Imaging in traumatic mandibular fractures
Introduction
In all facial trauma, a mandibular fracture must be excluded due to the prominence of the bone within the viscerocranium. In an acute trauma setting, before the fracture is assessed, care must be given to ensure the airway is secure and associated injuries pertaining to the patient’s primary survey are excluded. A mandibular fracture should be suspected if a patient presents with malocclusion, trismus, broken teeth or obvious step deformity.
Diagnostic imaging allows the severity of the fracture to be classified, which therefore decides treatment options. The desired outcome is to achieve corrective occlusion whilst preventing any nonunion, malunion or delayed union of the fracture.
Within this paper we discuss the epidemiology and classification of mandibular fractures as well as the varied imaging modalities used to assess this injury. In particular, we look at how computer tomography (CT) surpasses X-ray within a trauma setting, as well as the role of ultrasound and magnetic resonance imaging (MRI).
Epidemiology
A fracture of a mandible in facial trauma commonly occurs within young males aged between 16 and 30 years (1,2). In comparison to other major bones within the viscerocranium, such as the zygoma and maxilla, the mandible is noted to be fractured significantly more, representing up to 70% of all facial fractures (3).
The leading cause of mandibular fractures in this present day are motor vehicle accidents (3,4). This is partly due to the increasing number of automobiles on roads and higher speed limits allowed, thus increasing the prevalence of high velocity trauma. The second leading cause is assault, which 30–40 years ago was the first due to there being less vehicles used per capita (4,5). Furthermore, a mandibular fracture is demonstrated to occur in populations with a lower socioeconomic status. This is due to the increased prevalence of alcohol dependence and violent altercations, such as with firearms or by physical assault (6-8).
The literature describes a range of occurrences of mandibular fracture by site. The most frequent fractures are of the parasymphysis (35–50%), body (21–36%), condyle (20–26%) and of the angle (15–26%). Less common fractures are of the ramus (2–4%) and of the coronoid process (1–2%) (3,9-11). Of note, fractures of the mandibular angle are particularly encountered with physical assault due the prominence of this anatomical location (10).
Classification
There are various methods of classifying mandibular fractures; anatomically, by dentition, by muscle action and by severity. The fracture itself may be closed, open, comminuted, displaced or pathological. It is important to remember that due to its U-shape, the mandible is covered by the ‘ring bone rule’ and identification of a fracture should prompt a thorough assessment for a second fracture or dislocation. If two fractures are identified, they are more commonly positioned opposite to each other as apposed to being on the same side (12,13).
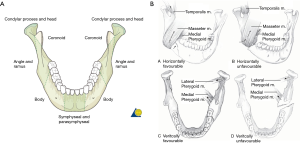
Anatomical classification is best described by Dingman and Natvig, whom locate fractures of the mandible to the symphysis, parasymphysis, body, angle, ramus, condylar process, coronoid process and alveolar process (Figure 1A) (16).
The Kazanjian and Converse Classification describes three classes based on dentition. In a Class I injury, teeth are present on both sides of the fracture line. If teeth are only present on one side of the fracture line this is a Class II injury and when both fragments about the fracture are edentulous this is Class III injury. This bears clinical relevance as teeth may be utilized for reduction of the fracture fragments and subsequent attachment of wires to maintain alignment (17).
Fractures of the angle and body can be classified by muscle action. Some fractures may be displaced or held in apposition by the surrounding musculature, which can impede or ameliorate healing respectively. Favourable fractures occur when the actions of the surrounding muscles oppose the fracture fragments. When the muscle actions result in displacement of the fracture fragments these are unfavourable fractures. Anterior fragments are generally pulled posteriorly or inferiorly and posterior fragments are generally pulled superiorly and medially (Figure 1B) (5).
A fractured mandible can also be classified according to its severity. This includes the F–F4 scoring system which is a described as: F—an undisplayed fracture line; F1—a single mobile fragment of the alveolar or basal region; F2—single separation of the mandibular arch continuity; F3—two separations of the mandibular arch continuity or F4—three or more mandibular arch fragments (Figure 2A). This bears clinical relevance as the higher the classification, the increased incidence of inferior alveolar nerve dysfunction and post-surgical complications (18).
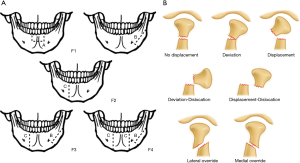
Localised condylar fractures can also be separated according to the Lindahl classification, which corresponds to the anatomical location of the fracture. This can be divided into the condylar head, neck or subcondylar region. Of note, the terms intracapsular and extracapsular are used to describe fractures of the condylar head and neck respectively, referring to the joint capsule. The fractures are then classed as being non-displaced, deviated, displaced, deviated and dislocated, displaced and dislocated, laterally overriding or medially overriding (Figure 2B). It is important to be aware that if a fracture occurs at the base of the condyle this often results in a dislocation from the temporomandibular joint (TMJ), due to the medial pull of the lateral pterygoid muscle.
Treatment
Depending on the classification of a mandibular fracture, there can be varied surgical management which is of importance to the reporting radiologist (20).
Closed reduction would be indicated for localised fractures involving the condylar region or the coronoid process (21). They are also indicated in non-displaced favourable fractures, as the opposition of the fracture is already maintained thus allowing for the simplest treatment option. Grossly comminuted fractures are also treated by this method, primarily due to inadequate stabilisation that will occur with any internal fixation (5,21).
Open reduction internal fixation (ORIF) is reserved for fractures involving the angle, body or parasymphyseal region of the mandible, where reduction cannot be achieved without intraosseous screws, wires or plating (21). They are also used in displaced unfavourable fractures in order to maintain opposition. Mandibular fractures of elderly patients, whom are edentulous, have poor cancellous bone and again require an ORIF to ensure a satisfactory outcome (5).
Imaging
The decision to image a mandibular injury can be justified if a fracture is suspected. It is important for a fracture to be identified quickly as there can be detrimental outcomes to the patient if missed, this includes malunion, nonunion and delayed union of the fracture. In the context of trauma, the presence of malocclusion, trismus, pain with the mouth closed, broken teeth or a step deformity, are all clinical features that present with a mandibular fracture. If a patient presents with any of these features they should receive X-ray imaging (22).
X-ray
X-ray evaluation of a mandibular fracture follows a set mandibular series, which involves three views; a posteroanterior (PA), oblique and lateral view. Imaging can be supplemented further with a reverse Towne’s view or an orthopantomogram (OPG). Exposure settings typically include a kVp range of 65–70 with a mAS range of 16–20. The projection would then be at a fixed distance of 40 inches.
On first review of plain radiographs the adequate image quality must be evaluated and then the cortical margins of the mandible should be traced to note any discontinuity. Particular attention should be made to the condylar areas as they are commonly overlooked. Note that any cortical break may range from being subtle to obvious where there is significant displacement. Dislocation of the condyle from the TMJ should be ruled out next and as aforementioned, fracture at the base of the condyle is a likely cause. Care should be noted that a true dislocation occurs when the condyle is anterior to the articular eminence of the temporal bone but must not be confused with the normal slight anterior displacement that appears on a lateral open mouth view.
Several X-ray views are obtained at different projections so that you are able to identify all visible fracture lines and the displacement shown. Individual views are insufficient in detailing the mandible and each have their own advantages and limitations.
A PA view accurately details fractures of the ramus, angle and body. Due to superimposed anatomy, the symphysis and condyles are displayed poorly however, being obscured by the cervical spine (c-spine) and mastoid process respectively (Figure 3A).
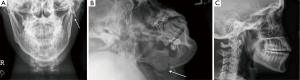
An oblique view, similarly to a PA view, visualises the ramus, angle and body well. They also detail the mandibular groove, which may be mistaken for a cortical break in other projections. The disadvantages is again limited visualisation of the condylar region as well as the symphysis. This view also may lead to a false positive of a fractured condyle, due to the superimposed anterior cortex of C2 (Figure 3B) (5).
The lateral view is particularly helpful in assessing the TMJ and any associated dislocation. A condylar fracture would also be displayed better in comparison to a PA or an oblique view, although there is limited detail in assessing any medial or lateral displacement. Another disadvantage includes the symphysis not being visualised at all in this projection. (Figure 3C).
A supplemented reverse Towne’s view can help visualise the condylar region to which is demonstrated poorly on PA and oblique projections (5). It consists of a PA view with the patient having their cervical spine (c-spine) flexed and mouth open. This allows substantial detail of the condyles and is excellent for detailing any medial or lateral displacement, with little overlapping of the mastoid bone. A disadvantage with this projection is as with a standard PA view, the symphysis is detailed inadequately due to the superimposed c-spine (Figure 4A).
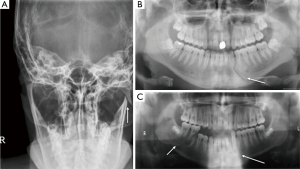
OPG X-rays is another supplemented view and images the entire mandible in a one dimensional plane. They subsequently are the most informative radiograph and are more sensitive in detecting a mandibular fracture in comparison to other X-ray views (Figure 4B,C). It has been reported to demonstrate a sensitivity of 92% of detecting a mandibular fracture in comparison to 66% with a set mandibular series (23). In particular, they demonstrate fractures clearly through the body and allow better appreciation of any comminution or segmental displacement. Although they do demonstrate increased sensitivity, similarly to oblique and PA views, OPG X-rays provide limited detail on condylar injury, particularly with medial displacement. Another limitation is that they are prone to artefact. This is due to the high radiographic skill required to obtain satisfactory images in this projection, inevitably leading to frequent inappropriate image acquisitions (24).
In unstable trauma patients whom have to remain supine and have a cervical collar present, only limited X-rays projections can be obtained. This would include a anteroposterior (AP), lateral and oblique view. These projections are inadequate in assessing the mandible in its entirety, as the condylar area is poorly detailed as well as the fracture displacement angle (5). An OPG, reverse Towne’s and a PA view are all prevented as they require the patient to be able to stand and move their neck in order to be performed. Thus, X-ray evaluation of mandibular fractures is best restricted to trauma patients whom can ambulate and have isolated injuries. When this is not the case, CT is the initial imaging modality of choice.
CT
The indications for performing CT imaging of the mandible are several. Firstly, as aforementioned, they are performed first in all unstable patients where the suspicion of mandibular fracture is present. Secondly, they are indicated when there are ongoing concerns that a fracture is likely despite not being demonstrated on X-ray. Finally, CT imaging would be performed in all patients whom have a X-ray diagnosis of a fracture that would be amenable for either a closed or open reduction. This is due to the enhanced detail provided in the images allowing for better operative planning (5,25,26).
A CT Facial bones is a series of images used to evaluate the mandibular fracture. Exposure settings should be of 120 kVp, 180 mA and with a window level of 3,000/650. The reconstructed slice thickness should be of 1–3 mm, which will provide comprehensive detail in detecting even the most subtle fracture (5,25,27).
A CT scout image taken prior to the series should be reviewed first, as it serves as a helpful comparison with initial AP and lateral X-rays views taken. The sensitivity of a scout image in detecting a mandibular fracture is however noted lower in comparison to radiograph images, and therefore should not be used as a replacement. This has been evidenced by a study conducted by the Santa Clara Valley Medical Centre after retrospectively reviewing the images of 400 traumatic mandibular fractures (5).
The advantages of CT vs. X-ray in mandibular fractures are several, and partly due to the presence of images in a three-dimensional (3D) plane. This is through the reconstructed coronal and sagittal (Figure 5) planes taken from an axial CT image (Figure 6). This therefore provides views where superimposed anatomy is avoided, which commonly occurs with X-rays projections. For example, condylar or symphyseal fractures are detailed well in CT, which is commonly obscured in a PA radiograph as discussed earlier. Furthermore, another advantage of having images in a 3D plane is that it overcomes the limited views gained by X-rays in an unstable trauma patient (5,28).
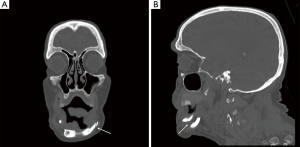
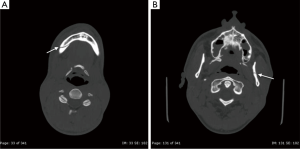
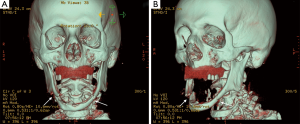
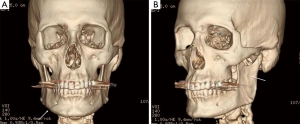
A CT facial bones series also contains a reconstructed 3D view of the mandible, which provides several benefits when assessing a fracture (Figures 7,8). Firstly, it is particularly helpful in identifying the classification and severity of this injury. This is due to a better display of the spatial relationship of the fracture with surrounding structures, and a more precise calculation of its the location and direction of displacement (27,29). This therefore allows easier identification of the fracture’s F–F4 severity score and whether it is favourable or unfavourable for example (18). Secondly, a reconstructed 3D view allows a maxillofacial surgeon a more realistic interpretation of how the fracture may appear in an operating theatre, ultimately influencing the choice of ORIF.
The overall advantages discussed with CT result in an increased sensitivity in detecting mandibular fractures in comparison to X-ray, with values reported at up to 100% (30). The lower sensitivities noted for X-ray projections is partly due to undisplaced fractures not appearing until 7–10 days after the initial injury, therefore being commonly missed upon review of the initial radiograph (1).
Although there is higher sensitivity in assessing a fracture with CT imaging, as is the radiation dose. A CT Facial bones is measured at approximately 2 mSv where as a panoramic mandibular X-ray is measured at 0.010 mSv (31). Another advantage of OPG against CT is that it provides better detail in evaluating dental structures. As a result, when a dental fracture is suspected, particularly at the mandibular angle, an OPG should be performed in addition to a CT (32). A longer scanning time is another limitation of CT vs. X-ray and can lead to motion blur producing artefacts within the image. This is seen particularly with planar sagittal and coronal reconstructions as well as reconstructed 3D views (33). To overcome motion blur, the use of multidetector-row CT (MDCT) scanners are increasingly being used as they allow faster scanning times and improve z-axis resolution (34). Its value in trauma imaging is particularly useful, as they produce acceptable reconstructive coronal imaging whereby direct coronal views cannot be obtained due to the supine patient (5).
Concomitant injuries with traumatic mandibular fractures are common, particularly intracranial lesions. They have been shown to be prevalent in up to 19% of mandibular fractures, emphasising the important of CT Brain imaging if the patient has any suspicion of head injury at the time of presentation (35). Cervical spinal injuries (CSI) are a another concomitant injury and should be suspected in patients with an altered neurological status or whom have sustained a high velocity MVA (36). Interestingly, where multiple mandibular fractures were sustained, this has demonstrated to be inversely correlated with CSI. This was hypothesised to be due to more energy being dissipated in multiple mandibular fractures therefore leading to less force transmitted to the cervical spine (37). Overall, due to the high incidence of concomitant injuries, commonly a combined CT Brain, Facial Bones & C-Spine should be performed, which will also reduce radiation through avoidance of subjecting the patient to separate scans.
Ultrasound
Ultrasonography (U/S) has been demonstrated as a useful imaging modality in detecting mandibular fractures (38,39). Sensitivities have been demonstrated at up to 94%, which is slightly higher in comparison to an OPG which has earlier been reported at 93% (30,38). The parameters of a scan should include a linear probe with a frequency of 10–15 MHz (38,40). This will allow for identification of fractures with a step-deformity, but prove harder in diagnosing non-displaced fractures. This is primarily due to a minimum of 0.2 mm displacement required to be detected by U/S (37). If high resolution echography is used however, detection can be improved to as little as 0.1 mm of displacement (41).
The overall advantages of U/S are being a fast imaging technique, relatively inexpensive and one that does not use ionising radiation. This would be particularly useful in trauma patients whom are too unstable to have a CT performed or whom are pregnant and therefore wanting to limit radiation exposure (38). U/S however, provides limited detail on quantifying the severity of the fracture due to the limited views achievable and the lack of spatial detail.
MRI
MRI of a mandibular injury is performed when assessing any associated soft tissue injuries. In particular, assessing for temporomandibular disc disruption or capsular tear which can occur with high condylar fractures (42). Detail of bony injury, which is what is required in an traumatic mandibular injury, is reserved for CT due to quicker scan times and typical 24-hour access. MRI does however serve the advantage of not using ionising radiation to the patient.
Conclusions
Diagnosis of a traumatic mandibular fracture can be performed by a variety of imaging modalities. A typical mandibular series can provide good sensitivity in detecting a fracture, whilst including quick scan times and minimal radiation dose. They are however ineffective in detailing condylar fractures due to superimposed anatomy. This can be addressed through a reverse Towne’s view but is often prevented due to restricted range of the c-spine in a trauma patient. CT imaging of the mandible, in particular MDCT, has been demonstrated to have higher sensitivity in detecting a mandible fracture in comparison to X-ray, and provide excellent detail in detecting a condylar fracture. This is due to high z-axis resolution and detailed coronal and sagittal reconstructions which have minimal artefact. In addition, the benefit of a 3D reconstructed view with CT, allows the classification and severity of the fracture to be evaluated due to the spatial information it provides. This can also be achieved with an OPG but requires an ambulant patient and a radiographer with high technical skill. Ultrasound remains useful in patients whom are too unstable to a have CT and have sensitivities comparable to X-ray in detecting a fracture. They do however provide limited detail on classification and should serve as an adjunct when evaluating a mandibular fracture. MRI is reserved for assessing soft tissue injuries associated with condylar fractures. It can be used as an additional imaging modality once the patient is stable and clinical suspicion pertinent of such injury is high.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Ceallaigh PO, Ekanaykaee K, Beirne CJ, Patton DW. Diagnosis and management of common maxillofacial injuries in the emergency department. Part 2: mandibular fractures. Emerg Med J 2006;23:927-28. [Crossref] [PubMed]
- Haug RH, Prather J, Indreasno AT. An epidemiologic survey of facial fractures and concomitant injuries. J Oral Maxillofac Surg 1990;48:926-32. [Crossref] [PubMed]
- Laub DR. Mandibular Fractures. Medscape. 2016 Jan 14. Available online: http://emedicine.medscape.com/article/1283150-overview#a4
- Vyas A, Mazumdar U, Khan F, Mehra M, Parihar L, Purohit C.. A study of mandibular fractures over a 5-year period of time: A retrospective study. Contemp Clin Dent 2014;5:452-5. [Crossref] [PubMed]
- Soule WC, Fisher LH. Mandibular Fracture Imaging. Medscape. 2015 Jul 01. Available online: http://emedicine.medscape.com/article/391549-overview
- McDade AM, McNicol RD, Ward-Booth P, Chesworth J, Moos KF. The aetiology of maxillo-facial injuries, with special reference to the abuse of alcohol. Int J Oral Surg 1982;11:152-5. [Crossref] [PubMed]
- May M, Cutchavaree A, Chadaratana P, West J. Mandibular fractures from civilian gunshot wounds: a study of 20 cases. Laryngoscope 1973;83:969-73. [Crossref] [PubMed]
- Munante-Cardenas JL, Facchina NPH, Passeri LA. Etiology, treatment, and complications of mandibular fractures. J Craniofac Surg 2015;26:611-5. [Crossref] [PubMed]
- Gadicherla S, Sasikumar P, Gill SS, Bhagania M, Kamath AT, Pentapati KC. Mandibular Fractures and Associated Factors at a Tertiary Care Hospital. Arch Trauma Res 2016;5:e30574. [Crossref] [PubMed]
- Fridrich KL, Pena-Velasco G, Olson RA. Changing trends with mandibular fractures: A review of 1067 cases. J Oral Maxillofac Surg 1992;50:586. [Crossref] [PubMed]
- King RE, Scianna JM, Petruzzeli GJ. Mandible fracture patterns: a suburban trauma center experience. Am J Otolaryngol 2004;25:301-7. [Crossref] [PubMed]
- Cillo JE Jr, Ellis E 3rd. Treatment of patients with double unilateral fractures of the mandible. J Oral Maxillofac Surg 2007;65:1461-9. [Crossref] [PubMed]
- Natu SS, Pradhan H, Gupta H, Alam S, Gupta S, Pradhan R, Mohammad S, Kohli M, Sinha VP, Shankar R, Agarwal A. An Epidemiological Study on Pattern and Incidence of Mandibular Fractures. Plast Surg Int 2012;2012:834364. [Crossref] [PubMed]
- AO Foundation. Fracture Location. Available online: https://www2.aofoundation.org/wps/portal/!ut/p/a0/04_Sj9CPykssy0xPLMnMz0vMAfGjzOKN_A0M3D2DDbz9_UMMDRyDXQ3dw9wMDAzMjfULsh0VAbWjLW0!/?bone=CMF&segment=Mandible&showPage=A&contentUrl=srg/popup/additional_material/91/X99_terminology.jsp
- Ento Key. Mandibular Fractures. 2016 May 24. Available online: https://entokey.com/mandibular-fractures/
- Dingman R, Natvig P, Reed O. Surgery of facial fractures Dingman & Paul Natvig. Philadelphia: WB Saunders; 1964.
- Kazanjian V, Converse J. Surgical Treatment of facial injuries. Baltimore: The Willians Wilkins; 1974.
- Carinci F, Arduin L, Pagliaro F, Zollino I, Brunelli G, Cenzi R.. Scoring Mandibular Fractures: A Tool for Staging Diagnosis, Planning Treatment, and Predicting Prognosis. J Trauma 2009;66:215-9. [Crossref] [PubMed]
- Powers DB. Classification of Mandibular Condylar Fractures. Atlas Oral Maxillofac Surg Clin North Am 2017;25:1-10. [Crossref] [PubMed]
- Shetty V, Atchison K, Der-Martirosian C, Wang J, Belin T. Determinants of surgical decisions about mandible fractures. J Oral Maxillofac Surg 2003;61:808-13. [Crossref] [PubMed]
- Part III Management of Head and Neck Injuries. In: Fonseca RJ, Barber HD, Powers MP, Frost DE. editors. Oral & Maxillofacial Trauma. Fourth Edition. Missouri: Elsevier Health Division; 2013:308-11.
- Charalambous C, Dunning J, Omorphos S, Cleanthous S, Begum P, Mackway-Jones K.. A maximally sensitive clinical decision rule to reduce the need for radiography in mandibular trauma. Ann R Coll Surg Engl 2005;87:259-63. [Crossref] [PubMed]
- Chayra GA, Meador LR, Laskin DM. Comparison of panoramic and standard radiographs for the diagnosis of mandibular fractures. J Oral Maxillofac Surg 1986;44:677. [Crossref] [PubMed]
- Nair MK, Nair UP. Imaging of Mandibular Trauma: ROC Analysis. Academic Emergency Medicine 2001;8:689-695. [Crossref] [PubMed]
- Manson PN, Markowitz B, Mirvis S, Dunham M, Yaremchuk M. Toward CT-based facial fracture treatment. Plast Reconstr Surg 1990;85:202-212. [Crossref] [PubMed]
- Timashpolsky A, Dagum AB, Sayeed SM, Romeiser JL, Rosenfeld EA, Conkling NA. A prospective analysis of physical examination findings in the diagnosis of facial fractures: Determining predictive value. Plast Surg (Oakv) 2016;24:73-9. [PubMed]
- Cevidanes LH, Bailey LJ, Tucker SF, Styner MA, Mol A, Phillips CL, Proffit WR, Turvey T. Three-dimensional cone-beam computed tomography for assessment of mandibular changes after orthognathic surgery. Am J Orthod Dentofacial Orthop 2007;131:44-50. [Crossref] [PubMed]
- Huang G, Zheng J, Zhang S, Yang C. The value of panoramic radiograph, CT and MRI for the diagnosis of condylar fracture. Zhonghua Kou Qiang Yi Xue Za Zhi 2014;49:434-9. [PubMed]
- Rodt T, Bartling SO, Zajaczek JE, Vafa MA, Kapapa T, Majdani O, Krauss JK, Zumkeller M, Matthies H, Becker H, Kaminsky J. Evaluation of surface and volume rendering in 3D-CT of facial fractures. Dentomaxillofac Radiol 2006;35:227-31. [Crossref] [PubMed]
- Wilson IF, Lokeh A, Benjamin CI, Hilger PA, Hamlar DD, Ondrey FG, Tashjian JH, Thomas W, Schubert W. Prospective comparison of panoramic tomography (zonography) and helical computed tomography in the diagnosis and operative management of mandibular fractures. Plast Reconstr Surg 2001;107:1369-75. [Crossref] [PubMed]
- Ngan DC, Kharbanda OP, Geenty JP, Darendeliler MA. Comparison of radiation levels from computed tomography and conventional dental radiographs. Aust Orthod J 2003;19:67-75. [PubMed]
- Mehta N, Butala P, Bernstein M.. The imaging of Maxillofacial Trauma and its Pertinence to Surgical Intervention. Radiol Clin North Am 2012;50:43-57. [Crossref] [PubMed]
- Napolitano G, Sodano A, Califano L, Grassi R, Brunese L. Multidetector row computed tomography with multiplanar and 3D images in the evaluation of post treatment mandibular fractures. Semin Ultrasound CT MR 2009;30:181-7. [Crossref] [PubMed]
- Horton KM, Sheth S, Corl F, Fishman EK. Multidetector row CT: principles and clinical applications. Crit Rev Comput Tomogr 2002;43:143-81. [PubMed]
- Czerwinski M, Parker WL, Williams HB. Algorithm for head computed tomography imaging in patients with mandible fractures. J Oral Maxillofac Surg 2008;66:2093-7. [Crossref] [PubMed]
- Mukherjee S, Abhinav K, Revington PJ. A review of cervical spine injury associated with maxillofacial trauma at a UK tertiary referral centre. Ann R Coll Surg Engl 2015;97:66-72. [Crossref] [PubMed]
- Chu MW, Soleimani T, Evans TA, Fernandez SI, Spera L, Klene C, Zarzaur BL, Tholpady SS. C-spine injury and mandibular fractures: lifesaver broken in two spots. J Surg Res 2016;206:386-90. [Crossref] [PubMed]
- Singh KS, Jayachandran S. A comparative study on the diagnostic utility of ultrasonography with conventional radiography and computed tomography scan in detection of zygomatic arch and mandibular fractures. Contemp Clin Dent 2014;5:166-9. [Crossref] [PubMed]
- Adeyemo WL, Akadiri OA. A systematic review of the diagnostic role of ultrasonography in maxillofacial fractures. Int J Oral Maxillofac Surg 2011;40:655-61. [Crossref] [PubMed]
- Rama Mohan K, Roa NK, Krishna GL, Kumar VS, Ranganath N, Lakshmi UV. Role of Ultrasonography in Oral and Maxillofacial Surgery: A Review of Literature. J Maxillofac Oral Surg 2015;14:162-70. [Crossref] [PubMed]
- Hirai T, Manders EK, Nagamoto K, Saggers GC. Ultrasonic observation of facial bone fractures: Report of cases. J Oral Maxillofac Surg 1996;54:776-9. [Crossref] [PubMed]
- Emshoff R, Rudisch A, Ennemoser T, Gerhard S. Magnetic resonance imaging findings of temporomandibular joint soft tissue changes in type V and VI condylar injuries. J Oral Maxillofac Surg 2007;65:1550-4. [Crossref] [PubMed]