
Relationship between development of the condylar cortex and the changes in condyle morphology: a cone-beam computed tomography (CBCT) observational study
Introduction
A correct and in-depth understanding of the mandibular condyle morphology may help clinicians judge the normal range of morphological variations of asymptomatic patients or the pathological conditions correctly (1). Frequently, some normal condyles with relatively rare morphologies are mistaken for abnormal condyles. Many doctors with little clinical experience in this area are at risk to misdiagnose a temporomandibular joint (TMJ) with no pathologically relevant condylar bone changes as temporomandibular joint osteoarthritis (TMJOA). This misdiagnosis will directly affect clinical decision making, which highlights the importance to correctly understand normal condyles of different shapes. The morphology of mandibular condyles has been investigated for years. According to the recent studies, the changes of condyle morphology seem to be closely related to the age among the possible influencing factors (2-6). However, no study has focused yet on the changes of condyle morphology in teenagers and young people. Based on the results of recent studies, the development of condyle cortication is associated with the chronological age (7), and not all of the bilateral condyles had the same shape (4) or cortical state. In that way, compared with the correlation of the age and condyle morphology, the relationship between cortical bone and morphology can better reflect the influence of growth on condyle morphology. Hence, the aim of the present study was (I) to evaluate the status of condyle cortication and morphology from childhood to early adulthood, and (II) to investigate the relationship between them, which may indicate a potential connection between the development of the condylar cortex and the changes of condyle morphology. We present the following article in accordance with the STROBE reporting checklist (available at https://qims.amegroups.com/article/view/10.21037/qims-22-891/rc).
Methods
The present study was an observational study.
Subjects
TMJ cone-beam computed tomography (CBCT) images of 505 orthodontic patients (1,010 sides of TMJ) from January, 2014 to December, 2015 were retrospectively collected from the radiographic database in Peking University School and Hospital of Stomatology, and the information on age and gender was also verified in this process. All the included patients had their images taken in a standing position, and were asked to keep the maximum intercuspation to ensure the ideal position of the condyles and to prevent motion artifacts during exposure. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The ethical approval was obtained from the Institutional Review Board of Peking University School and Hospital of Stomatology (No. PKUSSIRB-201520035). Because our study did not disclose any private patient data, individual consent for this retrospective analysis was waived.
The inclusion criteria of the patients were (I) age from 12 to 30 years old; (II) no abnormal clinical symptoms such as joint sounds or pain; (III) no history of trauma and/or fractures; (IV) no tumors or dysplasia; (V) no osseous defects of mandibular condyle; (VI) has bilateral condyles shown in one CBCT image; (VII) CBCT images of the patient has no artifacts.
All CBCT images were acquired with one NewTom VGi CBCT unit (Quantitative Radiology, Verona, Italy). Exposure parameters for CBCT images were 110 kVp, 5.58–18.07 mAs and the field of view (FOV) was 15 cm × 15 cm. Acquired images were subsequently reconstructed with a voxel-size of 300 µm.
Calibration of images
To standardize the observation condition, the axial, coronal and sagittal views of the condyle were calibrated along the long axes of the condylar heads (Figure S1). In order to unify the consistency of the observers, 20 condyles, which were not included in the study samples, were selected to train and standardize the process of image calibration.
Observation
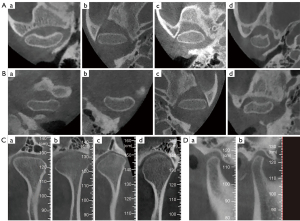
Classification of mandibular condyle morphology
The condyle morphology was assessed in the calibrated axial, coronal and sagittal views. The process was conducted in the maximum cross-section in axial view and the middle sections in sagittal and coronal views (Figure S2). In the axial view, the morphology of the condyle was classified as concave, convex, plane and others for the anterior and posterior aspects, respectively. In the coronal view, the condyle morphology was classified as plane, convex, angled and round. In the sagittal view, the condyle morphology was classified as round and plane. The example images were shown in Figure 1, which was modified on the basis of the previous studies on condyle morphology (3,8).
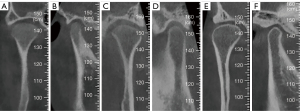
Assessment of mandibular condyle cortication
The superior facet of the condyle including the internal and external poles was evaluated according to the status of the bone cortex. The status of the cortex was classified into three groups:
- Undeveloped cortex of condyle: no evidence of a cortical bone appears in the superior facet of condyle (Figure 2A,2B);
- Developing cortex of condyle: a status between developed and undeveloped cortex of condyle. The density of the cortical bone is increased, but not as dense as that of mature cortical bone (Figure 2C,2D);
- Developed cortex of condyle: continuous and compact cortical bone appears (Figure 2E,2F).
All image data from subjects were assessed and recorded in the middle sections (coronal and sagittal views) across the long axes of the coronal and sagittal orientations and the maximum sections (axial view) perpendicular to the long axes of the coronal and sagittal orientations by two investigators, who have at least 5-year experience in reading CBCT images (RH Ma and JL Feng). Disagreements were resolved by discussion or in case of prevailing disagreement referred to a senior dentomaxillofacial radiologist.
Statistical analysis
Statistical analysis was performed using IBM SPSS Statistics, Version 19 (SPSS, Inc., an IBM Company). Chi-square test was used to determine the correlation of bone cortex formation and condyle morphology classification. When the expected frequency of more than 20% cells was less than 5, or the expected frequency of any one cell was less than 1, Fisher’s Exact test was used. A P value of 0.05 or less was considered significant. To decrease the risk of a type I error in pairwise comparisons, a Bonferroni correction at α’=α/[k(k−1)/2] was used (k is the number of groups) (9).
Results
A total of 505 asymptomatic patients (1,010 TMJs), 173 males and 332 females, were included in the present investigation (Figure 3). For the evaluation of cortical bone of condyle, 278 condyles (27.5%) had no cortical bone at all, 261 condyles (25.8%) had incompletely formed cortical bone and 471 condyles (46.6%) had completely formed cortical bone. Cortical bone was first observed at age 12 years in both genders. The mean age for the condyle without formation of cortical bone (15.11±2.71 years) for the males was significantly higher than that (14.25±2.60 years) for the females (P=0.008). The mean age for developing cortical bone for the females and males were 18.65±3.45 and 19.45±3.92 (P=0.09), respectively. The mean age for developed cortical bone for the females and males were 23.86±3.73 and 23.63±3.36 (P=0.58), respectively (Table 1). For the developing and developed groups, there were no significant differences in the average age of the males and the females. There were 103 patients (20.4%) who had different types of cortication in both condyles.
Table 1
| Gender | Undeveloped | Developing | Developed |
|---|---|---|---|
| Female | 14.25±2.60 | 18.65±3.45 | 23.86±3.73 |
| Male | 15.11±2.71 | 19.45±3.92 | 23.63±3.36 |
| P value | 0.008* | 0.09 | 0.58 |
| 95% CI for the mean difference | −1.49 to −0.23 | −1.71 to 0.12 | −0.58 to 1.03 |
*, α=0.05. SD, standard deviation; 95% CI, 95% confidence interval.
The number and percentages of different kinds of condyle morphology in relation to different types of bone cortication of the condyles are shown in Table 2. In the present study, a total of 64 variations of condyle morphology were observed. Figure 4 exhibits the most common condyle morphologies, which accounted for 3% of the total samples or above. The condyle morphology with a plane form in the anterior aspect, a convex form in the posterior aspect, a convex form in the coronal view and a round form in the sagittal view was the most often recorded condyle morphologies (133/1,010, 13.2%).
Table 2
| Cortication | Anterior (axial)† | Posterior (axial) | Superior (coronal) | Superior (sagittal) | Total | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Concave | Convex | Plane | Other | Concave | Convex | Plane | Other | Plane | Convex | Angled | Round | Round | Plane | |||||
| Female | ||||||||||||||||||
| Undeveloped | 30 (22.9)‡ | 32 (24.4) | 64 (48.9) | 5 (3.8) | 2 (1.5) | 103 (78.6) | 26 (19.8) | 0 (0.0) | 6 (4.6) | 83 (63.4) | 3 (2.3) | 39 (29.8) | 121 (92.4) | 10 (7.6) | 131 (19.7) | |||
| Developing | 35 (21.2) | 44 (26.7) | 77 (46.7) | 9 (5.5) | 1 (0.6) | 135 (81.8) | 28 (17.0) | 1 (0.6) | 23 (13.9) | 80 (48.5) | 10 (6.1) | 52 (31.5) | 138 (83.6) | 27 (16.4) | 165 (24.8) | |||
| Developed | 111 (30.2) | 73 (19.8) | 156 (42.4) | 28 (7.6) | 2 (0.5) | 316 (85.9) | 48 (13.0) | 2 (0.5) | 94 (25.5) | 162 (44.0) | 28 (7.6) | 84 (22.8) | 301 (81.8) | 67 (18.2) | 368 (55.4) | |||
| Male | ||||||||||||||||||
| Undeveloped | 40 (27.2) | 42 (28.6) | 58 (39.5) | 7 (4.8) | 0 (0.0) | 107 (72.8) | 40 (27.2) | 0 (0.0) | 9 (6.1) | 81 (55.1) | 14 (9.5) | 43 (29.3) | 140 (95.2) | 7 (4.8) | 147 (42.5) | |||
| Developing | 24 (25.0) | 42 (43.8) | 27 (28.1) | 3 (7.3) | 1 (1.0) | 68 (70.8) | 27 (28.1) | 0 (0.0) | 8 (8.3) | 56 (58.3) | 7 (7.3) | 25 (26.0) | 86 (89.6) | 10 (10.4) | 96 (27.7) | |||
| Developed | 39 (38.9) | 22 (21.4) | 39 (37.9) | 3 (2.9) | 2 (1.9) | 80 (77.7) | 21 (20.4) | 0 (0.0) | 24 (23.3) | 49 (47.6) | 18 (17.5) | 12 (11.7) | 83 (80.6) | 20 (19.4) | 103 (29.8) | |||
| Total | 279 (27.6) | 255 (25.3) | 421 (41.7) | 55 (5.4) | 8 (0.8) | 809 (80.1) | 190 (18.8) | 3 (0.3) | 164 (16.2) | 511 (50.6) | 80 (7.9) | 255 (25.3) | 869 (86.0) | 141 (14.0) | 1,010 (100.0) | |||
†, anterior (axial): anterior morphology in axial view; posterior (axial): posterior morphology in axial view; superior (coronal): superior morphology in coronal view; superior (sagittal): superior morphology in sagittal view; ‡, number with percentage in the brackets. CBCT, cone-beam computed tomography.
Table 3 shows the P values obtained from the comparisons among different condyle bone cortication at different view. For the anterior aspect, there was no significant difference among the three kinds of bony cortication in the females (P=0.11), while in the males the bony difference between developing and developed groups was statistically significant (P=0.007). For the posterior morphology, there was no significant difference among the three kinds of bony cortication in both genders (P=0.319 for female, P=0.720 for male). For the coronal view of the condyles, there were significant differences of condyle bone conditions between undeveloped and developed (P<0.001 for both genders), developing and developed subgroups (P=0.01 for female, P=0.001 for male) in both genders. Besides, the difference of condyle bone condition between undeveloped and developing subgroups was significant for female (P=0.008). The analysis for sagittal view also indicated that there were significant differences between undeveloped and developed subgroups (P=0.004 for female, P<0.001 for male) in both genders.
Table 3
| P value | Axial view (anterior)† | Axial view (posterior) | Coronal view | Sagittal view | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Undeveloped | Developing | Undeveloped | Developing | Undeveloped | Developing | Undeveloped | Developing | ||||
| Female | |||||||||||
| Developed | 0.11* | 0.319 (0.309, 0.328) | <0.001§** | 0.01§** | 0.004§** | 0.606§ | |||||
| Developing | 0.008§** | – | 0.02§ | – | |||||||
| Male | |||||||||||
| Developed | 0.27§ | 0.007‡§** (0.005, 0.008) | 0.720 (0.711, 0.729) | <0.001§** | 0.001§** | <0.001§** | 0.076§ | ||||
| Developing | 0.09§ | – | 0.79§ | – | 0.09§ | – | |||||
†, anterior morphology in axial view; posterior morphology in axial view; superior morphology in coronal view; superior morphology in sagittal view; ‡, if the expected frequency of more than 20% cells is less than 5, or the expected frequency of any one cells is less than 1, Fisher’s Exact test-Monte Carlo method was used, which has a 95% confidence interval; *, α=0.050; §, a Bonferroni correction at α’=0.017 was used; **, P value ≤0.017.
Table 4 shows the percentage of condyle morphology in a combined observation of sagittal and coronal view. For the females, the plane form in sagittal and the angled form in coronal views was the most often recorded condyle morphology (31.7%) and significantly higher than the plane form in sagittal view combined with other coronal morphologies (22.0% for coronal plane, 13.2% for coronal convex and 12.0% for coronal round, P=0.002). Meanwhile, no significant difference was found for males among the associated morphologies in the sagittal and coronal views (P=0.985).
Table 4
| Sagittal view (superior) | Coronal view (superior) | |||
|---|---|---|---|---|
| Plane | Convex | Angled | Round | |
| Female | ||||
| Round | 78.0% [96] | 86.8% [282] | 68.3% [28] | 88.0% [154] |
| Plane | 22.0% [27] | 13.2% [43] | 31.7%* [13] | 12.0% [21] |
| Male | ||||
| Round | 87.8% [36] | 89.2% [166] | 89.7% [35] | 90.0% [72] |
| Plane | 12.2% [5] | 10.8% [20] | 10.3% [4] | 10.0% [8] |
*, P=0.002, a Bonferroni correction at α’=0.008 was used. CBCT, cone-beam computed tomography.
Discussion
A full recognition of the morphology and the level of condyle cortication of healthy condyles would provide a baseline when the normal and the pathological conditions need to be distinguished. The present study mainly evaluated the status of condyle cortication and condyle morphology and investigated the relationship between the development of the condylar cortex and the changes of condyle morphology. In view of the relatively high diagnostic accuracy for the detection of TMJ bony changes, CBCT was used to observe the mandibular condyles (10-13). Bayrak et al. (7) demonstrated that the cortication of the condyle occurred between the age 13–19 years, and all stages of the cortication in the condyle of males occurred later than in females. Similarly, Lei et al. (14) reported that the cortical bone began to form around the periphery of the condyles during the age of 12–14 years, and completely corticated around 21–22 years. The results of the present investigation were partly consistent with the previous works (7,14-16). The mean age of the undeveloped bony cortication in females was lower than that in males (P<0.05), which may mean that cortical bone appears in girls earlier than in boys. However, there were no significant differences of the mean ages in the developing and developed bony cortication groups between both genders. Females in the present study were twice as many as males, which may have an impact on the present statistical results. However, when considering that the female to male ratio is similar to the previous studies (7,14), the results may be reasonable and acceptable.
Based on the classification of previous works, various condylar types in axial, coronal and sagittal CBCT views were established for the present work. Yale et al. (3) indicated that the four basic types of coronal superior surface of condyles (flattened, convex, angled and rounded) constitute 98.8% of the total sample, and convex in the anterior, posterior and superior surface was the most common morphology. The classification of superior surface morphology in the coronal view was consistent with the classification reported by Yale et al., but the classification of axial morphology was modified into concave, convex, plane and other, because it was found that some axial morphologies encountered could not be classified into the first three morphologies. Besides, the superior facet morphology in the sagittal view were classified into round and plane, so these two types of morphology in sagittal view was also assessed in the present research. A total of 1,010 CBCT images of TMJ were observed, the largest proportion of each view was plane (anterior edge of axial view), convex (posterior edge of axial view), convex (superior edge of coronal view) and round (superior edge of sagittal view). It could be demonstrated that the morphologies mentioned above were relatively stable for TMJ in an asymptomatic population. Furthermore, from the present study, the investigators found that there was no certain relationship between the morphologies in sagittal and coronal views, except the number of angled-shape in sagittal and plane form in coronal view was relatively high in female. It is worth to be noted that the heart-shaped superior facet in coronal view was mentioned in the reference (17) which was not observed in the present research. This may be due to the relatively small sample size. Therefore, it is crucial to use a large sample size to estimate the morphologies of condyle with no bone changes integrally and systematically in the future.
Yalcin et al. (2) demonstrated that angled shape condyle is significantly common between the ages of 30 to 59 compared to the ages of 18 to 29 and over 60 years. Nevertheless, no research has focused on the relationship between condylar development and morphology up to date. The formation of condylar cortical bone was actually correlated with the chronologic age (7,18). Besides, not all of the bilateral condyles had the same shape (4) or cortical state, which was corroborated in the present study, so it was more rational to use the status of bony cortication to investigate the relationship between the development of the condylar cortex and morphology. According to the results, the morphology has undergone subtle changes with the progress of development. For dental clinicians, especially for young doctors, these findings are very helpful in differentiating normal condyle morphology without bone changes from condyles with bone changes. For instance, the flattening or erosion of the condyle should be differentiated from the flat and angled shape of normal condyle. Based on the present results it seems that the morphology of the mandibular condyle is associated with different stages of bony cortication, and the plane morphology of the superior facet may be related with the bone remodeling. The reasons for this phenomenon need to be further explored and verified. As for the influencing factors for condyle morphology, it may also include malocclusion (2,19), temporomandibular disordors (TMD) or TMJOA (20-23), which were not assessed in the current investigation and should be specifically investigated in the future studies.
Conclusions
The condyle shape gradually changes with growth and development of the condyle bone cortex. The more mature the bone cortex is, the higher the probability that the condyle will have an uneven shape, which may mean that the condyle morphology may change due to remodeling during growth and development.
Acknowledgments
Funding: This work was supported by the National Natural Science Foundation of China (No. 81671034), PKU-Baidu Fund (project No. 2020BD037), and Research Foundation of Peking University School and Hospital of Stomatology (No. PKUSS20220116).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://qims.amegroups.com/article/view/10.21037/qims-22-891/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-22-891/coif). The authors report that this work was supported by the National Natural Science Foundation of China (No. 81671034), PKU-Baidu Fund (No. 2020BD037), and Research Foundation of Peking University School and Hospital of Stomatology (No. PKUSS20220116). The authors have no other conflicts interest to declare.
Ethical Statement:
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Yasa Y, Akgül HM. Comparative cone-beam computed tomography evaluation of the osseous morphology of the temporomandibular joint in temporomandibular dysfunction patients and asymptomatic individuals. Oral Radiol 2018;34:31-9. [Crossref] [PubMed]
- Yalcin ED, Ararat E. Cone-Beam Computed Tomography Study of Mandibular Condylar Morphology. J Craniofac Surg 2019;30:2621-4. [Crossref] [PubMed]
- Yale SH, Allison BD, Hauptfuehrer JD. An epidemiological assessment of mandibular condyle morphology. Oral Surg Oral Med Oral Pathol 1966;21:169-77. [Crossref] [PubMed]
- Singh B, Kumar NR, Balan A, Nishan M, Haris PS, Jinisha M, Denny CD. Evaluation of Normal Morphology of Mandibular Condyle: A Radiographic Survey. J Clin Imaging Sci 2020;10:51. [Crossref] [PubMed]
- Kijima N, Honda K, Kuroki Y, Sakabe J, Ejima K, Nakajima I. Relationship between patient characteristics, mandibular head morphology and thickness of the roof of the glenoid fossa in symptomatic temporomandibular joints. Dentomaxillofac Radiol 2007;36:277-81. [Crossref] [PubMed]
- Saini V, Srivastava R, Rai RK, Shamal SN, Singh TB, Tripathi SK. Mandibular ramus: an indicator for sex in fragmentary mandible. J Forensic Sci 2011;56:S13-6. [Crossref] [PubMed]
- Bayrak S, Halıcıoglu S, Kose G, Halıcıoglu K. Evaluation of the relationship between mandibular condyle cortication and chronologic age with cone beam computed tomography. J Forensic Leg Med 2018;55:39-44. [Crossref] [PubMed]
- de Farias JF, Melo SL, Bento PM, Oliveira LS, Campos PS, de Melo DP. Correlation between temporomandibular joint morphology and disc displacement by MRI. Dentomaxillofac Radiol 2015;44:20150023. [Crossref] [PubMed]
- Armstrong RA. When to use the Bonferroni correction. Ophthalmic Physiol Opt 2014;34:502-8. [Crossref] [PubMed]
- Zain-Alabdeen EH, Alsadhan RI. A comparative study of accuracy of detection of surface osseous changes in the temporomandibular joint using multidetector CT and cone beam CT. Dentomaxillofac Radiol 2012;41:185-91. [Crossref] [PubMed]
- Honda K, Larheim TA, Maruhashi K, Matsumoto K, Iwai K. Osseous abnormalities of the mandibular condyle: diagnostic reliability of cone beam computed tomography compared with helical computed tomography based on an autopsy material. Dentomaxillofac Radiol 2006;35:152-7. [Crossref] [PubMed]
- Hussain AM, Packota G, Major PW, Flores-Mir C. Role of different imaging modalities in assessment of temporomandibular joint erosions and osteophytes: a systematic review. Dentomaxillofac Radiol 2008;37:63-71. [Crossref] [PubMed]
- Ma RH, Yin S, Li G. The detection accuracy of cone beam CT for osseous defects of the temporomandibular joint: a systematic review and meta-analysis. Sci Rep 2016;6:34714. [Crossref] [PubMed]
- Lei J, Liu MQ, Yap AU, Fu KY. Condylar subchondral formation of cortical bone in adolescents and young adults. Br J Oral Maxillofac Surg 2013;51:63-8. [Crossref] [PubMed]
- Mérida-Velasco JR, Rodríguez-Vázquez JF, Mérida-Velasco JA, Sánchez-Montesinos I, Espín-Ferra J, Jiménez-Collado J. Development of the human temporomandibular joint. Anat Rec 1999;255:20-33. [Crossref] [PubMed]
- Yuodelis RA. The morphogenesis of the human temporomandibular joint and its associated structures. J Dent Res 1966;45:182-91. [Crossref] [PubMed]
- Perschbacher S. Temporomandibular joint abnormalities. In: White SC, Pharoah MJ, editors. Oral and radiology principles and interpretation. 7th edition. Missouri: Mosby; 2014:492-523.
- Bayrak S, Göller Bulut D. Relationship between condyle cortication, sphenooccipital synchondrosis, and chronological age. Oral Radiol 2020;36:190-6. [Crossref] [PubMed]
- Kurusu A, Horiuchi M, Soma K. Relationship between occlusal force and mandibular condyle morphology. Evaluated by limited cone-beam computed tomography. Angle Orthod 2009;79:1063-9. [Crossref] [PubMed]
- Derwich M, Mitus-Kenig M, Pawlowska E. Morphology of the Temporomandibular Joints Regarding the Presence of Osteoarthritic Changes. Int J Environ Res Public Health 2020;17:2923. [Crossref] [PubMed]
- Derwich M, Mitus-Kenig M, Pawlowska E. Temporomandibular Joints' Morphology and Osteoarthritic Changes in Cone-Beam Computed Tomography Images in Patients with and without Reciprocal Clicking-A Case Control Study. Int J Environ Res Public Health 2020;17:3428. [Crossref] [PubMed]
- Lee YH, Hong IK, Chun YH. Prediction of painful temporomandibular joint osteoarthritis in juvenile patients using bone scintigraphy. Clin Exp Dent Res 2019;5:225-35. [Crossref] [PubMed]
- Jeon KJ, Lee C, Choi YJ, Han SS. Analysis of three-dimensional imaging findings and clinical symptoms in patients with temporomandibular joint disorders. Quant Imaging Med Surg 2021;11:1921-31. [Crossref] [PubMed]




