic internal fixation surgery 3 months ago due to a fall from height. Since then, there had been no improvement in his right lower limb numbness and foot drop. The pain manifested as a persistent painful paresthesia and neuralgia throughout the right leg from hip to toe (S1–3), with progressive aggravation. After 3 months, the patient was admitted to the hospital and received a diagnosis of neuropathic pain, sacral plexus injury, and postoperative pelvic and sacral fracture (Denis type II). He reported a very sharp, needle- and electric shock-like pain on the whole right leg that was continuously merged (from hip to all toes, S1–3 region), accompanied by obvious symptoms of hyperalgesia, tactile allodynia, and paresthesia. The numeric rating scale (NRS) of the patient was 9/10. Computed tomography (CT) plain scan showed changes after internal fixation of the fractures of the lumbar and the right side of the sacrum. There were no bone fragments in the sacral foramen or vertebral canal, and the sacrum was relatively aligned (Figure 1A). Contrast magnetic resonance imaging (MRI) scanning revealed thickening of the S1–3 nerve root at the junction of the sciatic nerve and peripheral effusion, which was considered indicative of sacral plexus injury (Figure 1B). Electromyography (EMG) indicated that the injury had occurred in the right S1–3 sacral nerve. Therefore, nerve adhesion, edema, and aseptic inflammation were considered the causes of this patient’s neurological symptoms. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this article and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
This severe pain did not improve significantly with medication (NRS 8/10). Thus, after obtaining the patient’s consent, we performed an ultrasound-guided sacral plexus and S1–3 nerve root blocks using local anesthetics.
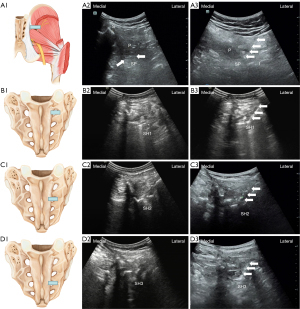
First, the sacral plexus block was performed. A low-frequency convex array transducer was placed along the transverse plane after the patient had been disinfected and stabilized in a prone position. The anatomy is shown in Figure 2, A1. The 2-dimensional (2D) cross-sectional ultrasound imaging is shown in Figure 2, A2. The entry point was located at the lower margin of the medial half of a line between the posterior superior iliac crest and the greater trochanter of the femur. The needle (22 G, 12 cm) was inserted along the plane between the sacrum and the ilium for sciatic plexus block using 12 mL of 0.375% ropivacaine. The needle insertion path is shown in Figure 2, A3. We then performed blocks of S–S3 through the foramina sacral posterior. The anatomy is shown in Figure 2, B1, and the 2D cross-sectional ultrasound imaging is shown in Figure 2, B2. Adopting the method of inserting the needle along the plane, the needle was inserted into the posterior foramina sacral for the S1 nerve block using 3 mL of 0.375% ropivacaine, and the needle insertion path is shown in Figure 2, B3. In the same way, we performed blocks of S2 (Figure 2, C1-2C3) and S3 (Figure 2, D1-2D3). The NRS reduced from 8 to 5 for a short time. Next, we used ultrasound guidance and performed S1–3 nerve and sacral plexus block with a mixture of 0.375% ropivacaine and triamcinolone. After injection, the patient’s pain was significantly relieved and the NRS score was reduced to 3 points. The above treatment was administered once a week for a total of 4 times. The sharp pain and discharge-like tingling sensation in the foot of the patient were alleviated after receiving 4 treatments (NRS 2-3/10). The pain was significantly relieved after 3 months (NRS 1-2/10). A year later, the patient’s pain was completely relieved.
Discussion
Ultrasound-guided techniques to accurately assess the target region are superior to blind techniques (4). As a real-time imaging technology, ultrasound technology can effectively reflect the thickness, depth, accurate location, and adjacent structures of the patient’s nerves (5,6). So far, few researchers have studied the effect of sacral plexus and sacral nerve root blocks on pain. In the current study, the application of ultrasonic guidance for sacral plexus and sacral nerve root blocks were shown to alleviate pain effectively on an intractable patient with sacral plexus injury related to sacrum fracture. Glucocorticoid injections that relieve inflammatory reactions are generally applied in clinical practice for treating aseptic inflammation and neuropathic pain by reducing nerve inflammation and ischemia due to multiple conditions, including inflammatory edema, adhesive tissues, and scar formation (7,8). This study demonstrates that sacral plexus and sacral nerve root blocks with ultrasonic guidance could alleviate the incidence and degree of allodynia and hyperalgesia and greatly improve patient satisfaction.
Acknowledgments
Funding: This work was funded by
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-23-1560/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this article and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Wang D, Lu Y, Han Y, Zhang X, Dong S, Zhang H, Wang G, Wang G, Wang JJ. The Influence of Etiology and Stimulation Target on the Outcome of Deep Brain Stimulation for Chronic Neuropathic Pain: A Systematic Review and Meta-Analysis. Neuromodulation 2024;27:83-94. [Crossref] [PubMed]
- Mu A, Weinberg E, Moulin DE, Clarke H. Pharmacologic management of chronic neuropathic pain: Review of the Canadian Pain Society consensus statement. Can Fam Physician 2017;63:844-52.
- Gadsden JC. The role of peripheral nerve stimulation in the era of ultrasound-guided regional anaesthesia. Anaesthesia 2021;76:65-73. [Crossref] [PubMed]
- Bosenberg AT. Innovative peripheral nerve blocks facilitated by ultrasound guidance. Paediatr Anaesth 2018;28:684-5. [Crossref] [PubMed]
- Guay J, Suresh S, Kopp S. The use of ultrasound guidance for perioperative neuraxial and peripheral nerve blocks in children. Cochrane Database Syst Rev 2019;2:CD011436. [Crossref] [PubMed]
- Gungor I, Gunaydin B, Oktar SO. M Buyukgebiz B, Bagcaz S, Ozdemir MG, Inan G. A real-time anatomy ıdentification via tool based on artificial ıntelligence for ultrasound-guided peripheral nerve block procedures: an accuracy study. J Anesth 2021;35:591-4. [Crossref] [PubMed]
- Xu Z, Wu S, Li X, Liu C, Fan S, Ma C. Ultrasound-Guided Transforaminal Injections of Platelet-Rich Plasma Compared with Steroid in Lumbar Disc Herniation: A Prospective, Randomized, Controlled Study. Neural Plast 2021;2021:5558138. [Crossref] [PubMed]
- Abdelwahab EH, Hodeib AA, Marof HM, Fattooh NH, Afandy ME. Ultrasound-Guided Erector Spinae Block Versus Ultrasound-Guided Thoracic Paravertebral Block for Pain Relief in Patients With Acute Thoracic Herpes Zoster: A Randomized Controlled Trial. Pain Physician 2022;25:E977-85.


