
Application of transvaginal two-dimensional fundamental sonosalpingography in infertile women with tubo-ovarian cyst
We have great interest in the clinical value of transvaginal two-dimensional fundamental sonosalpingography (2D-FS). Recently, we published an original article entitled “The performance of transvaginal two-dimensional fundamental sonosalpingography combined with saline infusion pelvic sonosalpingography for assessing fimbrial part’s morphology and function of the fallopian tubes” (1). Herein, we would like to further share our experience of the application of 2D-FS in the diagnosis of tubo-ovarian cyst (TOC) in a 32-year-old infertile woman who underwent hysterosalpingo-contrast sonography (HyCoSy) for bilateral hydrosalpinx as indicated by transvaginal sonography (TVS). To the best of our knowledge, no similar studies have been previously reported. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was provided by the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
TOC is not an uncommon type of pelvic inflammatory disease (PID) that occurs predominantly in sexually active women of reproductive age. It is most commonly caused by tubal inflammation involving the ovary, which may result in adhesion between the fimbrial part of the fallopian tube and the ipsilateral ovary, leading to the formation of an inflammatory mass (2,3). For women preparing for pregnancy, TOC prevents the fimbriae from picking up eggs, which serves a critical role in fertilization. In addition, regurgitation of the inflammatory fluid retained in the cyst into the uterine cavity can damage the embryo and the endometrium, which may reduce the embryo implantation rate or increase the risk of early abortion (4). Furthermore, gradual ovarian shrinkage and functional decline are likely to occur with expansion of the TOC. Therefore, early diagnosis is essential for selecting an appropriate treatment strategy. However, the vague and unspecific symptoms of TOC present a diagnostic dilemma that hinders correct and timely diagnosis. Currently, preoperative diagnosis of TOC predominantly relies on various imaging techniques, such as computed tomography (CT), magnetic resonance (MR), and TVS (2,3). As a cost-effective, time-saving, nonradiating, and noninvasive procedure, TVS has become the first-line imaging modality in the evaluation of PID (5). Nonetheless, it is challenging to make a diagnosis of TOC via TVS (Figure 1A,1B), as its imaging manifestations are almost always atypical and may mimic some other pelvic processes (2). We interpreted the underlying reasons why TVS fails to diagnose TOC as follows: (I) the opening between the fimbriae and the ipsilateral ovary may be concealed in a significantly distended fallopian tube with multiple intermittent segments folded together; (II) adhesion among the internal genital organs and the pelvic wall lead to the displacement of local anatomical structures; and (III) lack of experience of the sonographer. Overall, the diagnostic difficulty of TOC is mainly related to the obscure anatomical relationship between the fimbrial part of the fallopian tube and the ipsilateral ovary.
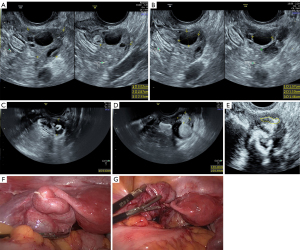
It has been shown that HyCoSy is an important imaging technique for evaluating fallopian tubal patency with an evidence level of 2B (6). The 2D-FS is a contrast mode of HyCosy that provides some advantages in ascertaining the relationship between the fimbrial part of the fallopian tube and the ipsilateral ovary. We summarize the reasons for this as follows (1,7): (I) the acoustic energy output when operated at a high mechanical index allows the trajectory of the microbubble signals and the surrounding anatomical structures to be tracked simultaneously; and (II) as imaging is not limited by the sampling frame, the acquisition of distal information can be ensured to a large extent. In this case, during the process of 2D-FS, we tracked the location of the contrast agent in real time and captured the moment that the dilated distal part of the left fallopian tube became ensconced in the ipsilateral ovary in a cystic form. Subsequently, a small amount of contrast agent diffusing into the ovarian parenchyma was observed, indicating that there was at least 1 leak at the weak part of the fimbrial part of the fallopian tube. These 2 signs were thus named “distal part of fallopian tube buried in the ipsilateral ovary” and “contrast agent diffusion into ovarian parenchyma”, respectively (Figure 1C-1E). Both were verified by laparoscopy and dye test (LDT) as characteristic and specific imaging features for the diagnosis of TOC (Figure 1F,1G). It should be noted that the latter sign was not indispensable for the diagnosis of TOC. Although the presence of this sign strongly favors TOC, the absence of this sign does not necessarily exclude the possibility of TOC since the fimbrial part might instead be an actual cul-de-sac.
In conclusion, the possibility of TOC should be considered in an infertile woman with hydrosalpinx detected by TVS. A HyCoSy, especially 2D-FS, is recommended for further workup for patients suspected of TOC. Identifying the “distal part of fallopian tube buried in ipsilateral ovary” sign and the “contrast agent diffusion into ovarian parenchyma” sign could be very helpful for establishing a definitive diagnosis. However, a larger sample size is recommended to further validate the application of 2D-FS in daily practice in patients with suspected TOC.
Acknowledgments
Funding: This study was supported by the Medical and Health Technology Project in Zhejiang Province of China (No. 2020KY430), the Excellent Scientific Research Foundation of Zhejiang Provincial People’s Hospital (No. ZRY2021B012), and the Excellent Scientific Research Foundation of Zhejiang Provincial People’s Hospital (No. ZRY2020B016).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-22-5/coif). All authors report that this study was supported by the Medical and Health Technology Project in Zhejiang Province of China (No. 2020KY430), the Excellent Scientific Research Foundation of Zhejiang Provincial People’s Hospital (No. ZRY2021B012), and the Excellent Scientific Research Foundation of Zhejiang Provincial People’s Hospital (No. ZRY2020B016). The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was provided by the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Xu Z, Peng C, Lv Y, et al. The Performance of Transvaginal Two-Dimensional Fundamental Sonosalpingography Combined with Saline Infusion Pelvic Sonosalpingography for Assessing Fimbrial Part's Morphology and Function of the Fallopian Tubes. J Ultrasound Med 2022;41:41-50. [Crossref] [PubMed]
- Revzin MV, Mathur M, Dave HB, et al. Pelvic Inflammatory Disease: Multimodality Imaging Approach with Clinical-Pathologic Correlation. Radiographics 2016;36:1579-96. [Crossref] [PubMed]
- Huang BT, Han SZ, Cai DN, et al. Clinical pathological features and MRI analysis of tubo-ovarian cyst: 16 cases. Journal of Guangdong Medical University 2018;36:584-7.
- Campbell S. Ultrasound Evaluation in Female Infertility: Part 2, the Uterus and Implantation of the Embryo. Obstet Gynecol Clin North Am 2019;46:697-713. [Crossref] [PubMed]
- Wall DJ, Javitt MC, Glanc P, et al. ACR appropriateness Criteria® infertility. Ultrasound Q 2015;31:37-44. [Crossref] [PubMed]
- Lin X, Huang G, Sun H, et al. Chinese expert consensus on diagnosis and treatment of tubal infertility. J Reprod Med 2018;27:1048-56.
- Chen F, Chen W, Wei F, et al. Diagnosis of fallopian tube patency by combination of four-dimensional and two-dimensional transvaginal hysterosalpingo-contrast sonography. Chin J Ultrasonogr 2015;24:869-73.


