
Coronary artery calcium score scan at 100 kVp with tin filtration (Sn100 kVp) prior to coronary computed tomography angiography for overall radiation dose reduction: a prospective cohort study
Introduction
Reducing the radiation dose of coronary computed tomography angiography (CCTA), a widely used diagnostic modality for coronary artery disease (CAD), is a concern for medical centers throughout the globe (1,2). The radiation dose should be as low as reasonably achievable, as a higher radiation dose has been reported to possibly damage DNA with an effective dose (ED) of ionizing radiation over 6 mSv (3). The coronary artery calcium score (CACS) scan, with great clinical significance (4,5), is performed to assess the graded increased risk of future coronary events, heart failure, and mortality (6-8). In addition, CACS scans also have the potential to the reduce radiation dose during subsequent cardiac imaging (9-11).
Previous studies have reported that the CACS scan may guide reduction of the scan length during CCTA scanning (10,11) and that the overall radiation dose can be determined by the ED of both the CACS and CCTA (10). However, tube voltage at 100 kVp with tin filtration (Sn100 kVp), which can lead to a significantly low radiation dose during the CACS scan, is feasible and highly accurate compared to the standard 120 kVp (9,12). Debates have emerged on the need for a CACS scan to be performed before CCTA imaging, and although the Society of Cardiovascular Computed Tomography (SCCT) guidelines (13) recommends the use of CACS, there is no consensus or guideline regarding this protocol. Therefore, we aimed to investigate whether the CACS scan can reduce the overall radiation dose in addition to reducing the scan length. If so, there will be additional benefits for patients (6), including exposure to a lower radiation dose, among others. We present the following article in accordance with the STROBE reporting checklist (available at https://qims.amegroups.com/article/view/10.21037/qims-21-1129/rc).
Methods
Study population
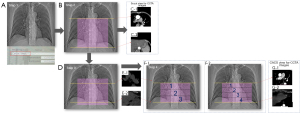
This prospective cohort study was approved by the Ethics Committee of Huadong Hospital, and written informed consent was provided by all patients. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). We enrolled 297 consecutive patients [152 women, 145 men; mean age 64.15±11.05 years; age range 23 to 91 years; mean body mass index (BMI) 24.09±3.27 kg/m2; BMI range 15.99 to 34.38 kg/m2] between March 2021 and September 2021 with suspected CAD undergoing CCTA examination. The first 150 consecutive patients (group A, n=150) were scanned with CACS for guiding CCTA scanning range, whereas the remaining consecutive patients (151–297; group B, n=147) were not scanned with CACS to guide the CCTA range (Figure 1). The inclusion criteria were age over 18 years and the ability to control and hold breath. Patients were excluded if they had (I) allergies to iodine contrast agent, (II) severe renal insufficiency, (III) decompensated cardiac insufficiency, (IV) a history of medication use to control their heart rate, or (V) a coronary artery bypass graft.
CT protocol and image reconstruction
All participants underwent CT using a new generation, dual-source CT scanner (Somatom Drive; Siemens Healthineers, Erlangen, Germany). A CACS scan was performed for group A to plan the scan range of CCTA using the following parameters: a tube voltage with Sn100 (Figure 2), an automated anatomical tube current modulation with 188 mAref.qual (CARE Dose 4D; Siemens Healthineers), and a data acquisition window (R-R interval) set at 70%. For CCTA imaging of both groups, the collimation was 2×64×0.6 mm, and the rotation time was 0.28 seconds per rotation. A prospective electrocardiogram (ECG)-triggered sequence acquisition mode (step and shoot) was used, and scanning was performed from the cranium to the cauda. An automated anatomical tube current modulation technique with 380 mAsref.qual (CARE Dose 4D; Siemens Healthineers) and an attenuation-based tube voltage selection (ATVS) with 120 kVref.qual (ATVS, CARE kV; Siemens Healthineers) were used, with the range of exposure dose (ECG pulsing) set at 30–80%. The bolus tracking technique was used for threshold monitoring at the aortic root for coronary arteries with an enhancement threshold of 80 Hounsfield units (HU) and a delay time of 7 seconds. Prewarmed contrast medium [CM; iobitridol, 350 mg iodine (mgI)/mL] was injected using an 18-G closed intravenous catheter system with an Ulrich high-pressure syringe. For CCTA, the CM was administered according to the patient’s weight (0.8 mL/kg with a 13-s injection duration), and saline was administered at the same delivery rate with a 10-second injection duration.
For the CACS scan, the images were reconstructed with a 3.0-mm slice thickness and image reconstruction interval using a medium sharp algorithm (B35f) with an advanced modeled iterative reconstruction (strength level 3) algorithm. For CCTA imaging, the slice thickness and image reconstruction interval with the Advanced Modeled Iterative Reconstruction (ADMIRE; strength level 4, Siemens Healthineers) algorithm for coronary arteries were 0.6 mm and 0.4 mm, respectively.
Image analysis
Qualitative analysis was performed by 2 independent radiologists (one with 8 years of experience in chest imaging and the other with over 15 years of experience in chest imaging) using a 5-point Likert scale: 1= poor opacification, insufficient for diagnosis; 2= suboptimal opacification, low diagnostic confidence; 3= acceptable opacification, sufficient for diagnosis; 4= good opacification of proximal and distal segments; and 5= excellent opacification of proximal and distal segments (14).
Each CCTA imaging was diagnosed within 48 hours by both independent radiologists (usually a junior radiologist with 1–5 years of experience in chest diagnosis and another senior radiologist with over 10 years of experience in chest diagnosis) who did not participate in this study. The CT reports of all participants were analyzed in 2 categories: (I) there was a definitive diagnosis for diagnostic CT reports; and (II) there was motion artifact, other artifacts affected the diagnosis, or the image quality could not be diagnosed for nondiagnostic CT reports.
Actual heart length
The actual heart length was calculated as follows: the table position on the image of the termination of the coronary arteries minus the table position on the image of the origin of the coronary arteries, plus the thickness of the image (0.6 mm).
Radiation dose
The radiation dose of calcium score and CCTA were recorded using the dose-length product (DLP) and volume CT dose index (CTDIvol), which were automatically provided by the CT scanner. Radiations associated with the scout view and the automatic bolus tracking technique were excluded. The ED was estimated by multiplying the DLP by a conversion factor of 0.026 (3) for coronary arteries.
Statistical analyses
The SPSS 26.0 software (IBM Corp., Armonk, NY, USA) was used for statistical analysis. The Levene test was used to verify the homogeneity of variance, while the Shapiro–Wilk test was used for normal distribution. Measurement data that conformed to the normal distribution are expressed in the form of mean ± SD, whereas data that did not conform to the normal distribution are described as median and interquartile range [expressed as M (P25, P75)]. The count data are expressed as frequencies and percentages. If the variances of the basic patient data and radiation parameters of the 2 groups of data were homogeneous, an independent sample t-test was performed, and if the variances were not uniform, the Wilcoxon rank-sum test was performed. Count data and subjective image scores were tested using the chi-squared test. The kappa test was used to determine the consistency between the subjective scores of different physicians. A k value between 0.21 and 0.40 indicated poor consistency, that between 0.41 and 0.60 indicated moderate consistency, and that between 0.61 and 0.80 indicated good consistency. The statistical significance level was set at P<0.05.
Results
All participants in group A (with CACS) finished CCTA imaging successfully with no rescans required, whereas 2 patients in group B (without CACS) were scanned twice because their coronary arteries had not been included in the scan range at the first scan. There were no significant differences in gender, age, height, weight, BMI, and heart rate between the 2 groups (Table 1).
Table 1
| Characteristics | Group A (N=150) | Group B (N=147) | P value |
|---|---|---|---|
| Male/female | 66/84 | 79/68 | 0.093 |
| Age (years) (P25, P75) | 64.0 (57.0, 71.0) | 66.0 (59.0, 72.0) | 0.259 |
| Height (cm) (P25, P75) | 1.64 (1.58, 1.70) | 1.65 (1.59, 1.72) | 0.136 |
| Weight (kg) (P25, P75) | 62.25 (57.1, 73.0) | 69.0 (58.0, 75.0) | 0.111 |
| BMI, mean ± standard deviation | 23.95±3.13 | 24.23±3.41 | 0.455 |
| HR (bpm) [P25, P75] | 70 [64, 80] | 72 [65, 81] | 0.467 |
BMI, body mass index; HR, heart rate; bpm, beats per minute.
In group A, there were 115 (76.7%) participants scanned at 90 kV, 22 (14.7%) scanned at 100 kV, 8 (5.3%) scanned at 110 kV, and 5 (3.3%) scanned at 120 kV; meanwhile in group B, 84 (57.1%) patients were scanned at 90 kV, 45 (30.6%) were scanned at 100 kV, 12 (8.2%) were scanned at 110 kV, and 6 (4.1%) were scanned at 120 kV; this showed a significant difference (P<0.001) between the groups. In group A, 149 patients underwent 3 scans of CCTA, and 1 patient underwent 4 scans of CCTA; meanwhile, in group B, 36 patients underwent 3 scans of CCTA, 109 patients underwent 4 scans of CCTA, and 2 patients underwent 5 scans of CCTA; this also showed a significant difference (P<0.001) between groups. However, the actual heart lengths were similar between groups. The CTDIvol of CCTA (16.13; P<0.04), DLP of CCTA (166.90; P<0.001), ED of CCTA (4.34*0.026; P<0.001), and overall ED (4.57*0.026; P<0.001) of group A showed significant differences compared to group B (36 of 3 scans at 10.35 cm, 109 of 4 scans at 13.80 cm, 2 of 5 scans at 17.25 cm; CTDIvol of CCTA at 18.30 mGy; DLP of CCTA at 235.60 mGy*cm; ED of CCTA at 6.13 mSv; overall ED at 6.13 mSv), whereas the qualitative analysis and diagnostic CT reports were similar. The details are shown in Table 2.
Table 2
| Parameters | Group A (N=150) | Group B (N=147) | P value |
|---|---|---|---|
| Tube voltage (kV) | 0.004 | ||
| 70 | 0 | 0 | |
| 80 | 0 | 0 | |
| 90 | 115 (76.7%) | 84 (57.1%) | |
| 100 | 22 (14.7%) | 45 (30.6%) | |
| 110 | 8 (5.3%) | 12 (8.2%) | |
| 120 | 5 (3.3%) | 6 (4.1%) | |
| Number of scans (scanning length) | <0.001 | ||
| 3 (10.35 cm) | 149 | 36 | |
| 4 (13.80 cm) | 1 | 109 | |
| 5 (17.25 cm) | 0 | 2 | |
| Actual heart length (cm) | 0.169 | ||
| <10.35 | 149 | 143 | |
| 10.35–13.80 | 1 | 4 | |
| 13.80–17.25 | 0 | 0 | |
| CTDIvol-CACS (P25, P75) | 0.60 (0.49, 0.82) | N/A | N/A |
| DLP-CACS (P25, P75) | 8.00 (6.58, 10.73) | N/A | N/A |
| ED-CACS ×0.026 (mSv) (P25, P75) | 0.21 (0.17, 0.28) | N/A | N/A |
| CTDIvol-CCTA (P25, P75) | 16.13 (12.33, 21.86) | 18.30 (12.94, 26.20) | 0.040 |
| DLP-CCTA (P25, P75) | 166.90 (129.35, 226.23) | 235.60 (169.40, 336.50) | <0.001 |
| ED-CCTA ×0.026 (mSv) (P25, P75) | 4.34 (3.37, 5.88) | 6.13 (4.40, 8.75) | <0.001 |
| ED-whole examination ×0.026 (mSv) (P25, P75) | 4.57 (3.54, 6.18) | 6.13 (4.40, 8.75) | <0.001 |
| Qualitative analysis | |||
| LAD | 4.0 (3.0, 4.0) | 4.0 (3.75, 4.0) | 0.375 |
| LCX | 4.0 (3.0, 4.0) | 4.0 (3.0, 4.0) | 0.131 |
| RCA | 4.0 (4.0, 4.0) | 4.0 (4.0, 4.0) | 0.551 |
| Diagnostic CT reports | 145 | 141 | 0.733 |
| Non-diagnostic CT reports | 5 | 6 | |
The median and interquartile range, expressed as P25, P75. CTDIvol-CACS, volume CT dose index in coronary artery calcium score scan; CTDIvol-CCTA, volume CT dose index in coronary computed tomography angiography; DLP-CACS, dose-length product in coronary artery calcium score scan; DLP-CCTA, dose-length product in coronary computed tomography angiography; DLP-whole-examination, dose-length product in whole examination; ED-CACS, effective dose in coronary artery calcium score scan; ED-CCTA, effective dose in computed tomography angiography; D-whole examination, effective dose in whole examination; kV, kilovolt, millisievert; LAD, left anterior descending; LCX, left circumflex artery; RCA, right coronary artery.
Discussion
Our study used a CACS scan with Sn100 kVp to plan the scan range of CCTA for overall examination of radiation dose reduction, and our results demonstrated the following: (I) A CACS scan with Sn100 kVp could reduce the radiation dose of the CCTA scan by approximately 29.7% due to accurate scan length, which is consistent with previous studies (10,11,15). However, our study also found a significant difference in CTDIvol between the 2 groups, which had not been previously reported with the ATVS algorithm. Leschka et al. (11). did not report the relationship between scan length and tube voltage in detail, whereas our previous study (10) showed that similar CTDIvol was not associated with scan length either on force CT or revolution CT, indicating that the tube voltage selection may change due to the increased scan length (Figure 3). Our study demonstrated that the ED of CCTA could be raised by increased CTDIvol and scan length with the new dual-source CT (Somatom Drive). More importantly, 2 patients were rescanned because some of their coronary arteries had not been included in the first scan, indicating that the CACS scan could reduce the risk of rescans, leading to a lower radiation dose. (II) A CACS scan with tin-filtered 100 kV could reduce the overall ED by approximately 25.5%, with a conversion factor of 0.026. A previous study stated that the ED of CACS scan was the main factor in presenting the main power in terms of overall dose reduction (10), as the overall dose increase with CACS scan only reduces the scan length of CCTA imaging and has no added benefits for patients. The present study showed that a CACS scan with Sn100 kVp contributed to the sufficiently low radiation dose of the CACS scan, and it has also been reported that a CACS scan with Sn100 kVp does not reduce the image quality or accuracy (9,12,16).

Drive CT is an upgraded CT based on the second-generation dual-source CT, which has the same detector width (38.4 mm) and gantry speed (0.28 s per rotation); the number of scans of the step-and-shoot acquisition is used to cover the scan length of each CCTA imaging (Figure 2). In the present study, only 1 patient in group A finished the CCTA imaging with 4 scans, whereas the other 149 underwent 3 scans, which comprised the actual heart length coverage (149<10.35 cm and 1 between 10.35 and 13.80 cm); however, in group B, most of the patients [109] underwent 4 scans, and 2 patients underwent 5 scans, while the actual heart length coverage of 143 patients was <10.35 cm and 10.35–13.80 cm for 4 patients (Table 2). The similar actual heart length (all <13.80 cm) of both groups (P=0.169) indicated that the number of scans required to cover the scan length of CCTA used in group A through CACS scan was more accurate than that in group B, as the overused number of scans led to higher ED in group B. In addition, through the tube voltage distribution, the accurate scan length in group A led to a lower tube voltage than in group B (Figure 3).
The CACS has great clinical benefits for patients (6). The only instance of CACS being mentioned in the SCCT guidelines suggests that CACS may be performed before CCTA scanning to detect and quantify coronary artery calcification (13). However, to date, the guidelines have not stipulated when to perform the scan, and it remains controversial whether it is a part of the entire CCTA examination just before CCTA scanning (at the same time) or an isolated scan. Our results indicated that CACS with Sn100 kVp could be added to the CCTA examination as a necessary component, either because of the accurate calculation of calcification or the low radiation dose, both of which will be beneficial to patients.
This study had some limitations. First, ATVS with 120 kVref.qual may be higher than usual setting like 100 kVref.qual, which may lead to lower ED of both CCTA scanning and overall radiation dose. We speculate that a further reduction in radiation dose could be achieved with a lower tube voltage or narrow range of exposure (30–80%) dose; however, the narrow range could also lead to a possible unsatisfactory image quality of CCTA imaging. Second, in our study, tube voltage below 90 kV in both groups did not appear; thus, we will try to investigate this issue in the future. Third, the accuracy of calcium score by using Sn100 kVp was not evaluated in our study; however, a previous study had already proven the accuracy of calcium score by using Sn100 kVp compared with conventional 120 kVp (9,12,16). Finally, this was a single-center study, which may limit the generalizability of the results. Large, multicenter prospective studies may be designed to generalize these results in the future.
In conclusion, CACS scan with Sn100 kVp prior to CCTA imaging on dual-source CT could reduce the overall radiation dose of the CCTA examination, which would be of great value in the clinical setting, with additional clinical information.
Acknowledgments
Funding: This work was supported by the Youth Medical Talents—Medical Imaging Practitioner Program (No. AB83030002019004), the Health Commission of Shanghai (No. 2018ZHYL0103), the National Natural Science Foundation of China (No. 61976238), and the Shanghai “Rising Stars of Medical Talent” Youth Development Program “Outstanding Youth Medical Talents” (No. SHWJRS [2021]-99).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://qims.amegroups.com/article/view/10.21037/qims-21-1129/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-21-1129/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This prospective cohort study was approved by the Ethics Committee of Huadong Hospital, and written informed consent was provided by all participants. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- LaBounty TM. Reducing Radiation Dose in Coronary Computed Tomography Angiography: We Are Not There Yet. JACC Cardiovasc Imaging 2020;13:435-6. [Crossref] [PubMed]
- Stocker TJ, Deseive S, Leipsic J, Hadamitzky M, Chen MY, Rubinshtein R, Heckner M, Bax JJ, Fang XM, Grove EL, Lesser J, Maurovich-Horvat P, Otton J, Shin S, Pontone G, Marques H, Chow B, Nomura CH, Tabbalat R, Schmermund A, Kang JW, Naoum C, Atkins M, Martuscelli E, Massberg S, Hausleiter J. investigators PV. Reduction in radiation exposure in cardiovascular computed tomography imaging: results from the PROspective multicenter registry on radiaTion dose Estimates of cardiac CT angIOgraphy iN daily practice in 2017 (PROTECTION VI). Eur Heart J 2018;39:3715-23. [Crossref] [PubMed]
- Nguyen PK, Lee WH, Li YF, Hong WX, Hu S, Chan C, Liang G, Nguyen I, Ong SG, Churko J, Wang J, Altman RB, Fleischmann D, Wu JC. Assessment of the Radiation Effects of Cardiac CT Angiography Using Protein and Genetic Biomarkers. JACC Cardiovasc Imaging 2015;8:873-84. [Crossref] [PubMed]
- Xu C, Guo H, Xu M, Duan M, Wang M, Liu P, Luo X, Jin Z, Liu H, Wang Y. Automatic coronary artery calcium scoring on routine chest computed tomography (CT): comparison of a deep learning algorithm and a dedicated calcium scoring CT. Quant Imaging Med Surg 2022;12:2684-95. [Crossref] [PubMed]
- Pan YK, Sun MH, Wang JJ, Chen XB, Kan XJ, Ge YH, Guo ZP. Effect of different reconstruction algorithms on coronary artery calcium scores using the reduced radiation dose protocol: a clinical and phantom study. Quant Imaging Med Surg 2021;11:1504-17. [Crossref] [PubMed]
- Polonsky TS, McClelland RL, Jorgensen NW, Bild DE, Burke GL, Guerci AD, Greenland P. Coronary artery calcium score and risk classification for coronary heart disease prediction. JAMA 2010;303:1610-6. [Crossref] [PubMed]
- Leening MJ, Elias-Smale SE, Kavousi M, Felix JF, Deckers JW, Vliegenthart R, Oudkerk M, Hofman A, Steyerberg EW, Stricker BH, Witteman JC. Coronary calcification and the risk of heart failure in the elderly: the Rotterdam Study. JACC Cardiovasc Imaging 2012;5:874-80. [Crossref] [PubMed]
- Bos D, Leening MJG. Leveraging the coronary calcium scan beyond the coronary calcium score. Eur Radiol 2018;28:3082-7. [Crossref] [PubMed]
- Tesche C, De Cecco CN, Vliegenthart R, Albrecht MH, Varga-Szemes A, Duguay TM, Ebersberger U, Bayer RR 2nd, Canstein C, Schmidt B, Allmendinger T, Litwin SE, Morris PB, Flohr TG, Hoffmann E, Schoepf UJ. Accuracy and Radiation Dose Reduction Using Low-Voltage Computed Tomography Coronary Artery Calcium Scoring With Tin Filtration. Am J Cardiol 2017;119:675-80. [Crossref] [PubMed]
- Jin L, Gao Y, Jiang A, Li Z, Wang P, Li M. Can the Coronary Artery Calcium Score Scan Reduce the Radiation Dose in Coronary Computed Tomography Angiography? Acad Radiol 2021;28:364-9. [Crossref] [PubMed]
- Leschka S, Kim CH, Baumueller S, Stolzmann P, Scheffel H, Marincek B, Alkadhi H. Scan length adjustment of CT coronary angiography using the calcium scoring scan: effect on radiation dose. AJR Am J Roentgenol 2010;194:W272-7. [Crossref] [PubMed]
- Vingiani V, Abadia AF, Schoepf UJ, Fischer AM, Varga-Szemes A, Sahbaee P, Allmendinger T, Tesche C, Griffith LP, Marano R, Martin SS. Low-kV coronary artery calcium scoring with tin filtration using a kV-independent reconstruction algorithm. J Cardiovasc Comput Tomogr 2020;14:246-50. [Crossref] [PubMed]
- Abbara S, Blanke P, Maroules CD, Cheezum M, Choi AD, Han BK, Marwan M, Naoum C, Norgaard BL, Rubinshtein R, Schoenhagen P, Villines T, Leipsic J. SCCT guidelines for the performance and acquisition of coronary computed tomographic angiography: A report of the society of Cardiovascular Computed Tomography Guidelines Committee: Endorsed by the North American Society for Cardiovascular Imaging (NASCI). J Cardiovasc Comput Tomogr 2016;10:435-49. [Crossref] [PubMed]
- Kosmala A, Petritsch B, Weng AM, Bley TA, Gassenmaier T. Radiation dose of coronary CT angiography with a third-generation dual-source CT in a "real-world" patient population. Eur Radiol 2019;29:4341-8. [Crossref] [PubMed]
- Zimmermann E, Dewey M. Whole-heart 320-row computed tomography: reduction of radiation dose via prior coronary calcium scanning. Rofo 2011;183:54-9. [Crossref] [PubMed]
- Hecht HS, de Siqueira ME, Cham M, Yip R, Narula J, Henschke C, Yankelevitz D. Low- vs. standard-dose coronary artery calcium scanning. Eur Heart J Cardiovasc Imaging 2015;16:358-63. [Crossref] [PubMed]



