
Confirmation of the third lumbar transverse process syndrome by clinical treatment and magnetic resonance imaging: a case description
Introduction
The third lumbar transverse process syndrome was first proposed by traditional Chinese medicine (TCM), which asserted that the disease was related to the anatomical position, structure, and mechanical properties of the third lumbar transverse process (1,2). However, the pathological changes of this disease are not uniform. Most patients with similar symptoms usually relieve their pain by rest, activity reduction, weight reduction, or block therapy. Furthermore, routine imaging examinations, such as X-rays, computed tomography (CT), and magnetic resonance imaging (MRI), provide no clear evidence of the disease.
Clinically, the third lumbar transverse process syndrome is most often characterized by low back and leg pain. Due to the lack of understanding of this disease by clinicians and radiologists, the pain is often attributed to factors such as lumbar muscle strain and lumbar disc herniation. Therefore, few patients seek further medical care or further imaging due to worsening pain.
T2-weighted fat-suppressed MRI, including the scan range of the third lumbar vertebral body, plays an important role in diagnosing this disease. However, in the past, conventional imaging examinations were not sufficient to confirm the existence of this disease. In the case presented here, we confirmed the existence of the third lumbar transverse process syndrome through a site-specific T2-weighted fat-suppressed MRI and clinical diagnosis.
Case presentation
The patient, a 52-year-old woman, had experienced lumbar discomfort for more than 1 year. In the previous 1.5 months, she had experienced recurrent episodes of right lumbar pain with pain radiating to the right lower limb. The patient’s lumbar movement was limited in its anterior curvature, dorsiflexion, lateral rotation, and lateral flexion, but the pain could be relieved in a seated position. Physical examination revealed the following findings: the bilateral knee-tendon reflex was positive, the bilateral straight leg-raising test was negative, the bilateral hip abduction and external rotation test was negative, there was tenderness in the right transverse process of the third lumbar spine; the reverse traction test of the right psoas major was positive, and the patient did not have a pathological reflex.
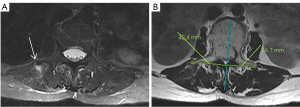
After having taken the patient’s medical history and physical examination, the clinician suspected “the third lumbar transverse process syndrome”, which was followed by X-ray and MRI examinations of the lumbar region. The X-ray examination showed that the lumbar spine was slightly curved to the right, and there was no developmental variation in the adjacent thoracic and lumbar vertebrae. The MRI showed that the right side of the third lumbar transverse process was longer than the left (4.24 cm on the right side and 3.47 cm on the left side). T2-weighted fat-suppressed images showed a flaky, slightly higher signal in the region adjacent to the apex of the right side of the third lumbar transverse process, with swelling of the surrounding muscles, tendons, and fascia (Figure 1). These accompanied a disc bulge from the first lumbar to the first sacral vertebrae. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki (as revised in 2013). Written informed consent was provided by the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Pathogenesis
This patient presented with low back pain associated with marked tenderness in the right transverse process of the third lumbar spine. The location of the pain was closely related to MRI findings. The psoas major, quadratus lumborum, and erector spinae muscle adjacent to the tip of the right transverse process showed obvious fluid exudation. We believe that the occurrence of this disease was closely related to a congenital developmental variation and that the mechanical variations of the third lumbar spine were acquired.
There may be variations in the morphology of the transverse processes, such as excessive length of the transverse process and left-right asymmetry (3). However, congenital developmental variations in the transverse process of the third lumbar spine may be associated with the development of the superior vertebral body. When a caudal shift of the thoracic-lumbar (T-L) border occurs, it will affect the transverse process of the first lumbar vertebra, even the second lumbar vertebra, promoting the transformation of the transverse process into ribs, which induces the lumbar spine to assume the characteristics of the thoracic spine. This process may result in spinal stress and, to some extent, promote the growth of the transverse process of the third lumbar vertebra (4).
Many muscles are attached to the transverse process of the lumbar spine, including the psoas major and quadratus lumborum in the front, the transversospinalis muscles (part of erector spinae) in the back, the thoracolumbar fascia (middle layer) formed by the extension of the transversus abdominis and the internal oblique abdominis tendon membranes on the lateral side, and the intertransverse muscle and ligament between the transverse processes. The stresses on the tendons, ligaments, and fascia of these muscles all act on the tip of the transverse process. This process will likely increase the transverse process’ length under such mechanical stimulation (5,6).
The third lumbar vertebra is the most convex vertebral body on the physiological curvature of the lumbar spine and is also the active center of the lumbar spine. In addition, the transverse process of the third lumbar vertebra is the longest of the transverse processes among all lumbar vertebrae. Therefore, during flexion, extension, and rotation, the third lumbar transverse process becomes the most concentrated point of tensile stress, which may also increase the length of the transverse process (7,8).
In this case, the anatomy of the patient’s first and second lumbar vertebrae was normal, and there was no anatomical variation, so the variation of the transverse process of the third lumbar vertebra of the patient was more likely to have been caused by acquired mechanical factors. When the muscles of the waist and abdomen contract strongly, it becomes easier for the attached ligaments, tendons, and fascia to form aseptic inflammation, and, in severe cases, an avulsion fracture of the transverse process may occur (9). The lesion at the tip of the transverse process of the third lumbar vertebra affects the nerve, especially the lateral branches of the first to third posterior spinal nerve branches immediately behind the transverse process, which travel dorsally and laterally through the intertransverse muscle and the surrounding soft tissues. This process causes pain in the corresponding area.
Differential diagnosis
In the past, the diagnosis of the third lumbar transverse process syndrome was mostly made according to the interrogation and palpation of TCM. The diagnosis was confirmed according to the effects of rest, moderate massage, or acupuncture treatment. The disease is rarely confirmed via combination with imaging examinations, especially MRI of a specific scan range, which may lead to misdiagnosis.
Clinically, many diseases may lead to pain in the lumbar and legs, including degenerative diseases (4), inflammatory diseases, and organic diseases (10). Most clinicians and radiologists do not fully understand this disease and only allow patients to perform routine imaging examinations. However, some abnormalities, such as lumbar degeneration and edema of the lumbar muscle, can be identified in these examinations, which often mistake the disease for hyperostosis, lumbar disc herniation, or lumbar muscle strain, and delay the treatment of the disease. From the radiologist’s point of view, conventional MRI does not usually pass through the transverse process of the lumbar spine. Although X-rays and CT can observe some abnormalities in the transverse process, such as long transverse process or transverse process asymmetry, a definite diagnosis is difficult to make without combining the typical clinical feature of obvious tenderness in the transverse process of the third lumbar spine.
Radiologists can add the T2-weighted fat-suppressed MRI, including the scan range of the third lumbar vertebral body according to the typical clinical manifestations, to increase the contrast between soft tissues and better show the fluid exudation of the attached ligaments, tendons, and fascia. A T2-weighted fat-suppression sequence does not require high magnetic field uniformity of the device, which makes this an easy method to use in the basic scanning sequence of the third lumbar transverse process syndrome.
The third lumbar transverse process syndrome is not uncommon in clinical practice. Clinicians and radiologists should consider the existence of this disease in patients with low back pain, especially in patients with tenderness in the third lumbar transverse process. Routine MRI and T2-weighted fat-suppression MRI, including the third lumbar transverse process, are of great value in diagnosing this disease.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-22-520/coif). All authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki (as revised in 2013). Written informed consent was provided by the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Yu JN, Guo CQ, Hu B, Liu NG, Sun HM, Xu H, Wu HX, Guo Y, Liang CX, Chen ZX, Li XH. Effects of acupuncture knife on inflammatory factors and pain in third lumbar vertebrae transverse process syndrome model rats. Evid Based Complement Alternat Med 2014;2014:892406. [Crossref] [PubMed]
- Zhang A, Zhang L, Zhang S. Fifty cases of transverse process syndrome of third lumbar vertebra treated by acupuncture therapy according to acupotomy. Zhongguo Zhen Jiu 2015;35:199. [PubMed]
- Li F, Bi D. The third lumbar transverse process syndrome treated with acupuncture at zygapophyseal joint and transverse process:a randomized controlled trial. Zhongguo Zhen Jiu 2017;37:810-3. [PubMed]
- Barnes E. The atlas of developmental fild anomalies of human skeleton. John Wiley & Sons; 2012.
- Guo CQ, Dong FH, Li SL, Qiao JL, Jiang ZI, Liu NG, Chen ZL. Effects of acupotomy lysis on local soft tissue tension in patients with the third lumbar vertebrae transverse process syndrome. Zhongguo Zhen Jiu 2012;32:617-20. [PubMed]
- Jiao L, Xiao Y, Chi Z, Zhu D, Ouyang X, Xu W, You J, Luo Z, Yuan F. Acupotomy for third lumbar vertebrae transverse process syndrome: A protocol for systematic review. Medicine (Baltimore) 2020;99:e21072. [Crossref] [PubMed]
- Huang QQ, Liu SS, Liang GQ. Advances in the study of anatomy and biomechanics of lumbosacral transitional vertebrae. Zhonghua Wai Ke Za Zhi 2019;57:156-60. [PubMed]
- Wei JL, Zhu YB, Zhao DW, Chen W, Wang J, Wang H, Lv JL, Zhang T, Cheng L, Zhang YZ. Dynamic Change of Lumbar Structure and Associated Factors: A Retrospective Study. Orthop Surg 2019;11:1072-81. [Crossref] [PubMed]
- McGuire FP, Vu L, Hodgin CM, Bashaw RT, Pfeiffer DC. Lumbar Transverse Process Stress Fracture in an Elite Rower: A Case Report. Orthop J Sports Med 2020;8:2325967120910146. [Crossref] [PubMed]
- Will JS, Bury DC, Miller JA. Mechanical Low Back Pain. Am Fam Physician 2018;98:421-8. [PubMed]


