
Effect of cervical alignment change after anterior cervical fusion on radiological adjacent segment pathology
Introduction
Timely surgery can effectively improve the clinical symptoms and prognosis of patients with cervical spondylotic myelopathy (CSM). The clinical efficacy of anterior cervical fusion (ACF) in the treatment of CSM has been repeatedly demonstrated (1-3), and corpectomy and discectomy are the most common surgical approaches. With continuous improvements in modern medical technology, the long-term efficacy of ACF for the treatment of CSM has attracted increasing attention. Adjacent segment pathology (ASP) is one of the primary complications that affects the long-term efficacy of cervical fusion, and it can be classified as radiographic ASP (RASP) or clinical ASP (CASP) according to the absence or presence of clinical symptoms. The 10-year incidence of CASP is about 25% (4), while for RASP it can be much higher (5-7), and CASP tends to be found more often in patients with RASP. At present, the causes and mechanisms of adjacent segmental lesions are still unclear.
Good cervical fusion after surgery is the key factor in maintaining the physiological structure and function of the cervical spine. The healing process is influenced by physiological gravity and often results in embedding of the implant into the adjacent vertebral body. Therefore, there may be changes in the structure and curvature of the cervical spine after surgery. However, the effects of such changes on cervical curvature and long-term clinical outcomes after ACF remain controversial (8-11).
We present the following article in accordance with the STROBE reporting checklist (available at https://qims.amegroups.com/article/view/10.21037/qims-21-732/rc).
Objectives
To further clarify the incidence of adjacent segmental pathology after ACF, we investigated the influence of the height of the surgical segment or the curvature of the cervical spine on RASP development, and the correlation between RASP and postoperative clinical recovery.
Methods
Patients
A retrospective analysis was performed on 88 patients with CSM who underwent ACF surgery in the Department of Orthopedics and Spine Surgery at the Third Xiangya Hospital of Central South University between 1 January 2008 and 31 December 2013. Written or oral consent was provided by all patients in this study. The study was approved by the Ethics Committee of the Third Xiangya Hospital of Central South University, and was conducted in accordance with the Declaration of Helsinki (revised in 2013). The inclusion criteria were as follows: patients who underwent ACF for cervical spondylosis with a minimum follow-up period of 1 year, with complete imaging and clinical data available. The exclusion criteria were as follows: (I) patients who had already undergone cervical surgery, or underwent ACF combined with posterior cervical surgery; (II) patients with other cervical non-degenerative diseases including fractures, active infections or inflammation, diseases of the connective tissues, tumors, or congenital dysplasia. There were 42 males and 46 females included in the study with an average age of 50.9 years (SD: 8.7 years, range, 29 to 75 years). Cervical surgery in all patients was performed in the Third Xiangya Hospital of Central South University. The procedures were partial vertebral body resection and titanium cage autologous bone implantation and plate fixation of the anterior cervical spine. The mean follow-up period was 29.1 months (SD: 17.5 months, range, 12 to 88 months).
Imaging analysis
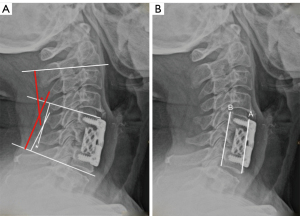
All cases had a radiological examination of the cervical spine preoperatively, postoperatively (2–4 weeks after surgery), and at a final follow-up (at least 1 year after surgery). The imaging data of all cases were analyzed at the Picture Archiving and Communication System (PACS) workstation of the Radiology Department of the Third Xiangya Hospital, Central South University. The imaging examination data included frontal and neutral lateral radiographs of the cervical spine. Preoperative and follow-up magnetic resonance imaging (MRI) and/or computed tomography (CT) images of the cervical spine were also obtained. If a patient exhibited a new or aggravated degenerative change in the adjacent segment, such as narrowing of the intervertebral space, enlargement of the osteophytes in the vertebral body, endplate sclerosis, uncinate hyperplasia, facet joint degeneration, and so on, RASP was diagnosed (12). The C2-7 Cobb angle, the Cobb angle of the operated segments, and the anterior and posterior height of the fused segments (AFH and PFH, respectively) were measured on the neutral lateral radiographs of the cervical spine before surgery, and again after surgery at the short-term and final follow-ups for each patient (Figure 1). The images were evaluated twice within 1 month by 2 senior imaging diagnostic radiologists who were blind to the clinical outcome, and the average was taken for data analysis. The diagnosis of RASP for each patient was made based on the agreement of both radiologists.
Preoperative and postoperative clinical evaluation
Demographic, clinical, and surgical information were obtained for each patient. The severity of the cervical spondylosis symptoms was evaluated by Japanese Orthopedic Association (JOA) score before surgery (preoperative JOA score), after surgery (postoperative JOA score), and at the final follow-up. The surgical outcome was measured by the recovery rate (RR), which was calculated using the JOA scores before and after surgery (within 1 month). The specific formula used is as follows, where normal score =17 (13):
Statistical analysis
All statistical analyses were performed using the software SPSS 18.0 (IBM Corp., Armonk, NY, USA). To compare the clinical and imaging characteristics of the 2 groups of cases, continuous variables were analyzed using a paired t-test or Mann-Whitney U test. The categorical variables were analyzed using the Fisher’s or chi-squared test, when appropriate. Single factor correlation was analyzed using Pearson correlation analysis. The factors with P<0.05 were further analyzed using Cox regression to determine the predictive value of RASP. Values of P<0.05 were considered statistically significant.
Results
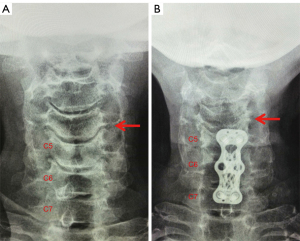
Except for the follow-up period and the clinical features of the patients, such as surgical site, number of fused segments, and JOA scores for preoperative, postoperative, and final follow-up, no significant differences were observed between the RASP and non-RASP groups (Table 1). The JOA scores in the short-term after surgery for all cases were significantly higher than those before surgery. The JOA score at the final follow-up for the RASP group was significantly lower than at the short-term follow-up, but the JOA score of the non-RASP group was significantly higher at the final follow-up than at the short-term follow-up. A typical RASP case exhibiting new development of neck pain and recurrence of symptoms is shown in Figure 2.
Table 1
| RASP group (N=42) | No-RASP group (N=46) | P value | |
|---|---|---|---|
| Age†, years | 50.4 (11.4) | 51.3 (8.5) | 0.6 |
| Gender (male) | 22 | 20 | 1 |
| Diagnosis | |||
| Radiculopathy | 2 | 4 | 0.67 |
| Myelopathy/mixed | 40 | 42 | |
| Fused segment | |||
| 1 segment | 6 | 6 | 0.26 |
| 2 segments | 31 | 33 | 1 |
| 3 segments | 5 | 7 | 0.26 |
| Surgical approach | 1 | ||
| Corpectomy | 36 | 39 | |
| Discectomy | 6 | 7 | |
| Graft type | 0.63 | ||
| Autologous bone only | 5 | 2 | |
| Ti-cage (± autologous bone) | 37 | 44 | |
| Follow up (month)† | 36.3 (20.9) | 22.5 (12.5) | <0.01 |
| Pre-operative JOA | 10.48±2.79 | 10.78±2.85 | 0.82 |
| Post-operative JOA | 13.71±2.24* | 14.42±2.44* | 0.91 |
| Follow-up JOA | 13.69±2.20** | 14.60±2.58** | 0.23 |
| Post-operative RR | 59.20±29.68 | 62.34±24.48 | 0.59 |
| Follow-up RR | 48.72±38.01§ | 65.63±27.62 | 0.01 |
†, average (standard deviation); *, comparing to pre-operative JOA, P<0.05; **, comparing to post-operative JOA, P<0.05; §, comparing to post-operative RR, P<0.05. RASP, radiological adjacent segment pathology; N, number; JOA, Japanese orthopaedic association; RR, recovery rate.
The anterior and posterior heights of the fused segments (AFH, PFH), together with the C2-7 Cobb angle (C27CA) and the Cobb angle of the fused segments (FCA) at 3 time points before and after surgery, are presented in Table 2. Compared with preoperative data, AFH and PFH for the 2 groups were significantly increased after surgery; however, they were significantly lower at the final follow-up than those at the short-term postoperative follow up. In the RASP group, the C2-7 Cobb angle was significantly lower at both the short-term and final follow-up compared to that before surgery, despite the C2-7 Cobb angle increased during follow-up. In the non-RASP group, both the C2-7 Cobb angle and the Cobb angle of the fusion segments in the short-term and final follow-up were both significantly higher than before surgery. When compared to the non-RASP group, significantly more patients in the RASP group demonstrated a decrease in postoperative lordosis (34 in the RASP group and 18 in the non RASP group, P<0.001).
Table 2
| Parameters | RASP group | Non-RASP group | P value | |
|---|---|---|---|---|
| Pre-operative | AFH, cm | 5.22±1.23 | 5.27±1.15 | 0.86 |
| PFH, cm | 5.12±1.12 | 5.14±1.06 | 0.91 | |
| C27CA, ° | 20.42±9.92 | 12.65±11.91 | <0.01 | |
| FCA, ° | 6.76±7.16 | 4.97±8.37 | 0.29 | |
| Post-operative | AFH, cm | 5.55±1.20** | 5.86±1.47** | 0.29 |
| PFH, cm | 5.38±1.20** | 5.63±1.40** | 0.37 | |
| C27CA, ° | 13.81±8.52** | 15.35±10.05* | 0.45 | |
| FCA, ° | 7.12±5.47 | 9.06±6.92** | 0.15 | |
| Follow-up | AFH, cm | 5.19±1.09§§ | 5.39±1.17**,§§ | 0.42 |
| PFH, cm | 5.05±1.05§§ | 5.14±1.06§§ | 0.67 | |
| C27CA, ° | 17.02±9.67*,§§ | 19.43±9.63**,§§ | 0.25 | |
| FCA, ° | 6.38±6.26 | 9.45±7.52** | 0.04 |
*, comparing to pre-operative, P<0.05; **, comparing to pre-operative, P<0.01; §§, comparing to post-operative, P<0.01. RASP, radiological adjacent segment pathology; AFH, anterior height of fused segments; PFH, posterior height of fused segments; C27CA, C2-7 Cobb angle; FCA, fused segment Cobb angle.
Correlations between the imaging parameters and the occurrence of RASP were analyzed and the results are presented in Table 3. When comparing the short-term postoperative data to the preoperative data, a change in AFH was significantly correlated with a change in the following: PFH (correlation coefficient 0.599, P<0.001), C2-7 Cobb angle (correlation coefficient 0.274, P=0.010), and the Cobb angle of the fused segments (correlation coefficient 0.333, P=0.002). After regression analysis, the short-term postoperative C2-7 Cobb angle and the Cobb angle of the fused segments were both related to RASP (Table 4). After adjusting for each patient’s age, gender, surgical site, and surgical segment, Cox regression analysis was performed, showing that only a short-term postoperative change in the C2-7 Cobb angle was significantly correlated with the occurrence of RASP and had predictive value, with a hazard ratio (HR) of 0.336 (Table 5).
Table 3
| RASP | RR1 | RR2 | AFH-C | PFH-C | C27CA-C | FCA-C | |
|---|---|---|---|---|---|---|---|
| RASP | 0.032 (0.772) | –0.118 (0.277) | –0.101 (0.354) | –0.040 (0.712) | –0.507* (0.000)* | –0.342* (0.001)* | |
| RR1 | 0.925 (0.000) | 0.166 (0.128) | 0.224* (0.038)* | 0.160 (0.139) | 0.191 (0.076) | ||
| RR2 | 0.141 (0.194) | 0.220* (0.042)* | 0.194 (0.072) | 0.226 (0.035) | |||
| AFH-C | 0.599* (0.000)* | 0.274* (0.010)* | 0.333* (0.002)* | ||||
| PFH-C | –0.024 (0.826) | 0.039 (0.719) | |||||
| C27CA-C | 0.785* (0.000)* |
Data was shown as r (P). *, P<0.05. RASP, radiological adjacent segment pathology; RR1, recovery rate at short term follow-up; RR2, recovery rate at final follow-up; AFH-C, change of post-operative anterior height of fused segments comparing to preoperative; PFH-C, change of post-operative posterior height of fused segments comparing to preoperative; C27CA-C, change of post-operative C2-7 Cobb angle comparing to preoperative; FCA-C, change of post-operative fused segment Cobb angle comparing to preoperative.
Table 4
| Parameters | OR (95% CI) | SE | Wald (χ2) | P value |
|---|---|---|---|---|
| AFH-C | 0.602 (–0.763, 1.967) | 0.696 | 0.748 | 0.387 |
| PFH-C | 0.098 (–1.111, 1.307) | 0.617 | 0.025 | 0.873 |
| C27CA-C | 1.960 (0.889, 3.031) | 0.547 | 12.857 | 0.000 |
| FCA-C | 1.481 (0.539, 2.422) | 0.480 | 9.499 | 0.002 |
RASP, radiological adjacent segment pathology; AFH-C, change of post-operative anterior height of fused segments comparing to preoperative; PFH-C, change of post-operative posterior height of fused segments comparing to preoperative; C27CA-C, change of post-operative C2-7 Cobb angle comparing to preoperative; FCA-C, change of post-operative fused segment Cobb angle comparing to preoperative; OR, odds ratio.
Table 5
| Parameters | β | Wald χ2 | P value | HR |
|---|---|---|---|---|
| C27 CA-C | –1.091 | 4.381 | 0.013* | 0.336 (0.121–0.933) |
| FCA-C | –0.279 | 0.412 | 0.521 | 0.756 (0.322–1.775) |
RASP, radiological adjacent segment pathology; C27CA-C, change of post-operative C2-7 Cobb angle comparing to preoperative; FCA-C, change of post-operative fused segment Cobb angle comparing to preoperative.
Discussion
A large number of clinical studies have shown that ACF surgery can effectively relieve the pressure on the spinal cord and nerves caused by cervical spondylosis, stabilizing or alleviating the associated symptoms (1-3). As patients undergoing ACF have become younger, the long-term surgical outcomes and their impact on quality of life have received increasing attention. Among these outcomes, ASP is of great interest, since it is one of the most common reasons for revision surgery in patients who have undergone ACF surgery (4).
Typically, RASP after ACF surgery is diagnosed by an imaging examination with objective and quantifiable characteristics. Due to significant variation in follow-up times and surgical approach, the incidence of RASP varies greatly in the literature, ranging from 50% to 90% (5-7). Kulkarni et al. (5) found that, compared with remote segments, a segment adjacent to the fused segment exhibited more pronounced degenerative changes in 75% of patients who had undergone 1 or 2-level central corpectomy after a mean follow-up period of 17.5 months. In the present study, the incidence of RASP after ACF surgery was 48%, slightly less than previously reported. However, considering the relatively short follow-up, this result was basically consistent with previous studies (5-7). Although there was no significant difference in short-term recovery rates between the 2 groups, the mean recovery rate at the final follow-up was significantly lower in the RASP group than in the non-RASP group. However, the correlation between RASP and CASP is still controversial, and some researchers believe that it is either small or negligible (8,9). In this study, there was no significant correlation between the occurrence of RASP and the clinical symptoms of patients. This might be due to the relatively short follow-up period in the RASP group, in which the number of patients with CASP or undergoing further surgery was small (therefore affecting the results of statistical analysis).
Postoperative cervical lordosis may be relevant to the therapeutic outcome of cervical arthrodesis, but its influence on ASP is still uncertain. Katsuura et al. (14) and Faldini et al. (15) found that incidence of ASP in lordotic patients was significantly lower than that in non-lordotic patients after arthrodesis. However, in the studies of Kulkarni et al. (5) and Park et al. (16), the postoperative C2-7 Cobb angle was not significantly correlated with ASP, though both studies found that incidence of ASP was significantly higher in non-lordotic patients after surgery. Others have also shown that there is no correlation between post-operative cervical Cobb angle and ASP development (5,8). Most of these studies, however, only examined the patients’ postsurgical lordosis conditions, and almost entirely ignored their preoperative status. In our study, most cases demonstrated a postoperative decrease in curvature compared with their preoperative measurement; however, in the RASP group, the cervical C2-7 curvature at the final follow-up was still less than the preoperative curvature, and the situation was reversed in the non-RASP group. As suggested by Cox regression analysis in this study, a change in the C2-7 Cobb angle was significantly associated with RASP onset, even with a mild degree. In addition to structural changes brought on by surgery, cervical lordosis can be influenced by adjacent soft tissue tension; this may be largely influenced by subjective sensations, such as pain and anxiety (17). Although the post-operative change of the C2-7 Cobb angle and fused segments were closely correlated with each other, only the change in the C2-7 Cobb angle was significantly correlated with RASP when considering other confounding factors. The reason was not clear, but we speculate that the short-term decrease in the C2-7 Cobb angle may better reflect postoperative adaptation status, in addition to the structural alterations caused by surgical interventions. Though the mechanism still warrants further investigation, maintaining a lordotic cervical alignment after ACF may be beneficial in reducing postsurgical RASP onset.
At present, the influence of changes to the fused segment height on postoperative cervical curvature or RASP is still unclear. Previous studies have shown that most of the titanium cages implanted during ACF surgery collapse to some degree during follow-up (18-21), and that the type of bone graft, titanium cage diameter, and placement site may be associated with collapse degree, which has been suggested to affect postsurgical cervical lordosis. Jang et al. (18) presented a retrospective analysis of 30 patients with cervical spondylosis with ACF and titanium cage implantation, wherein 93.3% of the implants were collapsed, and the posterior part was more obvious. In this study, changes in AFH and PFH were similar to those of Jang et al. Both RASP and non-RASP groups showed a postoperative increase at the short-term follow-up and a decrease at the final follow-up, while the cervical and segmental curvature had both increased at the final follow-up. However, only the anterior height change was significantly correlated with cervical and segmental lordosis change after ACF. Most of the patients included in this study were partial corpectomy with titanium cage implantation and anterior plating. As suggested by Jang et al., use of an anterior plate may help maintain the anterior height as well as the curvature of the cervical spine after ACF. However, Cox regression only showed that the change in C2-7 Cobb angle, not the fused segment height, was significantly related to the occurrence of RASP. This result suggested graft collapse may not be the only factor affecting cervical alignment. Whole spinal segment remodeling, such as local osteoporosis and disc degeneration, may also contribute to the height change, and sampling errors could not be excluded.
The mechanism of ASP onset after ACF is still unclear. In vivo and in vitro studies have found that the range of motion of adjacent segments after fusion was significantly increased, and the intravertebral disc pressure was significantly increased. Therefore, changes in the biomechanics of adjacent segments after cervical spine surgery may be related to ASP. Compared with other parts of the spine, the cervical vertebrae have unique morphological characteristics and highly complex anatomical structure. Normal sagittal alignment is one of the important morphological features of the cervical spine, which helps to maintain the normal distribution of cervical biomechanical load. Of this load, 36% is distributed in the anterior column, and the middle posterior column (bilateral facet joints and articular processes) is subjected to the remaining 64% of the force (22). Once the cervical curvature changes, it may cause differences in the biomechanical distribution of the cervical vertebrae and contribute to ASP onset, but this speculation remains to be confirmed.
Limitations
There were certain limitations in this study that should be addressed. Firstly, in addition to the large loss of follow-up data and heterogeneity of included cases in terms of the applied surgical approach, any retrospective study may contribute recall bias and/or sampling errors to the clinical information collected, and therefore limit the generalizability of the results. However, as the incidence of RASP was in good agreement with previous studies, and there were no significant differences in surgical approach and diagnosis, we do not believe these biases would affect any difference between the 2 groups. Secondly, a retrospective study may add bias to the collected imaging data. Despite this, considering that the imaging examinations were carried out at the same institution with the same procedure, any difference between the 2 groups should be negligible. In addition, this study only examined correlations between the Cobb angle, the fused segment height, and RASP. However, the Cobb angle may not sufficiently reflect alteration of the sagittal curvature of the whole cervical spine and other important cervical alignment parameters, such as T1 tilt and chin-brow vertical angle (CBVA), were not included in the retrospective imaging data. Prospective studies are therefore still needed to clarify the role of sagittal cervical alignment in ASP development after ACF surgery.
Conclusions
These results suggest that a decrease in cervical lordosis after ACF surgery may be related to postoperative RASP development, and that differences in the anterior height of the surgical segments may be related to postoperative changes in the cervical curvature. It may therefore be beneficial for a patient to maintain a lordotic cervical curvature not less than the patient’s preoperative lordosis, after ACF surgery in order to avoid RASP development.
Acknowledgements
Funding: This work was supported by the Natural Science Foundation of Hunan Province (No. 2018JJ3799 and No. 2020JJ4839) and the New Xiangya Talent Project of the Third Xiangya Hospital of Central South University (No. JY201712).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://qims.amegroups.com/article/view/10.21037/qims-21-732/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-21-732/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). All patients provided their informed consent and the study was approved by the ethics committee of the Third Xiangya Hospital of Central South University.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Lu T, Liu C, Yang B, Liu J, Zhang F, Wang D, Li H, He X. Single-Level Anterior Cervical Corpectomy and Fusion Using a New 3D-Printed Anatomy-Adaptive Titanium Mesh Cage for Treatment of Cervical Spondylotic Myelopathy and Ossification of the Posterior Longitudinal Ligament: A Retrospective Case Series Study. Med Sci Monit 2017;23:3105-14. [Crossref] [PubMed]
- Schulz C, Mauer UM, Mathieu R. Clinical and Radiological Results after Anterior Cervical Corpectomy with Cage Fusion - a Retrospective Comparison of PEEK vs. Titanium Cages. Z Orthop Unfall 2017;155:201-8. [PubMed]
- Ghogawala Z. Anterior Cervical Option to Manage Degenerative Cervical Myelopathy. Neurosurg Clin N Am 2018;29:83-9. [Crossref] [PubMed]
- Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am 1999;81:519-28. [Crossref] [PubMed]
- Kulkarni V, Rajshekhar V, Raghuram L. Accelerated spondylotic changes adjacent to the fused segment following central cervical corpectomy: magnetic resonance imaging study evidence. J Neurosurg 2004;100:2-6. [PubMed]
- Goffin J, Geusens E, Vantomme N, Quintens E, Waerzeggers Y, Depreitere B, Van Calenbergh F, van Loon J. Long-term follow-up after interbody fusion of the cervical spine. J Spinal Disord Tech 2004;17:79-85. [Crossref] [PubMed]
- Bydon M, Xu R, De la Garza-Ramos R, Macki M, Sciubba DM, Wolinsky JP, Witham TF, Gokaslan ZL, Bydon A. Adjacent segment disease after anterior cervical discectomy and fusion: Incidence and clinical outcomes of patients requiring anterior versus posterior repeat cervical fusion. Surg Neurol Int 2014;5:S74-8. [Crossref] [PubMed]
- Ishihara H, Kanamori M, Kawaguchi Y, Nakamura H, Kimura T. Adjacent segment disease after anterior cervical interbody fusion. Spine J 2004;4:624-8. [Crossref] [PubMed]
- Matsumoto M, Okada E, Ichihara D, Watanabe K, Chiba K, Toyama Y, Fujiwara H, Momoshima S, Nishiwaki Y, Iwanami A, Ikegami T, Takahata T, Hashimoto T. Anterior cervical decompression and fusion accelerates adjacent segment degeneration: comparison with asymptomatic volunteers in a ten-year magnetic resonance imaging follow-up study. Spine (Phila Pa 1976) 2010;35:36-43. [Crossref] [PubMed]
- Kawakami M, Tamaki T, Ando M, Yamada H, Yoshida M. Relationships between sagittal alignment of the cervical spine and morphology of the spinal cord and clinical outcomes in patients with cervical spondylotic myelopathy treated with expansive laminoplasty. J Spinal Disord Tech 2002;15:391-7. [Crossref] [PubMed]
- Bhalla A, Rolfe KW. Inadequate Surgical Decompression in Patients with Cervical Myelopathy: A Retrospective Review. Global Spine J 2016;6:542-7. [Crossref] [PubMed]
- Park JB, Cho YS, Riew KD. Development of adjacent-level ossification in patients with an anterior cervical plate. J Bone Joint Surg Am 2005;87:558-63. [Crossref] [PubMed]
- Odate S, Shikata J, Soeda T, Yamamura S, Kawaguchi S. Surgical results and complications of anterior decompression and fusion as a revision surgery after initial posterior surgery for cervical myelopathy due to ossification of the posterior longitudinal ligament. J Neurosurg Spine 2017;26:466-73. [Crossref] [PubMed]
- Katsuura A, Hukuda S, Saruhashi Y, Mori K. Kyphotic malalignment after anterior cervical fusion is one of the factors promoting the degenerative process in adjacent intervertebral levels. Eur Spine J 2001;10:320-4. [Crossref] [PubMed]
- Faldini C, Pagkrati S, Leonetti D, Miscione MT, Giannini S. Sagittal segmental alignment as predictor of adjacent-level degeneration after a cloward procedure. Clin Orthop Relat Res 2011;469:674-81. [Crossref] [PubMed]
- Park MS, Kelly MP, Lee DH, Min WK, Rahman RK, Riew KD. Sagittal alignment as a predictor of clinical adjacent segment pathology requiring surgery after anterior cervical arthrodesis. Spine J 2014;14:1228-34. [Crossref] [PubMed]
- Juhl JH, Miller SM, Roberts GW. Roentgenographic Variations in the Normal Cervical Spine. Radiology 1962;78:591-7. [Crossref]
- Jang JW, Lee JK, Lee JH, Hur H, Kim TW, Kim SH. Effect of posterior subsidence on cervical alignment after anterior cervical corpectomy and reconstruction using titanium mesh cages in degenerative cervical disease. J Clin Neurosci 2014;21:1779-85. [Crossref] [PubMed]
- Pinter ZW, Reed R, Townsley SE, Mikula AL, Dittman L, Xiong A, Skjaerlund J, Michalopoulos GD, Currier B, Nassr A, Fogelson JL, Freedman BA, Bydon M, Kepler CK, Wagner SC, Elder BD, Sebastian AS. Titanium Cervical Cage Subsidence: Postoperative Computed Tomography Analysis Defining Incidence and Associated Risk Factors. Global Spine J 2021; Epub ahead of print. [Crossref] [PubMed]
- Lee JJ, Lee N, Oh SH, Shin DA, Yi S, Kim KN, Yoon DH, Shin HC, Ha Y. Clinical and radiological outcomes of multilevel cervical laminoplasty versus three-level anterior cervical discectomy and fusion in patients with cervical spondylotic myelopathy. Quant Imaging Med Surg 2020;10:2112-24. [Crossref] [PubMed]
- Chen Y, Chen D, Guo Y, Wang X, Lu X, He Z, Yuan W. Subsidence of titanium mesh cage: a study based on 300 cases. J Spinal Disord Tech 2008;21:489-92. [Crossref] [PubMed]
- Pal GP, Sherk HH. The vertical stability of the cervical spine. Spine (Phila Pa 1976) 1988;13:447-9. [Crossref] [PubMed]


