
Spontaneous renal artery dissection complicated by renal infarction: description of two cases
Introduction
Spontaneous renal artery dissection (SRAD) is a rare clinical event that typically presents with acute low back or flank pain, hypertension, fever, hematuria, and acute renal failure. The condition is often misdiagnosed, or the diagnosis is delayed, due to its relative rarity and nonspecific presentation (1,2). The diagnosis can be made by contrasted-enhanced computed tomography (CT) scans, and if a problem is found, vascular reconstruction is performed, which can display the lesion more clearly. Over 300 cases have been reported since the first characterization (3,4) of SRAD. Although different therapeutic strategies are available for SRAD, a consensus has not yet been reached on the most appropriate treatment. Conservative therapy, open surgery, and intravascular intervention have been reported as treatments for SRAD (5,6). Endovascular stent repair is usually applied when prior medical therapy has been ineffective. There are few reports of endovascular therapy in the literature (6-11). In this report, we describe two SRAD cases complicated by renal infarction which were successfully treated by endovascular stenting using the Abbott Absolute Pro self-expanding nitinol stent system.
Case presentation
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was provided by the patients for publication of these two case reports and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Case 1
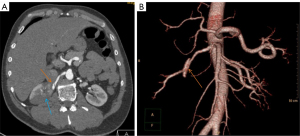
A 44-year-old man presented to the Department of Interventional Radiology, Affiliated Jiangyin Hospital, Medical College of Southeast University with a sudden onset of right flank pain of 17 h’ duration. The physical examination showed a blood pressure of 120/71 mmHg and percussion pain over the right flank. The medical laboratory test results showed a lactate dehydrogenase (LDH) level of 469 U/L, mild leukocytosis (18.41×109/L) with 84.5% neutrophils, and slight renal dysfunction (creatinine 119 µmol/L, urea nitrogen 7.32 mmol/L). However, the C-reactive protein (CRP) level was normal. No hematuria or proteinuria was detected in the spot urine, and urinalysis was negative. He had no past medical history and no urinary symptoms. He had been smoking approximately 10 cigarettes a day for 10 years. His bowel sounds were normal. A B-ultrasound examination showed bilateral small renal stones, and after analgesic treatment, no obvious relief of the lower back pain was achieved. Thus, we began to suspect acute renal colic. Computed tomography angiography (CTA) of the aorta and renal arteries showed dissection at the distal end of the main right renal artery, the formation of a dissecting aneurysm, and occlusion of the posterior branch of the right renal artery, including the branches supplying the lower level of the posterior right kidney (Figure 1).
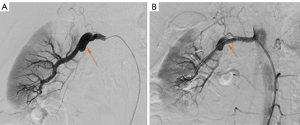
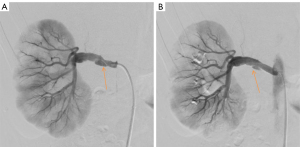
We decided to perform renal artery stenting after obtaining informed consent. The patient was anticoagulated with low-molecular-weight heparin of 6,000 U every 12 h and administered antibiotics (ceftazidime: 2 g every 12 h; levofloxacin: 0.5 g/day) prior to stenting. We decided to use an Absolute Pro vascular self-expanding stent (Abbott Vascular, Santa Clara, CA, USA) considering lesion length, vessel tortuosity, and the great flexibility and adhesion of this stent. Based on previous surgical experience, we performed stent implantation using the femoral artery approach during the procedure. The 6 F introducer sheath was placed using the Seldinger technique. The 6 F long sheath was delivered through the introducer sheath to the aorta at the level of the renal artery ostium, and a Cobra 5 F catheter (Terumo Corporation, Tokyo, Japan) was sent to the opening of the renal artery, at the best working angle. Then, with the guidance of the road map, the Progreat 2.7 F microcatheter and microwire (Terumo) were coaxially fed through the catheter. The microcatheter and microwire were matched to pass through the lesion and into the distal artery trunk and the V-18 hardened exchange guide wire (Boston Scientific Corp., Natick, MA, USA) (12). A 6 mm × 80 mm Absolute Pro Vascular self-expanding stent (Abbott Vascular) was deployed through the guide wire. A digital subtraction angiography (DSA) review showed that the stent was in a good position and the blood flow was unobstructed (Figure 2).
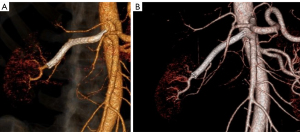
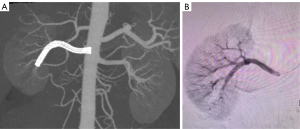
After the procedure, the patient’s right flank pain improved within 1 day. The patient was released from hospital on postoperative day four with anticoagulation and antiplatelet therapy, including low molecular weight heparin 6,000 U every 12 h for 3 days, clopidogrel 75 mg/day, and aspirin 100 mg/day for three months. At discharge, laboratory evaluations revealed that the patient’s blood pressure was 120/70 mmHg, LDH level was 285 U/L, leukocyte count was 5.36×109/L with 64.8% neutrophils, the serum creatinine and urea nitrogen levels were 103 µmol/L and 5.32 mmol/L, respectively. At one month of follow-up, the CTA results showed that the right renal artery stent was unobstructed, the dissecting aneurysm had disappeared, the posterior branch of the right renal artery was recanalized, and the lower level of the right kidney was enhanced. After 10 months, follow-up CTA showed that the lumen of the right renal artery stent was unobstructed and the right kidney was partially atrophied. Moreover, the cortex of the right posterior inferior kidney was thinned and poorly enhanced (Figure 3).
Case 2
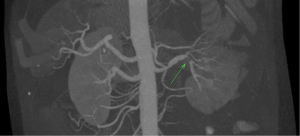
A 44-year-old man developed low back pain without obvious cause 12 h prior to presentation at our hospital with abdominal pain, nausea, and vomiting. The physical examination showed positive percussion pain in the right renal region. Laboratory evaluation revealed a blood pressure of 130/70 mmHg, an LDH level of 1,060 U/L, mild leukocytosis (11.29×109/L) with 88.3% neutrophils, slight renal dysfunction (creatinine 121 µmol/L, urea nitrogen 7.0 mmol/L), and a CRP level of 134 mg/L. Routine testing revealed that urine, coagulation function, procalcitonin, autoantibodies, and other indicators were all normal. The patient had neither past medical history and urinary symptoms nor a history of vascular intervention and recent trauma. However, he did have a history of smoking. Emergency CTA revealed right renal artery dissection with thrombosis and partial right kidney infarction (Figure 4).
After obtaining the informed consent of the patient and his family, we decided to perform renal artery stenting after thrombolysis. The patient underwent thrombolysis with urokinase 300,000 µ every 12 h, and he was anticoagulated with low molecular weight heparin 8,000 U every 12 h and administered antibiotics (ceftazidime: 2 g every 12 h; levofloxacin: 0.5 g/day) prior to stenting. Given its many advantages (i.e., the ability to reduce complications and better flexibility and bending resistance), we decided to continue using the Absolute Pro vascular self-expanding stent (Abbott Vascular) (13). The same steps were performed to finally deploy the stent. A 6 mm × 80 mm bare stent was deployed through a 6 F long sheath using a 5 F catheter. A DSA review showed that the stent was placed in a good position and blood flow was unobstructed (Figure 5).
The patient’s low back pain improved within half a day after surgery. The patient was released from hospital on postoperative day four with anticoagulation and antiplatelet therapy: low molecular weight heparin 6,000 U every 12 h for three days, clopidogrel 75 mg/day, and aspirin 100 mg/day for three months. At discharge, laboratory evaluations revealed the patient’s LDH level was 396 U/L, leukocyte count was 6.09×109/L with 64.9% neutrophils, and serum creatinine and urea nitrogen levels were 110 µmol/L and 5.14 mmol/L, respectively. After 1 month, follow-up CTA showed no deterioration of renal infarction of the right kidney, the stent was unobstructed, the inner membrane sheet was completely fitted by the stent, and the DSA showed no sign of residual dissection and confirmed the disappearance of the false lumen (Figure 6). It was suggested that the patient take the medication continuously and return to the clinic every six months for CTA.
Discussion
The incidence of SRAD accounts for only 1–2% of all arterial dissections, and bilateral involvement occurs in approximately 10–15% of patients (14-16). In a normal healthy individual with no predisposing factors, SRAD is an even rarer phenomenon. Both of the cases we have reported were male patients; SRAD occurs mostly in men between the ages of 40 and 60. The male: female ratio is reported to be in the range of 4:1 to 10:1 (5). The etiology of SRAD is still unclear. Adverse development of the media and alterations of the vasa vasorum, severe atherosclerosis, and blood flow shear stress may be pathogeny. Malignant hypertension, fibromuscular dysplasia (15), strenuous exercise (including sexual) (17), taking medication (18,19), Marfan syndrome (20), and Ehlers-Danlos syndromes (4) are all possible risk factors. In our two case studies, we found that both of the patients had a long history of smoking, which was similar to the reports by other researchers (6,11,21). Therefore, we believe that smoking may be another risk factor for SRAD. However, many cases occur in otherwise healthy individuals (22,23). Furthermore, the nonspecific presentation frequently results in a diagnostic delay. At the same time, the renal artery is located deep in the abdomen, it is relatively slender, and there are many abdominal organs and intestines around it. For patients with obesity or intestinal gas interference, the main renal artery may not be displayed clearly on imaging, and the relatively high requirements for Doppler ultrasound (DUS) instruments make imaging difficult. It is difficult to identify the early stage of SRAD using DUS, with poor sensitivity and low diagnostic rate (24,25). However, when there is a significant renal infarction in the late stage of SRAD, DUS can detect poor renal perfusion, thereby assisting in the diagnosis. A definitive diagnosis requires angiography studies which are able to precisely explain the degree and feature of vascular involvement while identifying potential treatment options. With the progress of science and technology, CTA has replaced conventional angiography owing to its noninvasiveness and accuracy. In these reports, we were without doubt regarding the diagnosis and subsequent follow up of SRAD using CTA. Since the accuracy of CTA is improving, conventional arteriography may be gradually replaced by novel technologies.
The optimal therapeutic approach for SRAD remains unclear. Overall, the treatment of SRAD is divided into two strategies. One is conservative treatment that is often a combination of antihypertensive drugs and systemic anticoagulation. Patients who show neither uncontrollable high blood pressure nor a worsening of serum creatinine levels are frequently treated conservatively. In some cases of conservative treatment, patients have received anticoagulant therapy for a short or long period to avoid thromboembolic events. However, no clinical studies have ever compared anticoagulation therapy with no anticoagulation therapy. Whether thrombolytic therapy should be provided is still controversial. Although thrombolytic therapy can reconstruct the blood flow of true lumen, it will also increase the pressure of false lumen, thereby expanding the dissection and aggravating damage to the intima. In severe cases, it may even lead to deterioration of the dissection and consequences of renal atrophy. When the patient’s drug treatment is ineffective, another method is needed, such as revascularization.
Revascularization includes surgical and endovascular treatment. Some relevant reports have suggested that the surgical effect is poor and can result in acute thrombosis of the renal artery and late anastomotic restenosis (11,15,26,27). Fortunately, owing to the advantages of avoiding clamping and allowing for rapid revascularization, endovascular treatment is emerging as a less aggressive treatment alternative, and, endovascular intervention tends to be the preferred therapeutic method with safer and more effective outcomes (6,11). The indications for vascular intervention are lesions located in the main renal artery with an enlarged false lumen of dissection, uncontrolled hypertension, and deterioration of renal function. Endovascular intervention includes placement of self-expanding stents or stents with coiling and thrombolysis followed by stenting. We chose the Absolute Pro vascular self-expanding stent because it has a thin wall, delivers little stimulation to the intima, and has good flexibility and adherence. Even if the blood vessel were to become twisted, in more severe cases it could completely cover the lesion. These superior features of the stent may significantly reduce the complications associated with arterial puncture points. In both of our cases, the patients’ severe symptoms of pain disappeared after successful revascularization with stent placement, and follow-up CTA in both patients showed that the renal artery stent was unobstructed and renal function was normal.
In conclusion, SRAD is a rare clinical event, and diagnosis is often delayed due to its indistinct and nonspecific clinical symptoms. The accuracy of CTA in diagnosing SRAD has gradually improved, making it the potential replacement for DSA in diagnosis. From the examples reported in this paper, it can be concluded that self-expanding stent implantation for SRAD is associated with favorable clinical results. Hence, the endovascular treatment of SRAD seems to be a safe and effective option that should be considered in the case of bad clinical or radiologic evolution of SRAD.
Acknowledgments
Funding: This study was supported by the general project of Jiangyin Health Committee (No. S202104).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-22-342/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was provided by the patients for publication of these two case reports and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Mansoor MS, Shafiq M. Spontaneous renal artery dissection: current perspective. J Pak Med Assoc 2012;62:1333-7. [PubMed]
- Guérin E, Vandueren E, Dubois E, et al. Spontaneous renal artery dissection in an otherwise healthy male. Acta Chir Belg 2006;106:703-6. [Crossref] [PubMed]
- Bumpus HC. A case of renal hypertension. J Urol 1944;52:295-9. [Crossref]
- Ramamoorthy SL, Vasquez JC, Taft PM, et al. Nonoperative management of acute spontaneous renal artery dissection. Ann Vasc Surg 2002;16:157-62. [Crossref] [PubMed]
- Edwards BS, Stanson AW, Holley KE, et al. Isolated renal artery dissection, presentation, evaluation, management, and pathology. Mayo Clin Proc 1982;57:564-71. [PubMed]
- Jiang J, Li L, Liu Y, et al. Endovascular treatment of spontaneous renal artery dissection. J Vasc Surg 2019;70:1889-95. [Crossref] [PubMed]
- Aoki Y, Sakai Y, Kimura T, et al. Renal Artery Stenting Recovered Renal Function after Spontaneous Renal Artery Dissection. Intern Med 2019;58:2191-4. [Crossref] [PubMed]
- Peynircioğlu B, Pişkinkaya S, Özer Ç, et al. Isolated spontaneous renal artery dissection: diagnosis and endovascular management. Diagn Interv Radiol 2011;17:101-4. [PubMed]
- Vitiello GA, Blumberg SN, Sadek M. Endovascular Treatment of Spontaneous Renal Artery Dissection After Failure of Medical Management. Vasc Endovascular Surg 2017;51:509-12. [Crossref] [PubMed]
- García-Familiar A, Ortiz-Gutiérrez F, De Blas-Bravo M, et al. Isolated spontaneous renal artery dissection: endovascular management. Ann Vasc Surg 2014;28:1034.e5-8. [Crossref] [PubMed]
- Pellerin O, Garçon P, Beyssen B, et al. Spontaneous renal artery dissection: long-term outcomes after endovascular stent placement. J Vasc Interv Radiol 2009;20:1024-30. [Crossref] [PubMed]
- Gao F, Huang X, Ren D, et al. Results Obtained with the Protege EverFlex Self-expanding Bare Stent in Interventional Treatment of Spontaneous Isolated Visceral Artery Dissection. Ann Vasc Surg 2021;77:86-93. [Crossref] [PubMed]
- Maleckis K, Deegan P, Poulson W, et al. Comparison of femoropopliteal artery stents under axial and radial compression, axial tension, bending, and torsion deformations. J Mech Behav Biomed Mater 2017;75:160-8. [Crossref] [PubMed]
- Mudrick D, Arepally A, Geschwind JF, et al. Spontaneous renal artery dissection: treatment with coil embolization. J Vasc Interv Radiol 2003;14:497-500. [Crossref] [PubMed]
- Lacombe M. Isolated spontaneous dissection of the renal artery. J Vasc Surg 2001;33:385-91. [Crossref] [PubMed]
- Mori H, Hayashi K, Tasaki T, et al. Spontaneous resolution of bilateral renal artery dissection: a case report. J Urol 1986;135:114-6. [Crossref] [PubMed]
- Elhassan M, Husnain S, Mian R. Spontaneous renal artery dissection associated with sexual intercourse: a case report. Int Med Case Rep J 2018;11:221-3. [Crossref] [PubMed]
- Regmi MR, Carbrey SA, Parajuli P, et al. A Rare Case of Isolated and Idiopathic Spontaneous Renal Artery Dissection in a Female Patient on Multiple Medications. Cureus 2019;11:e5770. [Crossref] [PubMed]
- Lou JY, Randhawa MS, Hornacek D, et al. Images in vascular medicine. Spontaneous renal artery dissection in a cannabis user. Vasc Med 2015;20:379-80. [Crossref] [PubMed]
- Slavis SA, Hodge EE, Novick AC, et al. Surgical treatment for isolated dissection of the renal artery. J Urol 1990;144:233-7. [Crossref] [PubMed]
- Afshinnia F, Sundaram B, Rao P, et al. Evaluation of characteristics, associations and clinical course of isolated spontaneous renal artery dissection. Nephrol Dial Transplant 2013;28:2089-98. [Crossref] [PubMed]
- Boughey JC, Gifford RR, Collins JB, et al. Spontaneous renal artery dissection in a healthy man. J S C Med Assoc 2001;97:246-9. [PubMed]
- Alamir A, Middendorf DF, Baker P, et al. Renal artery dissection causing renal infarction in otherwise healthy men. Am J Kidney Dis 1997;30:851-5. [Crossref] [PubMed]
- Renaud S, Leray-Moraguès H, Chenine L, et al. Spontaneous renal artery dissection with renal infarction. Clin Kidney J 2012;5:261-4. [Crossref] [PubMed]
- Gandhi SP, Patel K, Pal BC. Isolated Spontaneous Renal Artery Dissection Presented with Flank Pain. Case Rep Radiol 2015;2015:896706. [Crossref] [PubMed]
- Müller BT, Reiher L, Pfeiffer T, et al. Surgical treatment of renal artery dissection in 25 patients: indications and results. J Vasc Surg 2003;37:761-8. [Crossref] [PubMed]
- van Rooden CJ, van Baalen JM, van Bockel JH. Spontaneous dissection of renal artery: long-term results of extracorporeal reconstruction and autotransplantation1. J Vasc Surg 2003;38:116-22. [Crossref] [PubMed]


