Radiological changes of spine and liver in a case of Alagille syndrome
Alagille syndrome is a well-known, clinically important, but infrequent disease. It is an autosomal dominant disorder characterized by genetic abnormalities of Jag 1 and the Notch signaling pathway (1,2). Alagille syndrome is histologically characterized by a paucity of intrahepatic bile ducts leading to chronic cholestasis. Laboratory findings are often remarkable with serum bilirubin values up to 30 times the normal and serum bile salts up to 100 times the normal (3). It is a cause of cholestasis among children and adolescent anatomically, awareness of this congenital anomaly is important for the diagnosis and treatment. In addition to liver disease, Alagille syndrome can be associated with cardiac disease, skeletal and ocular anomalies, and characteristic facial features (4,5). Rare cases of Alagille syndrome have been reported in the literature. We herein describe a case of Alagille syndrome in a 20-year-old woman. The diagnosis of Alagille syndrome was made on the basis of combination of genetic testing for Jag 1 mutation and characteristic clinical findings.
A 20-year-old female patient presenting jaundice from birth was referred to the authors’ hospital. Her medical history included congenital biliary atresia with yellow discoloration of the skin, sclera, and mucous membranes soon after birth, which prompted a thorough systemic evaluation. She had been diagnosed “cytomegalovirus hepatitis” in one hospital 17 years ago, and liver biopsy revealed biliary cirrhosis in another hospital when she was 12 years old. Laboratory tests in the authors’ hospital revealed: WBC 0.46×109/L, PLT 18×109/L, RBC 2.32×1012/L. Bone marrow biopsy showed hyperplasia of bone marrow. Total bilirubin 188 µmol/L, direct bilirubin 127 µmol/L, total bile acid 211.7 µmol/L, ALT 50 U/L, AST 90 U/L, GGT 179 U/L, ALP 278 U/L, AFP 1.85 ng/mL, increased fibrosis-4 index, serology for HBV was positive. On physical examination, she was 145 cm high with short neck, developmental delay, had part “Alagille syndrome” characteristic face (i.e., broad forehead, deep-set eyes and straight nose) (4,5).
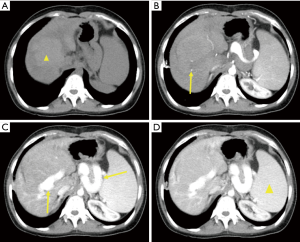
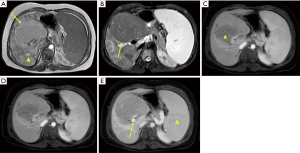
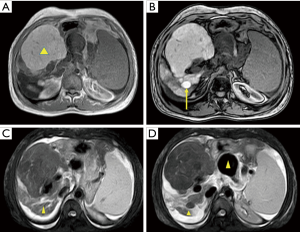
An anteroposterior X-ray revealed split vertebrae at T10 with two lateral halves, suggesting butterfly vertebra, and spinal scoliosis at the T10 level. Lateral X-rays showed anterior wedging of the T10 vertebrae. CT of the thoracolumbar region revealed two hemivertebrae, with a complete central cleft at T10 and complementary vertebral shapes at the adjacent vertebrae (Figure 1). A well-defined hypoechoic mass in segment IV of the liver was noted with ultrasound. This mass was hyperdense on unenhanced CT, measuring 3.8 cm × 3.6 cm with minimal hypervascularity in the arterial phase. The portal phase showed heterogeneous hypoattenuation (mimicking consistent with hepatocellular carcinoma) and enlarged portal vein (right branch) and splenic vein (Figure 2). Additional features of cirrhosis, portal hypertension and significant splenomegaly were noted. MRI showed an isointense mass on T1W images, which was heterogeneously hypointense on T2W images. At the same time, T1W MRI revealed many other regenerating nodules in the surrounding hepatic parenchyma. On the enhanced T1W sequences the mass demonstrated areas of poor arterial enhancement, which retained hypointense in delayed imaging (Figure 3). It was reported as a big benign regenerating nodule. After 2 years, the follow-up MRI show the mass volume in the right hepatic lobe increased slowly (Figure 4).
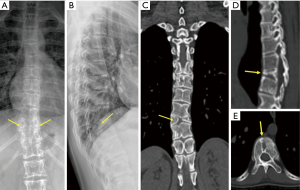
Finally, the diagnosis of Alagille syndrome was made on the basis of combination of genetic testing for Jag 1 mutation and characteristic clinical findings (chronic cholestasis/jaundice due to conjugated hyperbilirubinaemia, butterfly vertebra and dysmorphic face). This case suggests that despite the rarity of Alagille syndrome, awareness of this congenital anomaly is important.
Acknowledgements
Funding: This work was supported by the Sanming Project of Medicine in Shenzhen (SZSM201612053)
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Alagille D, Habib EC, Thomassin N. L'atresie des voies biliaires intrahepatiques avec voies biliaires extrahepatiques permeables chez l'enfant. J Par Pediatr 1969:301-318.
- Li L, Krantz ID, Deng Y, Genin A, Banta AB, Collins CC, Qi M, Trask BJ, Kuo WL, Cochran J, Costa T, Pierpont ME, Rand EB, Piccoli DA, Hood L, Spinner NB. Alagille syndrome is caused by mutations in human Jagged1, which encodes a ligand for Notch1. Nat Genet 1997;16:243-51. [Crossref] [PubMed]
- Suchy FJ, Sokol RJ, Balistreri WF. Liver disease in children. New York: Cambridge University Press, 2014.
- Alagille D, Estrada A, Hadchouel M, Gautier M, Odièvre M, Dommergues JP. Syndromic paucity of interlobular bile ducts (Alagille syndrome or arteriohepatic dysplasia): review of 80 cases. J Pediat 1987;110:195-200. [Crossref] [PubMed]
- Turnpenny PD, Ellard S. Alagille syndrome: pathogenesis, diagnosis and management. Eur J Hum Genet 2012;20:251-7. [Crossref] [PubMed]


