
Styloidogenic jugular venous compression syndrome as a source of cerebral venous sinus thrombosis
Introduction
Eagle syndrome is a rare condition associated abnormal styloid process which presents pain in the anterolateral neck. Incidences of abnormal stylohyoid length range from 4% to 7.3%. Abnormally elongated styloid process compress surrounding vascular and nerve structures including facial nerve, auriculo-temporal nerve, lingual nerve, chorda tympani, glossopharyngeal nerve, and hypoglossal nerve in classic subtype, and internal and external carotid arteries in carotid subtype. Although styloidogenic jugular venous compression syndrome (SJVCS) does not fit into two subtypes, it caused by an elongated styloid process compressing the internal jugular vein (IJV) (1,2). Here, we report a case of cerebral venous sinus thrombosis (CVST) in a patient with SJVCS caused by an elongated styloid process compressing the IJV.
Case presentation
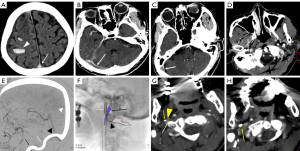
An 84-year-old male patient was admitted with sudden onset motor weakness of the right limb and facial muscles, asomatognosia, and dysarthria. He suffered from headache for 2 months and was treated unsuccessfully with acetaminophen. Papilledema which is sign of increased intracranial pressure and transient blurred vision in both eyes were found on neurological examination, and his score on the National Institutes of Health Stroke Scale was 6. He had no history of malignancy, infection, surgery, or head trauma. Electrocardiography revealed a sinus rhythm. Initial blood test results (including markers for infection, inflammation, coagulopathy, and cancer) were within the reference ranges. Initial blood test results (including markers for infection, inflammation, coagulopathy, and cancer) were within the reference ranges. Computed tomography (CT) revealed a cortical hemorrhage with perilesional edema and occlusion in the superior sagittal sinus, right transverse sinus, sigmoid sinus, and upper IJV, suggesting potential CVST (Figure 1A-1D). Subsequent digital subtraction angiography confirmed occlusion in the superior sagittal sinus, right transverse sinus, sigmoid sinus, and upper IJV, confirming CVST diagnosis (Figure 1E). Because extensive CVST, sign of increased intracranial pressure, and cortical hemorrhage were observed, we decided to apply interventional treatment for the patient. Aspiration thrombectomy with systemic anticoagulation was conducted using an aspiration catheter. However, the aspiration catheter with a 0.035-inch guidewire (Terumo, Tokyo, Japan) failed to pass through the occluded vessel, and only a small thrombus was pulled by aspiration (Figure 1F). Axial CT venography (CTV) revealed that the right IJVs were compressed between the transverse process of C1 and the elongated styloid process [31.4 mm (normal, <25 mm)], suggestive of the SJVCS subtype of Eagle’s syndrome (Figure 1G). Moreover, a low density in the upper IJV just above the tip of elongated styloid process was identified as a thrombus (Figure 1H). Ultrasonography of the lower extremity veins showed no other evidence of venous thromboembolism. Although we recommended surgery for the removal of the styloid process, consent was not provided. Oral anticoagulation therapy including warfarin was initiated instead and maintained for four weeks. Neurological deterioration was not observed and papilledema and headache were improved during the following four weeks, and therefore, the patient was discharged. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Eagle’s syndrome refers to the compression of vascular and nerve structures caused by an elongated styloid process. In SJVCS, a subtype of Eagle’s syndrome, the IJV is compressed by the elongated styloid process and the transverse process of C1 (3). Although several structures may cause extrinsic compression of the IJV, including arteries and the digastric and sternocleidomastoid muscles, an elongated styloid process is more common (4). The normal length of the styloid process is approximately 25 mm, and it is considered to be elongated when it reaches more than 30 mm. Although 4% of patients with an elongated styloid process display symptom, intracranial hypertension caused by an elongated styloid process compressing the IJV is very rare (5). The upper IJV is more frequently compressed and the left side is more commonly affected (6). The anatomical relationship between the IJV and elongated styloid process is easily visualized by CTV. Although treatment varies according to the occurrence of intracranial hypertension, good outcomes have been reported from venous stenting and removal of the styloid process. Nevertheless, no standard guidelines exist for the treatment of SJVCS with CVST.
Herein, we present a case of SJVCS and CVST associated with intracerebral hemorrhage and treated with aspiration thrombectomy and long-term anticoagulation therapy. Unusually, the patient was an elderly male with the right IJV affected. Because initially we did not know the cause of CVST, we performed aspiration thrombectomy with systemic anticoagulation. However, since the aspiration catheter and 0.035-inch guidewire failed to pass through the compressed IJV, contact aspiration thrombectomy could not be performed, and distant aspiration, which is less effective, removed only a small thrombus. The diameter of the IJV was estimated to be less than 0.035 inch (0.89 mm). IJV compression by the elongated styloid process was well visualized by CTV. Previous review showed that contact aspiration thrombectomy was salvage therapy for refractory CVST (7). In our case, distant aspiration thrombectomy and long-term anticoagulation therapy is an effective and feasible therapy for patients with SJVCS and CVST, who refuse surgery for the removal of the styloid process
In conclusion, an elongated styloid process was the cause for SJVCS with CVST. CTV may be a useful tool for the detection of thrombi within the IJV and an elongated styloid process and may thus aid in the accurate diagnosis of the syndrome.
Acknowledgments
Funding: This research was supported by a grant from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by The Ministry of Health & Welfare, Republic of Korea (grant number: HI20C1405) and the National Research Foundation of Korea (NRF) grant funded by the Government of South Korea (Ministry of Science of ICH, MSIT) (No. NRF-2020-R1C1C1006623).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-22-106/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Badhey A, Jategaonkar A, Anglin Kovacs AJ, et al. Eagle syndrome: A comprehensive review. Clin Neurol Neurosurg 2017;159:34-8. [Crossref] [PubMed]
- Aldakkan A, Dunn M, Warsi NM, et al. Vascular Eagle's Syndrome: Two Cases Illustrating Distinct Mechanisms of Cerebral Ischemia. J Radiol Case Rep 2017;11:1-7. [PubMed]
- Dashti SR, Nakaji P, Hu YC, et al. Styloidogenic jugular venous compression syndrome: diagnosis and treatment: case report. Neurosurgery 2012;70:E795-9. [Crossref] [PubMed]
- Jayaraman MV, Boxerman JL, Davis LM, et al. Incidence of extrinsic compression of the internal jugular vein in unselected patients undergoing CT angiography. AJNR Am J Neuroradiol 2012;33:1247-50. [Crossref] [PubMed]
- Prasad KC, Kamath MP, Reddy KJ, et al. Elongated styloid process (Eagle's syndrome): a clinical study. J Oral Maxillofac Surg 2002;60:171-5. [Crossref] [PubMed]
- Mooney J, Lepard J, Akbari SHA, et al. Styloidogenic jugular venous compression syndrome: a case report and review of the literature. Childs Nerv Syst 2020;36:3135-9. [Crossref] [PubMed]
- Ilyas A, Chen CJ, Raper DM, et al. Endovascular mechanical thrombectomy for cerebral venous sinus thrombosis: a systematic review. J Neurointerv Surg 2017;9:1086-92. [Crossref] [PubMed]


