
2D ultrasound diagnosis of middle compartment prolapse: a multicenter study
Introduction
The clinical examination based on the International Continence Society Pelvic Organ Prolapse Quantification (ICS POP-Q) system is the method used for the preoperative evaluation of pelvic organ prolapse (POP) (1). However, this assessment presents a series of limitations since it not only reports the state of the anatomical surface but also uses the hymen (mobile soft tissue point) as a reference. Therefore, imaging techniques have been proposed to be more accurate than a physical examination for determining which organs are involved in POP (1). However, due to the lack of standardization, validation or the availability of imaging techniques, proposed imaging assessments have ultimately not been recommended (1).
Currently, pelvic floor ultrasound can be used as a complementary technique for many pelvic floor pathologies (2), including POP (3,4). With the objective of standardizing the ultrasound diagnosis of POP, significant prolapse is defined as a descent of ≥10 mm for the anterior compartment and ≥15 mm for the middle and posterior compartments of the corresponding organ below the posteroinferior margin of the pubic symphysis (5,6). However, ultrasound is useful not only for the diagnosis of significant prolapse of each compartment but also for the differential diagnosis of the pathology in each compartment. In the anterior compartment, different types of POP have been described according to the positioning of the urethra [Green type I: open retrovesical angle (RVA) ≥140°, urethral rotation <5°; Green type II: open RVA ≥140° and urethral rotation 45–120°; Green type III: intact RVA <140°] (7-9). It is also applied for the differential diagnosis of the pathology of the posterior compartment and has been used to define rectocele (when alterations are observed in the rectovaginal septum), enterocele (in the presence of herniation of abdominal contents to the anorectal muscle layer) and perineal hypermotility (when no fascia defects are observed) (10). Recently, a specific methodology has been defined for the differential diagnosis of middle compartment prolapse [uterine prolapse (UP) or cervical elongation (CE) without UP] (3). This examination is based on the measurement of the difference between the pubis-uterine fundus distance at rest and during the Valsalva maneuver; UP is diagnosed when this difference is ≥15 mm, with a sensitivity of 75% (95% CI: 64–86%), a specificity of 95% (95% CI: 89–100%), a positive predictive value of 86% (95% CI: 78–95%) and a negative predictive value of 89% (95% CI: 82–97%) (3). The objective of this study was to determine the multicenter concordance of an ultrasound difference of ≥15 mm between the pubis-uterine fundus distance at rest and during the Valsalva maneuver for the diagnosis of UP.
Methods
Study population
A multicenter prospective observational study was conducted [Valme University Hospital of Seville (Hospital 1), University Healthcare Complex of Gran Canaria (Hospital 2), and University Healthcare Complex of León (Hospital 3)] with 97 patients who were recruited consecutively between June 1, 2019, and October 31, 2020. The patients underwent corrective surgery of the middle compartment of the pelvic floor (correction of UP or CE without UP). The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Biomedical Ethics Committee of the Junta de Andalusia (1259-N-20). All patients gave their written informed consent before starting the study.
Patients were included who were candidates for corrective surgery of the middle compartment of the pelvic floor (correction of UP or CE without UP) after an assessment with a standardized interview and a clinical examination using the ICS POP-Q system to assess POP (1). The type of surgery performed to correct UP was classic vaginal hysterectomy with natural tissue repair via the vagina, and in patients CE without UP, the Manchester cervical amputation technique was performed. It was defined significant prolapse of each compartment was defined as Ba =−0.5, C =−5 and Bp =−0.5 (11). True CE was defined based on a C point of the Pelvic Organ Prolapse Quantification (POP-Q) system ≥0 and a D point ≤−4, as well as an estimated cervical length of ≥5 cm (12).
Examination method
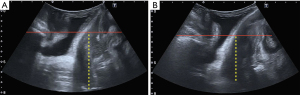
The ultrasound machines used were a Toshiba® 500 Aplio (Toshiba Medical Systems Corp., Tokyo, Japan) with a PVT-675 MV 3-dimensional abdominal probe and a Voluson E8 (GE Medical Systems, Zipf, Austria) ultrasound system with an RAB 8- to 4-MHz volume transducer covered by a sterile glove. Images were acquired from patients in the dorsal lithotomy position on the gynecological examination table under empty bladder conditions (13,14). The ultrasound study was performed using transperineal ultrasound by investigators with more than 5 years of experience in pelvic floor ultrasound (JAGM, EGD, and IO). The transducer was carefully placed (minimal possible pressure) on each patient’s perineum was applied. Two volume measurements were recorded for each patient: at rest, with maximum Valsalva maneuver [minimum of 6 s (15)]. Prior to ultrasound, the investigator verified that the Valsalsa maneuver had been performed correctly to avoid the bias of levator coactivation. Previously established criteria were used to ensure a stable reference line (6). The assessment of the descent of POP was based on the methodology described in a previous study (3) in relation to the posteroinferior margin of the pubis (6) in the midsagittal plane, with reference to the uterine fundus (established as the most distal hyperechogenic line from the pubis to the uterine fundus at rest and with the Valsalva maneuver (3) (Figure 1). We defined UP on ultrasound as a difference ≥15 mm between the pubis-uterine fundus distance at rest and with the Valsalva maneuver, and CE without UP on ultrasound was defined as a difference of <15 mm in this distance. Measurements within the posteroinferior margin of the pubis were defined as negative values, and measurements outside this margin were defined as positive values (16). As previously reported, excellent interobserver reliability in measurements of the difference in the distance from the pubic symphysis to the uterine fundus at rest and during the Valsalva maneuver have been reported for both UP and CE without UP (17).
Statistical analysis
Numerical variables are summarized as the means and deviations; qualitative variables are presented as frequencies and percentages. The comparison of numerical variables between the groups defined by the dichotomous variable UP/CE without UP was performed using Student’s t-test for independent samples or the Mann-Whitney test if the data did not meet the normality hypothesis (Shapiro-Wilk test). The association between qualitative variables was determined using Fisher’s exact test.
Cohen’s kappa coefficient of agreement and its 95% CI were used to assess the agreement between the clinical and ultrasound diagnoses of UP. Poor agreement was determined if the kappa coefficient was <0.20, weak if it ranged from 0.21 to 0.40, moderate if it ranged from 0.41 to 0.60, good if it ranged from 0.61 to 0.80 and very good if it ranged from 0.81 to 1.00 (18,19).
The minimum sample size necessary to perform the agreement study was 94 patients. We considered an α error of 5%, a β error of 20%, an expected success rate of 0.7 and kappa values under the null hypothesis and the alternative hypothesis of 0.8 and 0.6, respectively. The sample size was determined with nQuery Advisor 7.0 [2007].
Results
Of the 97 patients initially identified for inclusion in the study, 94 were evaluated (62 with UP and 32 with CE without UP): 44 patients from the Valme University Hospital of Seville (28 with UP and 16 with CE without UP), 27 patients from the University Healthcare Complex of León (20 with UP and 7 with CE without UP) and 23 patients from the University Healthcare Complex of Gran Canaria (14 with UP and 9 with CE without UP). We excluded 3 patients who underwent surgery outside the study centers. The clinical data of the patients evaluated and classified according to the presence of UP or CE without UP are shown in Table 1. The patients with UP were older (62.47 vs. 54.77 years; P=0.001). However, no differences between the groups in BMI (27.53 vs. 28.14; P=0.748), number of deliveries (2.86 vs. 2.53; P=0.076), number of cesarean sections (0.08 vs. 0.25; P=0.160), number of abortions (0.33 vs. 0.75; P=0.063) or menopausal age (53.02 vs. 52.33 years; P=0.532). The UP group had greater rates of cystocele (78.4% vs. 37%; P<0.0005), rectocele (25.5% vs. 7.0%; P=0.026) and enterocele (15.7% vs. 2.3%; P=0.036).
Table 1
| Characteristic | UP (ICS POP-Q) (n=51) | CE without UP (ICS POP-Q) (n=43) | P | 95% CI |
|---|---|---|---|---|
| Age, years | 62.47±11.17 | 54.77±11.45 | 0.001 | 4 to 14 |
| BMI, kg/m2 | 27.53±3.39 | 28.14±4.49 | 0.748 | −1.8 to 1.4 |
| Deliveries | 2.86±1.29 | 2.53±1.69 | 0.076 | −0.29 to 0.96 |
| Caesarean sections | 0.08±0.34 | 0.25±0.67 | 0.160 | −0.4 to 0.07 |
| Abortions | 0.33±0.66 | 0.75±1.19 | 0.063 | −0.84 to 0.001 |
| Menopausal age | 53.02±8.43 | 52.33±5.19 | 0.532 | −3 to 2 |
| Stress incontinence | 12 (23.5) | 6 (14.0) | 0.298 | −6.4% to 25.5% |
| Urge incontinence | 15 (29.4) | 11 (25.6) | 0.818 | −14.7% to 22.4% |
| Mixed incontinence | 7 (13.7) | 4 (9.3) | 0.541 | −8.9% to 17.8% |
| Cystocele | 40 (78.4) | 16 (37.2) | <0.0005 | 22.4% to 60.0% |
| Rectocele | 13 (25.5) | 3 (7.0) | 0.026 | 4.0% to 33.1% |
| Enterocele | 8 (15.7) | 1 (2.3) | 0.036 | 2.1% to 24.6% |
Data are represented by mean ± SD or n (%). UP, uterine prolapse; CE, cervical elongation.
The pubis-uterine fundus measurement at rest was −68.20±10.52 mm in the patients with UP and −68.53±18.51 mm in the patients with CE without UP (P=0.919). The pubis-uterine fundus measurement with the Valsalva maneuver was −40.21±15.14 mm in the patients with UP and −61.59±18.77 mm in the patients with CE without UP (P<0.0005). The difference in the pubis-uterine fundus measurement at rest and with the Valsalva maneuver was 27.99±10.64 mm in the patients with UP and 6.95±4.24 mm in the patients with CE without UP (P<0.0005) (Table 2).
Table 2
| Pubis-uterine fundus measurement | UP (ICS POP-Q) (n=51) | CE without UP (ICS POP-Q) (n=43) | P | 95% CI |
|---|---|---|---|---|
| Pubis-uterine fundus measurement in rest (mm) | −68.20±10.52 | −68.53±18.51 | 0.919 | −5.71 to 6.38 |
| Pubis-uterine fundus measurement in Valsalva (mm) | −40.21±15.14 | −61.59±18.77 | <0.0005 | 14.43 to 28.32 |
| Pubis-uterine fundus measurement: difference between rest and Valsalva (mm) | 27.99±10.64 | 6.95±4.24 | <0.0005 | 16 to 23 |
Data are represented by mean ± SD. UP, uterine prolapse; CE, cervical elongation.
Table 3 shows the kappa index for the ultrasound diagnosis of UP and of CE without UP. The ultrasound diagnosis of UP (≥15 mm between the pubis-uterine fundus distance at rest and with the Valsalva maneuver) was present in 54.3% of the general population, in 54.5% of the patients from Hospital 1, in 55.6% of the patients from Hospital 2 and in 52.2% of the patients from Hospital 3. The ultrasound diagnosis of global UP at the three centers showed very good agreement, with a kappa index of 0.826 (95% CI: 0.71–0.94). The agreement of ultrasound with the clinical diagnosis of UP with the ICS POP-Q system was very good for each of the hospitals [Hospital 1: 0.814 (95% CI: 0.64–0.98), Hospital 2: 0.847 (95% CI: 0.64–1) and Hospital 3: 0.824 (95% CI: 0.59–1)].
Table 3
| Hospitals and diagnosis of the type of POP with ultrasound |
UP (ICS POP-Q) | CE without UP (ICS POP-Q) | P value (McNemar) | Kappa (95% CI) |
|---|---|---|---|---|
| All hospital | 0.008 | 0.826 (0.71–0.94) | ||
| UP (ultrasound) | 51 (54.3%) | 0 (0.0%) | ||
| CE without UP (ultrasound) | 8 (8.5%) | 35 (37.2%) | ||
| Hospital 1 | 0.063 | 0.814 (0.64–0.98) | ||
| UP (ultrasound) | 24 (54.5%) | 0 (0.0%) | ||
| CE without UP (ultrasound) | 4 (9.1%) | 16 (36.4) | ||
| Hospital 2 | 0.250 | 0.847 (0.64–1) | ||
| UP (ultrasound) | 15 (55.6%) | 0 (0.0%) | ||
| CE without UP (ultrasound) | 2 (7.4%) | 10 (37.0%) | ||
| Hospital 3 | 0.250 | 0.824 (0.59–1) | ||
| UP (ultrasound) | 12 (52.2%) | 0 (0.0%) | ||
| CE without UP (ultrasound) | 2 (8.7%) | 9 (39.1%) |
ICS POP-Q, International Continence Society Pelvic Organ Prolapse Quantification; UP, uterine prolapse; CE, cervical elongation.
Discussion
We observed that the ultrasound diagnosis of UP based on the difference of ≥15 mm between the pubis-uterine fundus distance at rest and with the Valsalva maneuver presents very good agreement [kappa index 0.826 (95% CI: 0.71–0.94)], and this agreement is maintained when we studied the different hospitals individually (hospital 1: 0.814 (95% CI: 0.64–0.98), hospital 2: 0.847 (95% CI: 0.64–1) and Hospital 3: 0.824 (95% CI: 0.59–1). Therefore, we deduced that the concordance between the ultrasound and clinical diagnosis is not influenced by the investigator or the hospital where it is performed. This good concordance between the symptoms and ultrasound may affect the usual clinical symptoms, since ultrasound could assist with the management of those patients with UP in which uterine descent is not clinically evident.
This study confirmed the diagnostic utility of this parameter for the differential ultrasound diagnosis of middle compartment POP. Previously, significant prolapse of the middle compartment was defined when the cervix exceeded the posteroinferior ridge of the pubis by more than 15 mm during the Valsalva maneuver (6). However, that study (6) did not it assess the apical fixation points of the POP. Therefore, it does not allow the differential diagnosis of middle compartment POP, which includes two different pathologies, UP and CE without UP. A particular aspect that differentiates UP from CE without UP is that CE without UP has a relatively intact DeLancey level I (uterosacral-cardinal ligament complex). In fact, this characteristic feature is clinically observable, and the differential diagnosis between the two pathologies can be made with the pelvic organ prolapse quantification system (POP-Q) (1).
The ultrasound assessment of mean POP and its correlation with clinical POP has been discussed in the literature. The application of the ICS POP-Q system to these patients presents a series of limitations because it only provides information on the anatomical surface and uses the hymen (mobile soft tissue point) as a reference point. Therefore, an attempt was made to correlate this reference point (hymen) using transperineal ultrasound, and the results indicated the superiority of the clinical assessment over ultrasound determination (20). However, this study did not include patients with prolapse greater than stage 2 on the POP-Q (20). Additionally, they have defined that 2D translabial ultrasound is superior to assessment by POP-Q for the evaluation of POP (21). Other authors have described a good correlation (r=0.77) (22) between ultrasound and middle compartment POP, which contradicts the results described in later studies showing weaker correlations (23). A recent study shows that a difference of ≥15 mm (area under the curve was 0.81) in the pubis-uterine fundus distance at rest and with the Valsalva maneuver is useful for differentiating UP from CE without UP by ultrasound (3). Five years after surgery, a preserved original length of the mesh with apical support correlated with improved anatomical and patient-reported outcomes (4).
Preoperative transperineal ultrasound for POP not only reveals the anatomical state of the different pelvic structures but also helps to assess the degree of support of the different structures. In our study, by examining the difference in the pubis-uterine fundus measurement at rest and with the Valsalva maneuver, we indirectly evaluated apical support. As previously reported, in the study of the middle compartment POP the apical support is important (24). In fact, the closure of the levator hiatus by the levator ani muscle associated with the ligament support determines the support of the pelvic organs (25). In cases of apical support failure, a 20% increase in the length of the cardinal ligaments is observed (26). When we apply these concepts to patients with POP, we observe in patients with POP that the change in the length of these ligaments during the Valsalva maneuver is double that in patients with normal support (26). The identification of patients with apical support outside the normal range is useful for determining which patients require a hysterectomy and/or an apical support procedure, thus avoiding unnecessary surgical treatments (24).
The most important strength of this study is that it was a multicenter study that included an adequate number of patients and used different ultrasound equipment, suggesting that ultrasound is a useful parameter for the differential diagnosis of middle compartment POP. We have compared the pubis-uterine fundus to the POP-Q; however, apical support (middle compartment) is the lower end of the cervix, and we assume that the mobility of the uterine fundus is closely related to mobility of the lower end of the cervix, because the mobility of the uterus due to apical failure mobilizes the organ as a whole. Also, as previously reported, excellent interobserver variability has been obtained when we use the pubis-uterine fundus distance (17), therefore it is a technique that we can apply clinically. This fact favors its usefulness in routine clinical practice. In addition, by assessing the relationship between measures taken at rest and with the Valsalva maneuver, each patient can be considered individually, unlike when fixed cutoff points are used, as in previous studies of the diagnosis of significant POP (6). However, a possible limitation is that the ultrasound study was performed in the dorsal lithotomy position, and this position might limit the POP output. On the other hand, studies that assessed POP (during the Valsalva maneuver) in the supine position found no differences in POP descent compared to the standing position (27). Furthermore, in future studies, a convenient approach would be to relate the POP-Q measurements with the ultrasound descent of the uterus, as well as to determine new measurements for the study of the descent of the vaginal vault in hysterectomized patients. Similarly, further studies are needed to clarify whether this technique is equally useful in patients with anteverted or retroverted uteri or in patients with the presence of uterine fibroids, as well as its relationship with the different states of the POP-Q. Another potential limitation might be the force exerted by the transducer on the perineum at the time of image capture, which would potentially limit the POP output. Therefore, we recommend using minimal pressure of the transducer on the perineum to obtain a high-quality image.
Conclusions
In conclusion, we determined that a difference of ≥15 mm between the pubis-uterine fundus distance at rest and with the Valsalva maneuver presents very good agreement [kappa index 0.826 (0.71, 0.94)] with the results of clinical assessment with the ICS POP-Q system for the diagnosis of UP.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/qims-21-707). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Biomedical Ethics Committee of the Junta de Andalusia (1259-N-20). All patients gave their written informed consent before starting the study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bump RC, Mattiasson A, Bø K, Brubaker LP, DeLancey JO, Klarskov P, Shull BL, Smith AR. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 1996;175:10-7. [Crossref] [PubMed]
- AIUM/IUGA practice parameter for the performance of Urogynecological ultrasound examinations: Developed in collaboration with the ACR, the AUGS, the AUA, and the SRU. Int Urogynecol J 2019;30:1389-400. [Crossref] [PubMed]
- García-Mejido JA, Ramos-Vega Z, Armijo-Sánchez A, Fernández-Palacín A, García-Jimenez R, Sainz JA. Differential diagnosis of middle compartment pelvic organ prolapse with transperineal ultrasound. Int Urogynecol J 2021;32:2219-25. [Crossref] [PubMed]
- Poutakidis G, Marsk A, Altman D, Falconer C, Morcos E. Ultrasound evaluation of anterior transvaginal mesh for pelvic organ prolapse: correlation to 5-year clinical outcomes. Int Urogynecol J 2021; [Epub ahead of print]. [Crossref] [PubMed]
- Dietz HP, Lekskulchai O. Ultrasound assessment of pelvic organ prolapse: the relationship between prolapse severity and symptoms. Ultrasound Obstet Gynecol 2007;29:688-91. [Crossref] [PubMed]
- Shek KL, Dietz HP. What is abnormal uterine descent on translabial ultrasound? Int Urogynecol J 2015;26:1783-7. [Crossref] [PubMed]
- Eisenberg VH, Chantarasorn V, Shek KL, Dietz HP. Does levator ani injury affect cystocele type? Ultrasound Obstet Gynecol 2010;36:618-23. [Crossref] [PubMed]
- Green TH Jr. Urinary stress incontinence: differential diagnosis, pathophysiology, and management. Am J Obstet Gynecol 1975;122:368-400. [Crossref] [PubMed]
- Chantarasorn V, Dietz HP. Diagnosis of cystocele type by clinical examination and pelvic floor ultrasound. Ultrasound Obstet Gynecol 2012;39:710-4. [Crossref] [PubMed]
- Dietz HP, Steensma AB. Posterior compartment prolapse on two-dimensional and three-dimensional pelvic floor ultrasound: the distinction between true rectocele, perineal hypermobility and enterocele. Ultrasound Obstet Gynecol 2005;26:73-7. [Crossref] [PubMed]
- Dietz HP, Mann KP. What is clinically relevant prolapse? An attempt at defining cutoffs for the clinical assessment of pelvic organ descent. Int Urogynecol J 2014;25:451-5. [Crossref] [PubMed]
- Park YJ, Kong MK, Lee J, Kim EH, Bai SW. Manchester Operation: An Effective Treatment for Uterine Prolapse Caused by True Cervical Elongation. Yonsei Med J 2019;60:1074-80. [Crossref] [PubMed]
- Dietz HP, Simpson JM. Levator trauma is associated with pelvic organ prolapse. BJOG 2008;115:979-84. [Crossref] [PubMed]
- Dietz HP, Shek KL. Tomographic ultrasound imaging of the pelvic floor: which levels matter most? Ultrasound Obstet Gynecol 2009;33:698-703. [Crossref] [PubMed]
- Orejuela FJ, Shek KL, Dietz HP. The time factor in the assessment of prolapse and levator ballooning. Int Urogynecol J 2012;23:175-8. [Crossref] [PubMed]
- Dietz HP. Ultrasound imaging of the pelvic floor. Part I: two-dimensional aspects. Ultrasound Obstet Gynecol 2004;23:80-92. [Crossref] [PubMed]
- García-Mejido JA, Ramos Vega Z, Armijo Sánchez A, Fernández-Palacín A, Fernández CB, Sainz Bueno JA. Interobserver variability of ultrasound measurements for the differential diagnosis of uterine prolapse and cervical elongation without uterine prolapse. Int Urogynecol J 2021; [Epub ahead of print]. [Crossref] [PubMed]
- Altman DG. Practical statistics for medical research. New York: Chapman and Hall, 1991.
- Bloch DA, Kraemer HC. 2 x 2 kappa coefficients: measures of agreement or association. Biometrics 1989;45:269-87. [Crossref] [PubMed]
- Lone FW, Thakar R, Sultan AH, Stankiewicz A. Accuracy of assessing Pelvic Organ Prolapse Quantification points using dynamic 2D transperineal ultrasound in women with pelvic organ prolapse. Int Urogynecol J 2012;23:1555-60. [Crossref] [PubMed]
- Kluivers KB, Hendriks JC, Shek C, Dietz HP. Pelvic organ prolapse symptoms in relation to POPQ, ordinal stages and ultrasound prolapse assessment. Int Urogynecol J Pelvic Floor Dysfunct 2008;19:1299-302. [Crossref] [PubMed]
- Dietz HP, Haylen BT, Broome J. Ultrasound in the quantification of female pelvic organ prolapse. Ultrasound Obstet Gynecol 2001;18:511-4. [Crossref] [PubMed]
- Broekhuis SR, Kluivers KB, Hendriks JC, Fütterer JJ, Barentsz JO, Vierhout ME. POP-Q, dynamic MR imaging, and perineal ultrasonography: do they agree in the quantification of female pelvic organ prolapse? Int Urogynecol J Pelvic Floor Dysfunct 2009;20:541-9. [Crossref] [PubMed]
- Swenson CW, Smith TM, Luo J, Kolenic GE, Ashton-Miller JA, DeLancey JO. Intraoperative cervix location and apical support stiffness in women with and without pelvic organ prolapse. Am J Obstet Gynecol 2017;216:155.e1-8. [Crossref] [PubMed]
- Chen L, Ashton-Miller JA, DeLancey JOL. A 3D finite element model of anterior vaginal wall support to evaluate mechanisms underlying cystocele formation. J Biomech 2009;42:1371-7. [Crossref] [PubMed]
- Luo J, Betschart C, Chen L, Ashton-Miller JA, DeLancey JO. Using stress MRI to analyze the 3D changes in apical ligament geometry from rest to maximal Valsalva: a pilot study. Int Urogynecol J 2014;25:197-203. [Crossref] [PubMed]
- Rodríguez-Mias NL, Subramaniam N, Friedman T, Shek KL, Dietz HP. Prolapse assessment supine and standing: do we need different cutoffs for "significant prolapse"? Int Urogynecol J 2018;29:685-9. [Crossref] [PubMed]


