MR imaging of the traumatic triangular fibrocartilaginous complex tear
Clinical relevance
The triangular fibrocartilage complex (TFCC) serves to stabilize the distal radioulnar joint (DRUJ) by acting as cushion for the ulnar head and lunate during the axial loading of the wrist and ulnar deviation of the wrist (1-3). It also limits ulnar deviation of the carpus (4).
TFCC tear often results from a fall onto outstretched hand which severely increases axial loading or a hyperpronation injury to the forearm (5). TFCC tear usually presents as ulnar-sided wrist pain.
Another clinical manifestation of TFCC injury is DRUJ instability. DRUJ instability can result in audible clicking and pain during rotation of the forearm (6). Usually patients have dorsal subluxation of the ulnar head on extreme hyperpronation due to disruption of the dorsal radioulnar ligament of the TFCC and dorsal DRUJ capsule (4).
Chronic TFCC tear can result in premature degeneration of the ulnocarpal joint or DRUJ with osteophytosis, cartilage loss, subchondral sclerosis, subchondral oedema and cystic change. Chronic ulnar-sided wrist pain and swelling with synovitis usually ensures.
Normal anatomy
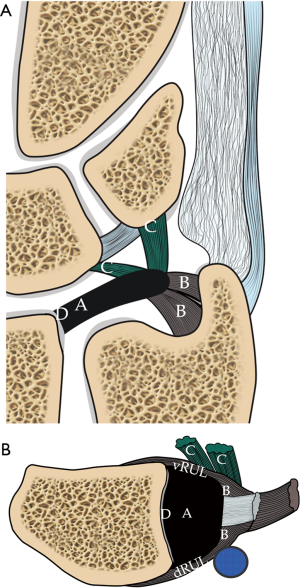
The TFCC is composed of ligament, cartilage and tendon. These include the triangular fibrocartilagous articular disc, volar and dorsal radioulnar ligaments, volar ulnotriquetral and ulnolunate ligaments, ulnar collateral ligament, extensor carpi ulnaris (ECU) tendon sheath and ulnomeniscal homologue (3,7-9).
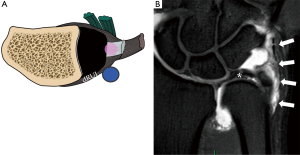
The central component of the TFCC is a triangular fibrocartilage (Figure 1). The ulnar side is broader while the dorsal and volar sides are thicker, giving it a bowtie appearance on sagittal view. It may be fenestrated centrally, especially in elderly due to degeneration. Ulnar positive variant patients have thinner articular discs while the reverse is true for ulnar negative patients making them more or less prone to tendon degeneration and tears respectively (10).
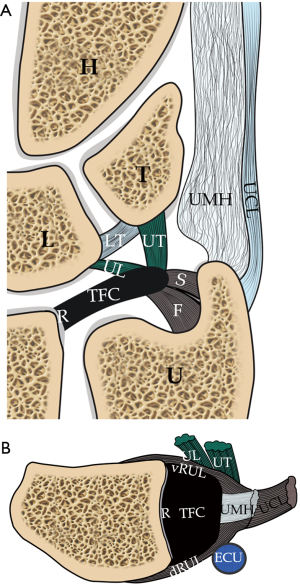
On the volar side, the triangular fibrocartilage merges completely with the volar radioulnar ligament which is reinforced by the ulnotriquetral and ulnolunate ligaments (Figure 1). These insert onto the volar aspect of the lunate and triquetrum respectively, forming the anterior band of the triquetral sling (11).
On the dorsal side, the triangular fibrocartilage merges with the dorsal radioulnar ligament which is reinforced by the dorsal radiotriquetral ligament (dorsal radiocarpal ligament) forming the posterior band of the triquetral sling (Figure 1). Since the volar and dorsal radioulnar ligament are so closely integrated with the articular disc, some authors consider this as simply thick, strong marginal portions of the disc composed of lamellar collagen (4).
At the ulnar side, the triangular fibrocartilage is attached to the inner side of the ulnar styloid process (just proximal to the ulnar tip) by a distal lamina and ulnar fovea by a proximal lamina (Figure 1). The disc is broader at this region. The tissue in between the two laminae is loose, though highly vascularized, areolar tissue named the ligamentum subcruentum.
At the ulno-dorsal aspect of the TFCC, the triangular fibrocartilage is reinforced by meniscal homologue which is situated in between the ulna and triquetrum (Figure 1). It has a common origin with the dorsal radioulnar ligament on the ulno-dorsal corner of the radius (12) and inserts on the ulnar border of triquetrum and 5th metacarpal base.
Some of TFCC fibres are also reinforced by ECU tendon sheath (13). The ECU is situated within the ulnar notch and surrounded by its synovial sheath and the investing fascia of the wrist (4). They are further reinforced by the ulnar collateral ligament which blends with the ECU tendon sheath. It is noteworthy that there is no prominent ulnar collateral ligament demonstrable on MR imaging (4,14) and the existence of this as an isolated structure has been challenged (15).
On the radial side, the triangular fibrocartilage is attached to the articular cartilage covering the ulnar side of the distal radius (Figure 1).
The ulnar side of the articular disc and its supporting structures are supplied by the ulnar and anterior interosseous arteries (16). The central and radial aspects of the disc are relatively avascular and comprise of chondrocytes in a fibrocartilaginous matrix, helping to explain why central and radial tear of the triangular fibrocartilage do not heal well if repaired (17).
MRI technique
For the intrinsic small and thin structures of the TFCC, high field MR scanner e.g., 3 Tesla MR scanner is ideally used to acquire a high spatial, high contrast imaging data (1,18).
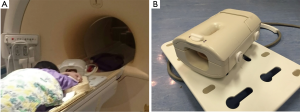
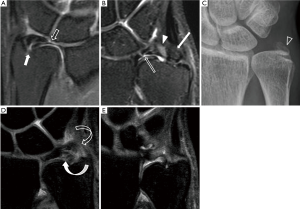
The ‘superman position’ with the hand raised up and above the head can allow the wrist to be scanned in the isocenter of the magnetic field, which is more homogeneous. The wrist in this position will be slightly semipronated (Figure 2A). The wrist should ideally be scanned in a dedicated eight-channel wrist coil (Figure 2B) which will enable acquisition of high resolution imaging data to more clearly depict the small structures of the TFCC.
Multiple different pulse sequences can be used for imaging the TFCC including spin echo and fat-suppression sequences (1). In our centre, we use high resolution proton density coronal with fat and non-fat suppression sequences, sagittal T2W fat-suppression sequence and axial proton-density fat suppression sequences. Three orthogonal planes are acquired allowing good correlation with each other.
Proton density sequences with or without fat suppression can detect intradiscal degeneration. A tear is seen as fluid signal filling an abnormal anatomical gap on T2W fat suppressed sequences.
3D gradient echo sequences allow the acquisition of thin contiguous sections 1mm or less through the TFCC (19) and no interslice gap. A recent study showed that punctate calcifications within the disc indicating degeneration were best depicted on the 3D gradient echoes sequence (20). Quantitative MRI such as T1 rho to look for changes of mechanical properties of TFCC is still under research.
Although the sensitivity and specificity of MR arthrography is overall unquestionably slightly better than non-arthrographic MR imaging, in most instances it is not necessary to perform an MR arthrogram to adequately assess the structures of the TFCC. Whether or not to undertake MR arthrography should consider local expertise, time and cost efficiency, patient comfort, and clinical need. The vast majority of surgically relevant pathology will be visible on a non-arthrographic MR study, especially nowadays with higher resolution data acquisition. Minor perforations and small tears may be missed on non-arthrographic studies though the relevance of these relatively minor injuries with respect to surgical decision making is highly questionable in most patients (3). In our institution, we perform MR arthrography for younger patients, particularly if they are athletic and/or considered good surgical candidates, or if they have unexplained ulnar wrist symptoms with a prior relatively normal non-arthrographic MR study of the wrist. MR arthrography risks contamination of soft tissue detail by contrast extravasation, does not allow one to appreciate joint effusion and seems to lessen the depiction of mild ulnocarpal synovitis.
MR arthrography can be indirect or direct (21-22). Direct arthrography is performed using ultrasound or fluoroscopic guidance (23) (Figure 3). We prefer to use ultrasound approach primarily for its superior real time capability. Though a limitation can be leakage of contrast from one wrist compartment to the other due to a communicating tear which cannot be seen during the injection.
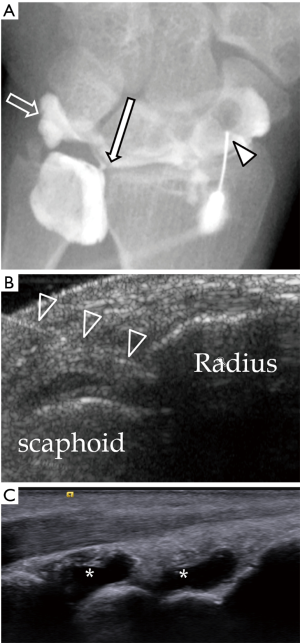
Both ultrasound and flurosocopic guidance are from the dorsal side because it is more superficial with less intervening crucial anatomical structures.
Usually contrast injected into the radiocarpal joint is enough to delineate any communicating tear. Contrast will fill the gap of the tear allowing clear depiction by MRI. If there is a full thickness tear of the articular disc, the DRUJ will also distend and the proximal surface of the triangular fibrocartilage will be delineated by contrast. However, if there is not full-thickness communicating tear, then injection of contrast into the DRUJ is necessary. If only the radiocarpal joint is injected, one may overlook a partial thickness tear along the proximal surface of triangular fibrocartilage or a tear of the proximal lamina attaching to the ulnar fovea.
In ulnotriquetral and ulnolunate ligament tears, there is no inter-compartment communication and thus there is only capsular leakage of contrast material evident on arthrogram or MR arthrogram after contrast is injected into either the DRUJ or radiocarpal joint (24).
Indirect arthrography is possible since intravenous contrast will diffuse into the joint space after about 20 minutes. The more synovitis is present, the more likelihood of contrast accumulation within the joint fluid. Schweitzer et al. and Herold et al. showed this method to have a higher accuracy at depicting tears of the TFCC (21,22). However, no communication from one compartment to another can be demonstrated compared to real time screening of contrast injection under fluoroscopy.
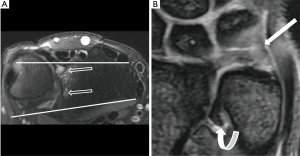
MR imaging of the TFCC can also be performed with or without traction. The wrist traction device was set up with the finger traps applied to the index and ring fingers and connected to a preselected weight (7 kg for men and 5 kg for women) by a nonelastic cord. The cord is routed over the edge of the MRI gantry table. Traction is better following direct MR arthrography since this removes the vacuum effect pulling opposing bone surfaces together. Traction is still possible, nevertheless, without prior direct arthrography though the degree of distraction achieved is less. Traction helps further improve the depiction of TFCC, and intrinsic ligament tears as well as articular cartilage surface during MR imaging of the wrist. The current likely hierarchy of techniques for wrist imaging with respect to depiction of tears and articular cartilage surface is suggested (Figure 4).
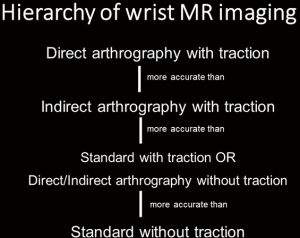
High resolution standard (i.e., non-arthrographic) MR imaging of the wrist without traction is highly accurate in the depiction of most TFCC pathology, particularly with regard to determining whether surgery is necessary or not, and this is by far the most widely used approach for high quality wrist imaging in most clinical settings. The non-standard approaches (direct/indirect arthrography, traction) have been shown to add significant benefit in overall accuracy though their use should be reserved for pre-determined selected clinical cases.
Normal appearances of TFCC
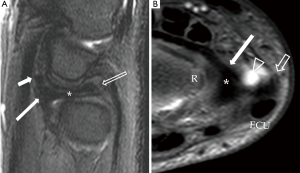
The central component of TFCC is a disc which is composed of fibrocartilage and shows homogeneous low signal intensity on spin-echo images (25) (Figures 5,6). Slightly increased in signal intensity on short TE sequences is related to mucoid degeneration, seen most commonly in elderly patients.
The triangular fibrocartilage disc is biconcave bowtie in appearance on coronal views, discoid on sagittal and triangular on axial images. It is thicker on the dorsal and volar sides.
The thickness of the triangular fibrocartilage disc depends on the degree of ulnar variance (6). In the ulnar negative wrist, triangular fibrocartilage disc appears thick and short and lies horizontal. In the ulnar positive wrist, it appears thin and elongated and lies in a more vertical orientation. A thin triangular fibrocartilage disc is more vulnerable to tear.
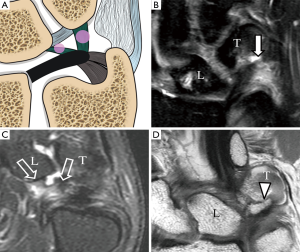
The proximal and distal laminae appear striated in appearance, less homogeneous and low in signal on all sequences (Figures 5,6). The ligamentum subcruentum appears as a higher signal intensity on T1 and T2-weighted images in between the laminae (4). On the radial side, the triangular fibrocartilage is attached the cartilage rim of the distal radius which is a high signal on PD or T2W images.
Ulnomeniscal homologue is fat signal on MRI and lies just ulnar to the prestyloid recess (26). It is best seen on coronal imaging (Figure 5B).
The dorsal and ulnar radioulnar ligaments are most easily discerned on sagittal images (Figure 6). These are striated in appearance and represent the thickest part of the margin of the triangular fibrocartilage. They are homogeneous, of slightly higher signal intensity and are not easily separated from the triangular fibrocartilage (4).
The ulnotriquetral and ulnolunate ligament show homogeneous low signal intensity. They can be identified on coronal and sagittal images by tracing them from the triangular fibrocartilage to the lunate and triquetral bones on consecutive slices (24) (Figures 5,6).
Types of TFCC tears
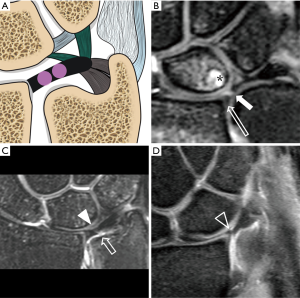
According to Palmer’s classification, the TFCC tear is divided into traumatic (type 1) or degenerative (type 2) tear. Degenerative tear is not discussed in this manuscript which primarily focuses on traumatic tears. Traumatic tears are divided into A to D (Figure 7).
- 1A tear is at the central or paracentral region of the triangular fibrocartilage. It is usually situated at the paracentral region, ~2–4 mm from the radial attachment;
- 1B is avulsion tear at the ulnar attachment with or without an ulnar styloid fracture. The tear is either at the ulnar styloid process attachment or the foveal attachment;
- 1C is avulsion tear at the distal attachment at the lunate or triquetrum i.e., the ulnolunate and ulnotriquetral ligament with or without avulsion fracture;
- 1D is avulsion tear at the radial attachment with or without distal radial fracture.
The type of treatment is mainly dependent on the blood supply. For 1A tear, since this part of the articular disc is avascular, no repair can be done and only debridement is performed. For 1B and 1C tears, the area of tear is vascularized and surgical repair can obtain good result. The current trend is to repair the TFCC under arthroscopy (27,28). For 1D tear, there are various ways to repair, depending on any associated ligament tear and DRUJ instability. In some cases, ulnar shortening osteotomy or arthroscopic wafer ulnar resection will be performed for relieving the axial load and stress on the TFCC.
Limitations of palmar classification
This classification has its limitations. The TFCC tear at the volar/dorsal radioulnar ligaments are not categorized under Palmer’s classification (29). Type 1B tear have not been further subclassified as tears of the foveal attachment, ulnomeniscal homologue, ulnar collateral ligament or ECU subsheath. Thirdly, there is no further differentiation into the full thickness or partial thickness tear or into different tear configuration, e.g., flap, horizontal tear (5,29). Finally, combined tear is not included which is not uncommon. Abe et al. found that there were 32 combined tears in 173 wrists (18.5%) (29).
MRI features of TFCC tear
Tear is defined as fluid signal intensity extending through the disc or ligament on fluid sensitive sequences, including proton density, T2-weighted or gradient echoes sequences (30). The tear can be a radial tear or named as slit-like radial or vertical appearance i.e., parallel to the rim of the distal radius or it can be horizontal in appearance. Combined tear or complex tear is not uncommon which include two components.
Palmer 1A tear is common. A slit tear at the central and paracentral region of the triangular fibrocartilage (Figure 8). The tear can be partial-thickness tear or full-thickness tear. Partial thickness tear only involves one articular surface, usually the proximal surface. MR arthrography of the DRUJ is good to depict this often subtle tear.
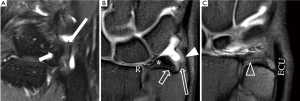
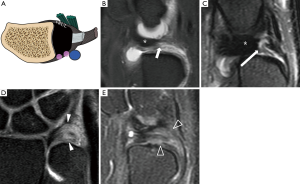
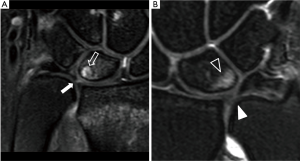
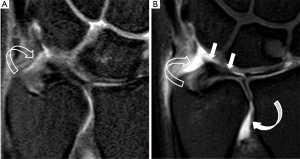
Palmer 1B tear is an avulsion of either the proximal or distal lamina (Figure 9). This peripheral tear is the most commonly missed. Indirect clues include altered morphology, excessive fluid accumulation and focal synovitis around this region (31). MR arthrography of the DRUJ will also help to depict tears at the foveal attachment.
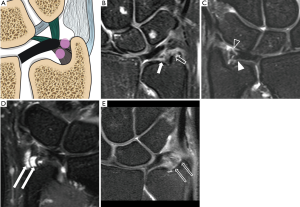
Ulnar detachment can be associated with avulsion fracture at the base of the styloid process (32,33) (Figure 10). Non-united styloid fracture in chronic TFCC tear with DRUJ instability is not uncommon.

Other secondary signs include the extension of fluid along the medial border of distal ulna, avulsive cystic changes or bone marrow oedema of the ulnar styloid process and fovea, and fascial oedema and fluid (3).
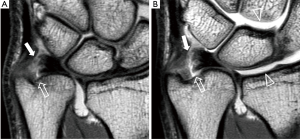
Palmer 1C tear is avulsion tear at the distal attachments of the lunate or triquetral bone (Figure 11). Tears of the UTL and ULL are usually intrasubstance tears with oedema and thickening rather than fibre discontinuity. The normal UTL and ULL are sometimes lax and slightly increased signal (2) on short TE sequence. If abnormal signal is seen within the ligaments on fluid-sensitive sequences, then a tear is likely (34).
Palmer 1D tear is avulsion tear at the radial attachment ± distal radial sigmoid fracture (Figure 12). Palmer 1D tear is either avulsion tear of the TFCC or avulsion fracture at the radial rim. When there is a tear at the radial side, it is important to look for any remnant attaching to the radial rim. If there is a small remnant present, it is termed a type 1A rather than 1D tear (4).
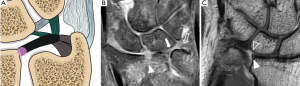
As mentioned in the previous paragraphs, the TFCC tear can be found at the dorsal radioulnar ligament (Figure 13), at the volar side (Figure 14) or at the ulnomeniscal homologue (Figure 15) which are not under the classification of Palmer’s classification. Some of tears are atypical in tear configuration or in combination (Figure 16).

Since some of the TFCC tears will result in DRUJ instability (1B to 1D) (29,35), the congruity of the ulnar head within the sigmoid notch will be disrupted, causing dorsal or volar subluxation. Dorsal instability is more common. A lateral radiograph or a CT scan can be used to confirm dorsal subluxation in neutral position (36). Mild dorsal subluxation may only manifest on pronation and volar subluxation on supination. For detailed evaluation, a CT scan performed in the neutral, pronation and supination positions is helpful. Usually both wrists are examined simultaneously as some individuals simply have undue physiological laxity and in this instance a comparable degree of laxity will be apparent on both sides. Chronic instability of DRUJ will predispose DRUJ degenerative change (Figure 17).
An ulnar positive variant is more frequently seen in patients with TFCC tear because this leads to developmental thinning of the articular disc with increase in force borne by the distal portion of the ulna (37). Ulnocarpal impaction may also be seen in these patients as evident by cartilage thinning or focal cartilage loss at the ulnar proximal aspect of the lunate (Figure 18), associated lunate bone oedema and attrition tears of the luno-triquetral ligament.
It is difficult to differentiate between degenerative and traumatic tears. The features favouring degenerative tears include diffuse thinning of the triangular fibrocartilage, ulnar positive variant, site of tear closer to the radial attachment. Both types of tear frequently co-exist.
Accuracy of MRI in TFCC tear detection
Plain MRI scan
Standard MRI can achieve high performance in detection of the TFCC tear. In a recent study, Zlatkin et al. found that the sensitivity, specificity and accuracy was 92%, 89% and 91% respectively (4). Johnstone and coworkers et al. also found that the sensitivity and specificity was 90% and 70% respectively (38). Haims et al. found that synovitis can be used as a marker for ulnar-sided tear (31) though the sensitivity and specificity are not high, which was 42% and 63% respectively. Oneson et al. found that sensitivity and specificity of radial slit-like tear was 100% and 86% though diagnosis of ulnar-sided tear was not so high (39).
Potter et al. have tried to use 3D-gradient echoes thin slices to improve the diagnosis of TFCC tear showing how MRI could achieve sensitivity and specificity up to 100% and 90% respectively (19).
MR arthrography
MRA was considered better than standard MR to depict central and peripheral tears with sensitivity and specificity more than 90% (40-43) (Figure 19).
Rarely, false negative diagnoses may occur for communicating tear when scar and fibrosis block the flow of contrast through the defect (44).
Herold et al. studied 45 patients and found that MR arthrogram using an indirect arthrogram method is better to detect TFCC defect with a sensitivity, specificity and accuracy of indirect arthrography were 100%, 77% and 93% respectively (22). Schweitzer et al. also found that MR arthrogram could achieve 100% accuracy though the sample size is small (21). However, some authors found that there is no significant difference when compared to non-enhanced MRI scan (45).
Multi-detector computed tomography (MDCT) arthrography
MDCT arthrography was advocated as an alternative to MR arthrography for its better resolution but its potential benefit is still controversial (23,46,47).
MR wrist with traction
Recently, MR wrist traction was proven to have significantly improved the visibility and detection of TFCC tears. The accuracy of TFCC tear has increased from 83% to 98% (48) (Figure 20). MR with traction is well tolerated and does not increase the examination time too much as almost all the preparation work is completed before entering the scanning room (48).
Pitfalls of MRI in TFCC tear detection
Mucoid degeneration will render the TFCC high signal intensity on short TE sequence, i.e., T1-weighted and proton-density sequences simulating tears (49). This alteration in signal intensity reflects alteration in the water binding property of the TFCC disk (50).
The most difficult area for detection of TFCC tears is the peripheral tear at the ulnar side, at the ulnar styloid and foveal attachements, especially for low field MRI studies (39). Haims et al. found that the sensitivity, specificity and accuracy of detection of peripheral ulnar tear were only 17%, 79% and 64% only (31).
The ligamentum subcruentum is loose areolar tissue situated between the proximal and distal laminae. It appears intermediate or slightly high T2W or proton density signal and this can mimic a tear in this region (51,52).
The attachment of the TFCC at the radial articular cartilage, which appears hyperintense on proton and T2W sequences, can also mimic a tear (52) but is easy to recognize once you are aware of this pitfall. Peripheral and undersurface tears of the triangular fibrocartilage can be obscured by synovitis (4). MR arthrogram is useful to differentiate a tear or synovitis if it cannot be differentiated by plain MRI.
Conclusions
MRI imaging is extremely helpful in revealing the normal anatomy and injury to the TFCC. Nowadays, with high or medium-field strength MR systems, high accuracy can be achieved in detecting and characterizing the specific type of injury present. Good quality MR imaging acquisition is a pre-requisite as it allows careful interpretation of the TFCC by a radiologist familiar with the normal MR anatomy of the TFCC as well as the likely injuries that can occur. In most instances, a standard high-resolution MR examination will suffice. Though in particular clinical settings, such as in professional athletes, MR arthrography and traction will help to maximize accuracy in those situations where doubt still exists after standard MR imaging.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Yu JS, Habib PA. Normal MR imaging anatomy of the wrist and hand. Radiol Clin North Am 2006;44:569-81. [Crossref] [PubMed]
- Davis KW, Blankenbaker DG. Imaging the ligaments and tendons of the wrist. Semin Roentgenol 2010;45:194-217. [Crossref] [PubMed]
- Chhabra A, Soldatos T, Thawait GK, Del Grande F, Thakkar RS, Means KR Jr, Carrino JA. Current perspectives on the advantages of 3-T MR imaging of the wrist. Radiographics 2012;32:879-96. [Crossref] [PubMed]
- Zlatkin MB, Rosner J. MR imaging of ligaments and triangular fibrocartilage complex of the wrist. Radiol Clin North Am 2006;44:595-623. [Crossref] [PubMed]
- Watanabe A, Souza F, Vezeridis PS, Blazar P, Yoshioka H. Ulnar-sided wrist pain. II. Clinical imaging and treatment. Skeletal Radiol 2010;39:837-57. [Crossref] [PubMed]
- Vezeridis PS, Yoshioka H, Han R, Blazar P. Ulnar-sided wrist pain. Part I: anatomy and physical examination. Skeletal Radiol 2010;39:733-45. [Crossref] [PubMed]
- Nakamura T, Makita A. The proximal ligamentous component of the triangular fibrocartilage complex. J Hand Surg Br 2000;25:479-86. [PubMed]
- Golimbu CN, Firooznia H, Melone CP Jr, Rafii M, Weinreb J, Leber C. Tears of the triangular fibrocartilage of the wrist: MR imaging. Radiology 1989;173:731-3. [Crossref] [PubMed]
- Yoshioka H, Ueno T, Tanaka T, Shindo M, Itai Y.. High-resolution MR imaging of triangular fibrocartilage complex (TFCC): comparison of microscopy coils and a conventional small surface coil. Skeletal Radiol 2003;32:575-81. [Crossref] [PubMed]
- Palmer AK, Glisson RR, Werner FW. Relationship between ulnar variance and triangular fibrocartilage complex thickness. J Hand Surg Am 1984;9:681-2. [Crossref] [PubMed]
- Smith DK. Volar carpal ligaments of the wrist: normal appearance on multiplanar reconstructions of three-dimensional Fourier transform MR imaging. AJR Am J Roentgenol 1993;161:353-7. [Crossref] [PubMed]
- Taleisnik J.. The ligaments of the wrist. J Hand Surg Am. 1976;1:110-8. [Crossref] [PubMed]
- Prendergast N, Rauschning W. Normal anatomy of the hand and wrist. Magn Reson Imaging Clin N Am 1995;3:197-212. [PubMed]
- Theumann NH, Pfirrmann CW, Antonio GE, Chung CB, Gilula LA, Trudell DJ, Resnick D. Extrinsic carpal ligaments: normal MR arthrographic appearance in cadavers. Radiology 2003;226:171-9. [Crossref] [PubMed]
- Taleisnik J, Gelberman RH, Miller BW, Szabo RM. The extensor retinaculum of the wrist. J Hand Surg Am 1984;9:495-501. [Crossref] [PubMed]
- Berquist TH. Anatomy. In: Berquist TH, editor. MRI of the hand and wrist. Philadelphia: Lippincoott Williams & Wilkins; 2003:1-32.
- Thiru RG, Ferlic DC, Clayton ML, McClure DC. Arterial anatomy of the triangular fibrocartilage of the wrist and its surgical significance. J Hand Surg Am 1986;11:258-63. [Crossref] [PubMed]
- Saupe N, Prüssmann KP, Luechinger R, Bösiger P, Marincek B, Weishaupt D. MR imaging of the wrist: comparison between 1.5- and 3-T MR imaging--preliminary experience. Radiology 2005;234:256-64. [Crossref] [PubMed]
- Potter HG, Asnis-Ernberg L, Weiland AJ, Hotchkiss RN, Peterson MG, McCormack RR Jr. The utility of high-resolution magnetic resonance imaging in the evaluation of the triangular fibrocartilage complex of the wrist. J Bone Joint Surg Am 1997;79:1675-84. [Crossref] [PubMed]
- Bae WC, Ruangchaijatuporn T, Chang EY, Biswas R, Du J, Statum S, Chung CB. MR morphology of triangular fibrocartilage complex: correlation with quantitative MR and biomechanical properties. Skeletal Radiol 2016;45:447-54. [Crossref] [PubMed]
- Schweitzer ME, Natale P, Winalski CS, Culp R. Indirect wrist MR arthrography: the effects of passive motion versus active exercise. Skeletal Radiol 2000;29:10-4. [Crossref] [PubMed]
- Herold T, Lenhart M, Held P, Babel M, Ruf S, Feuerbach S, Link J., Indirect MR. Arthrography of the wrist in the diagnosis of TFCC-Lesions. Rofo 2001;173:1006-11. [Crossref] [PubMed]
- Lee RK, Ng AW, Tong CS, Griffith JF, Tse WL, Wong C, Ho PC. Intrinsic ligament and triangular fibrocartilage complex tears of the wrist: comparison of MDCT arthrography, conventional 3-T MRI, and MR arthrography. Skeletal Radiol 2013;42:1277-85. [Crossref] [PubMed]
- Resnick DL, Kang HS, Pretterklieber ML. Wrist and Hand. In: Internal derangements of Joints. 2nd edition. Saunders 2006:1218-418.
- Sofka CM, Potter HG. Magnetic resonance imaging of the wrist. Semin Musculoskelet Radiol 2001;5:217-26. [Crossref] [PubMed]
- Buck FM, Gheno R, Nico MA, Haghighi P, Trudell DJ, Resnick D. Ulnomeniscal homologue of the wrist: correlation of anatomic and MR imaging findings. Radiology 2009;253:771-9. [Crossref] [PubMed]
- Tse WL, Lau SW, Wong WY, Cheng HS, Chow CS, Ho PC, Hung LK. Arthroscopic reconstruction of triangular fibrocartilage complex (TFCC) with tendon graft for chronic DRUJ instability. Injury 2013;44:386-90. [Crossref] [PubMed]
- Estrella EP, Hung LK, Ho PC, Tse WL. Arthroscopic repair of triangular fibrocartilage complex tears. Arthroscopy 2007;23:729-37. [Crossref] [PubMed]
- Abe Y, Tominaga Y, Yoshida K. Various patterns of traumatic triangular fibrocartilage complex tear. Hand Surg 2012;17:191-8. [Crossref] [PubMed]
- Zlatkin MB, Chao PC, Osterman AL, Schnall MD, Dalinka MK, Kressel HY. Chronic wrist pain: evaluation with high-resolution MR imaging. Radiology 1989;173:723-9. [Crossref] [PubMed]
- Haims AH, Schweitzer ME, Morrison WB, Deely D, Lange R, Osterman AL, Bednar JM, Taras JS, Culp RW. Limitations of MR imaging in the diagnosis of peripheral tears of the triangular fibrocartilage of the wrist. AJR Am J Roentgenol 2002;178:419-22. [Crossref] [PubMed]
- Corso SJ, Savoie FH, Geissler WB, Whipple TL, Jiminez W, Jenkins N. Arthroscopic repair of peripheral avulsions of the triangular fibrocartilage complex of the wrist: a multicenter study. Arthroscopy 1997;13:78-84. [Crossref] [PubMed]
- Hauck RM, Skahen J 3rd, Palmer AK. Classification and treatment of ulnar styloid nonunion. J Hand Surg Am 1996;21:418-22. [Crossref] [PubMed]
- Totterman SM, Miller RJ. MR imaging of the triangular fibrocartilage complex. Magn Reson Imaging Clin N Am 1995;3:213-28. [PubMed]
- Amrami KK, Felmlee JP. 3-Tesla imaging of the wrist and hand: techniques and applications. Semin Musculoskelet Radiol 2008;12:223-37. [Crossref] [PubMed]
- Mino DE, Palmer AK, Levinsohn EM. The role of radiography and computerized tomography in the diagnosis of subluxation and dislocation of the distal radioulnar joint. J Hand Surg Am 1983;8:23-31. [Crossref] [PubMed]
- Cerezal L, del Piñal F, Abascal F, García-Valtuille R, Pereda T, Canga A. Imaging findings in ulnar-sided wrist impaction syndromes. Radiographics 2002;22:105-21. [Crossref] [PubMed]
- Johnstone DJ, Thorogood S, Smith WH, Scott TD. A comparison of magnetic resonance imaging and arthroscopy in the investigation of chronic wrist pain. J Hand Surg Br 1997;22:714-8. [Crossref] [PubMed]
- Oneson SR, Scales LM, Timins ME, Erickson SJ, Chamoy L. MR imaging interpretation of the Palmer classification of triangular fibrocartilage complex lesions. Radiographics 1996;16:97-106. [Crossref] [PubMed]
- Lee YH, Choi YR, Kim S, Song HT, Suh JS. Intrinsic ligament and triangular fibrocartilage complex (TFCC) tears of the wrist: comparison of isovolumetric 3D-THRIVE sequence MR arthrography and conventional MR image at 3 T. Magn Reson Imaging 2013;31:221-6. [Crossref] [PubMed]
- Schweitzer ME, Brahme SK, Hodler J, Hanker GJ, Lynch TP, Flannigan BD, Godzik CA, Resnick D. Chronic wrist pain: spin-echo and short tau inversion recovery MR imaging and conventional and MR arthrography. Radiology 1992;182:205-11. Erratum in: Radiology 1992;184:583. [Crossref] [PubMed]
- Zanetti M, Bräm J, Hodler J. Triangular fibrocartilage and intercarpal ligaments of the wrist: does MR arthrography improve standard MRI? J Magn Reson Imaging 1997;7:590-4. [Crossref] [PubMed]
- Scheck RJ, Romagnolo A, Hierner R, Pfluger T, Wilhelm K, Hahn K. The carpal ligaments in MR arthrography of the wrist: correlation with standard MRI and wristarthroscopy. J Magn Reson Imaging 1999;9:468-74. [Crossref] [PubMed]
- Kirschenbaum D, Sieler S, Solonick D, Loeb DM, Cody RP. Arthrography of the wrist. Assessment of the integrity of the ligaments in young asymptomatic adults. J Bone Joint Surg Am 1995;77:1207-9. [Crossref] [PubMed]
- Haims AH, Schweitzer ME, Morrison WB, Deely D, Lange RC, Osterman AL, Bednar JM, Taras JS, Culp RW. Internal derangement of the wrist: indirect MR arthrography versus unenhanced MR imaging. Radiology 2003;227:701-7. [Crossref] [PubMed]
- Moser T, Khoury V, Harris PG, Bureau NJ, Cardinal E, Dosch JC. MDCT arthrography or MR arthrography for imaging the wrist joint? Semin Musculoskelet Radiol 2009;13:39-54. [Crossref] [PubMed]
- Moser T, Dosch JC, Moussaoui A, Dietemann JL. Wrist ligament tears: evaluation of MRI and combined MDCT and MR arthrography. AJR Am J Roentgenol 2007;188:1278-86. [Crossref] [PubMed]
- Lee RK, Griffith JF, Ng AW, Nung RC, Yeung DK. Wrist Traction During MR Arthrography Improves Detection of Triangular Fibrocartilage Complex and Intrinsic Ligament Tears and Visibility of Articular Cartilage. AJR Am J Roentgenol 2016;206:155-61. [Crossref] [PubMed]
- Kang HS, Kindynis P, Brahme SK, Resnick D, Haghighi P, Haller J, Sartoris DJ. Triangular fibrocartilage and intercarpal ligaments of the wrist: MR imaging. Cadaveric study with gross pathologic and histologic correlation. Radiology 1991;181:401-4. [Crossref] [PubMed]
- Steinbach LS, Smith DK. MRI of the wrist. Clin Imaging 2000;24:298-322. [Crossref] [PubMed]
- Timins ME, Jahnke JP, Krah SF, Erickson SJ, Carrera GF. MR imaging of the major carpal stabilizing ligaments: normal anatomy and clinical examples. Radiographics 1995;15:575-87. [Crossref] [PubMed]
- Burns JE, Tanaka T, Ueno T, Nakamura T, Yoshioka H. Pitfalls that may mimic injuries of the triangular fibrocartilage and proximal intrinsic wrist ligaments at MR imaging. Radiographics 2011;31:63-78. [Crossref] [PubMed]


