
3D printed coronary models offer new opportunities for developing optimal coronary CT angiography protocols in imaging coronary stents
Three-dimensional (3D) printing is a rapidly evolving technology with applications in different medical fields. An increasing trend in research and publications have been observed recently in the journal of Quantitative Imaging in Medicine and Surgery (QIMS), especially in the 2019 January special issue with a focus on 3D printing in medicine. In that special issue, a number of publications (original studies, technical notes and review articles) were contributed by researchers from different countries with expertise in different fields highlighting the importance of 3D printing in medical applications (1-13). In addition to these applications, a recent paper in this issue of QIMS presents another new research direction of using personalized 3D printed coronary artery models for simulation of coronary stenting procedure (14).
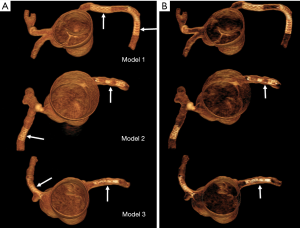
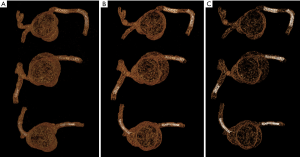
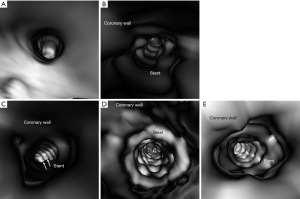
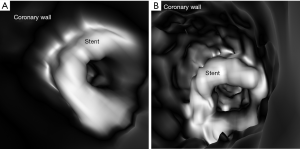
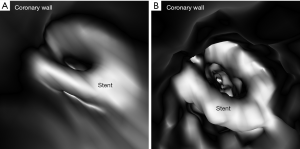
Authors in this experimental study demonstrated the feasibility of placing a number of coronary stents with different diameters into three patient-specific 3D printed coronary models. They scanned the models with the latest third generation 192-slice dual-source computed tomography (CT) scanner with images reconstructed using different kernels (smooth and sharp kernel algorithms) to study the effect on visualization of stent lumen visibility. Both 2D and 3D images were generated from the original data for demonstration of stent position and patency as well as stent lumen within the coronary arteries (Figure 1). Of 6 stents placed in the 3D printed coronary models, 2 of them failed to obtain wall apposition due to insufficient balloon expansion during stenting procedure. The visibility of stent lumen was found to be overall good ranging from 54% to 97% with the lowest visibility seen in the stents which did not achieve full expansion. The sharp kernel algorithm significantly improved the visualization of stent lumen, and this is especially apparent in detecting stenting regions where there were stent wires overlapping or stents were placed in the tortuous coronary location (Figures 2,3). Further, authors produced 3D virtual intravascular endoscopy (VIE) intraluminal views of these stents with demonstration of stent location in relation to the coronary wall (Figures 4-6). VIE images provide further information to confirm patency of these stents and their position inside the coronary arteries. When images were reconstructed with a sharp kernel algorithm, visualization of stent structures is improved when compared to those with a smooth kernel algorithm (Figures 4-6).

It is well known that 3D printing in cardiovascular disease mainly focuses on pre-surgical planning and simulation of complex cardiovascular (primarily in congenital heart disease) procedures, and the current research in this area is dominated by case reports, case series and some original studies (15-17). With regard to usefulness of 3D printed coronary models, the current literature shows their applications in guiding or managing treatment of complex coronary anomalies (18-22), while there is little or no information available about the simulation of coronary stenting. There are only a few studies reporting the research of developing optimal CT scanning protocols based on 3D printed heart and pulmonary artery models (2,3,23,24). In this study we further extend 3D printing’s application to simulating coronary stenting in the 3D printed realistic models, which is different from a previous study based on coronary stenting in a simple plastic tube (25). These 3D printed models were created from patient’s cardiac CT images, thus replicating the actual diameters and dimensions of coronary anatomy, therefore, creating opportunities for testing different scanning parameters for identification of optimal coronary CT protocols in coronary stenting.
Despite novelty of utilizing 3D printed coronary models in coronary stenting, this preliminary report will need to be further improved by simulating a wide range of coronary stents with inclusion of different materials. To represent the realistic physiological condition, 3D printed models should be filled with contrast medium to simulate contrast-enhanced coronary CT angiography, thus, allowing more accurate assessment of stent lumen diameter. Furthermore, simulation of in-stent restenosis is another area that deserves to be investigated due to the importance of detecting the restenosis following coronary stenting procedure. These areas are well highlighted in the study limitations and further results are expected to arise from this exciting proof-of-concept research report.
Acknowledgments
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Sun Z. Insights into 3D printing in medical applications. Quant Imaging Med Surg 2019;9:1-5. [Crossref] [PubMed]
- Aldosari S, Jansen S, Sun Z. Optimization of computed tomography pulmonary angiography protocols using 3D printed model with simulation of pulmonary embolism. Quant Imaging Med Surg 2019;9:53-62. [Crossref] [PubMed]
- Aldosari S, Jansen S, Sun Z. Patient-specific 3D printed pulmonary artery model with simulation of peripheral pulmonary embolism for developing optimal computed tomography pulmonary angiography protocols. Quant Imaging Med Surg 2019;9:75-85. [Crossref] [PubMed]
- Sun Z, Ng CK, Squelch A. Synchrotron radiation computed tomography assessment of calcified plaques and coronary stenosis with different slice thicknesses and beam energies on 3D printed coronary models. Quant Imaging Med Surg 2019;9:6-22. [Crossref] [PubMed]
- Witowski J, Darocha S, Kownachi L, Pietrasik A, Pietura R, Banaszkiewicz B, Kaminski J, Biederman A, Torbicki A, Kurzyna M. Augmented reality and three-dimensional printing in percutaneous interventions on pulmonary arteries. Quant Imaging Med Surg 2019;9:23-9. [Crossref] [PubMed]
- Witowski J, Wake N, Grochowska A, Sun Z, Budzynski A, Major P, Popiela TJ, Pedziwiatr M. Investigating accuracy of 3d printed liver models with computed tomography. Quant Imaging Med Surg 2019;9:43-52. [Crossref] [PubMed]
- Allan A, Kealley C, Squelch A, Wong YH, Yeong CH, Sun Z. Patient-specific 3D printed model of biliary ducts with congenital cyst. Quant Imaging Med Surg 2019;9:86-93. [Crossref] [PubMed]
- Maier J, Weiherer M, Huber M, Palm C. Imitating human soft tissue on basis of a dual-material 3D print using a support-filled metamaterial to provide bimanual haptic for a hand surgery training system. Quant Imaging Med Surg 2019;9:30-42. [Crossref] [PubMed]
- He Y, Liu Y, Dyer BA, Boone JM, Liu S, Chen T, Zheng F, Zhu Y, Sun Y, Rong R, Qiu J. 3D printed breast phantom for multi-purpose and multi-modality imaging. Quant Imaging Med Surg 2019;9:63-74. [Crossref] [PubMed]
- Zhang F, Zhang H, Zhao H, He Z, Shi L, He Y, Ju N, Rong Y, Qiu J. Design and fabrication of a personalized anthropomorphic phantom using 3D printing and tissue equivalent materials. Quant Imaging Med Surg 2019;9:94-100. [Crossref] [PubMed]
- Denizet G, Calame P, Lihoreau T, Kleinclauss F, Aubry S. 3D multi-tissue printing for kidney transplantation. Quant Imaging Med Surg 2019;9:101-6. [Crossref] [PubMed]
- Lau I, Wong YH, Yeong CH, Abdul Aziz Y, Md Sari N, Hashim A, Sun Z. Quantitative and qualitative comparison of low- and high-cost 3D printed heart models. Quant Imaging Med Surg 2019;9:107-14. [Crossref] [PubMed]
- Kiraly L, Kiraly B, Szigeti K, Tamas CZ, Daranyi S. Virtual museum of congenital heart defects: digitization and establishment of a database for cardiac surgeons. Quant Imaging Med Surg 2019;9:115-26. [Crossref] [PubMed]
- Sun Z, Jansen S. Personalized 3D printed coronary models in coronary stenting. Quant Imaging Med Surg 2019;9:1356.
- Sun Z, Lau I, Wong YH, Yeong CH. Personalised three-dimensional printed models in congenital heart disease. J Clin Med 2019;8:522. [Crossref] [PubMed]
- Lau IWW, Liu D, Xu L, Fan Z, Sun Z. Clinical value of patient-specific three-dimensional printing of congenital heart disease: Quantitative and qualitative assessments. PLoS One 2018;13:e0194333. [Crossref] [PubMed]
- Valverde I, Gomez-Ciriza G, Hussain T, Suarez-Mejias C, Velasco-Forte MN, Byrne N, Ordoñez A, Gonzalez-Calle A, Anderson D, Hazekamp MG, Roest AAW, Rivas-Gonzalez J, Uribe S, El-Rassi I, Simpson J, Miller O, Ruiz E, Zabala I, Mendez A, Manso B, Gallego P, Prada F, Cantinotti M, Ait-Ali L, Merino C, Parry A, Poirier N, Greil G, Razavi R, Gomez-Cia T, Hosseinpour AR. Three dimensional printed models for surgical planning of complex congenital heart defects: an international multicenter study. Eur J Cardiothorac Surg 2017;52:1139-48. [Crossref] [PubMed]
- Lee M, Moharem-Elgamal S, Beckingham R, Hamilton M, Manghat N, Milano EG, Bucciarelli-Ducci C, Caputo M, Biglino G. Evaluating 3D-printed models of coronary anomalies: a survey among clinicians and researchers at a university hospital in the UK. BMJ Open 2019;9:e025227. [Crossref] [PubMed]
- Misra A, Walters HL, Kobayashi D. Utilisation of a three-dimensional printed model for the management of coronary-pulmonary artery fistula from left main coronary artery. Cardiol Young 2019;29:431-4. [Crossref] [PubMed]
- Oliveira-Santos M, Oliveira Santos E, Marinho AV, Leite L, Guardado J, Matos V, Pego GM, Marques JS. Patient-specific 3D printing simulation to guide complex coronary intervention. Rev Port Cardiol 2018;37:541.e1-541.e4. [Crossref] [PubMed]
- Aroney N, Lau K, Daniele L, Burstow D, Walters D. Three-dimensional printing: to guide management of a right coronary artery to left ventricular fistula. Eur Heart J Cardiovasc Imaging 2018;19:268. [Crossref] [PubMed]
- Velasco Forte MN, Byrne N, Valverde Perez I, Bell A, Gómez-Ciriza G, Krasemann T, Sievert H, Simpson J, Pushparajah K, Razavi R, Qureshi S, Hussain T. 3D printed models in patients with coronary artery fistulae: anatomical assessment and interventional planning. EuroIntervention 2017;13:e1080-3. [Crossref] [PubMed]
- Abdullah KA, McEntee MF, Reed W, Kench PL. Development of an organ-specific insert phantom generated using a 3D printer for investigations of cardiac computed tomography protocols. J Med Radiat Sci 2018;65:175-83. [Crossref] [PubMed]
- Sun Z. Personalized three-dimensional printed coronary artery models for accurate assessment of coronary stenosis using high resolution imaging. Australasian Med J 2019;12:105-9.
- Hickethier T, Wenning J, Doerner J, Maintz D, Michels G, Bunck AC. Fourth update on CT angiography of coronary stents: in vitro evaluation of 24 novel stent types. Acta Radiol 2018;59:1060-5. [Crossref] [PubMed]


