
Computed tomography of an air-inflated resected lung is useful for verifying the intraoperative findings of complete resection in a reduction operation
The incidence of sublobar resection for small, indistinct pulmonary nodules is increasing because of the increased frequency of performing computed tomography (CT)-based whole-lung screening. Various techniques for the intraoperative localization of such indistinct lesions [e.g., confirmation by VALMAP (1) or palpation (2)] have been reported. In addition, we use intraoperative cone-beam CT to perform partial resection of small lesions (3). In this method, a clip is placed in the vicinity of the tumor, CT is performed, and the tumor is resected.
However, these are merely methods of marking lesions and do not guarantee complete resection. Complete resection is ensured by confirming the presence of the lesion within the resected specimen with adequate surgical margins. Sublobar resection that fails to provide adequate surgical margins carries a risk of local recurrence (4).
Surgical margins for complete resection are usually determined based on the final pathology results after surgery. However, surgeons cannot complete the operation with confidence if they cannot assess the completeness of resection during the procedure itself. It is difficult to incise a resected specimen with a scalpel in order to identify the tumor and surgical margin because directing scalpel insertion for small lesions is difficult, and surgical margins are not always correctly evaluated at the incision line. Furthermore, such attempts further damage the specimen and affect the final pathology results. A method that allows lesions and surgical margins to be identified without damaging the resected specimen is therefore desirable.
We previously reported the performance of intraoperative CT of a resected lung inflated with air to verify the surgical margin (5). Specifically, puncture was performed at a distant site where the pulmonary lesion was absent using a 23-G puncture needle connected to an appropriately sized syringe. Instillation was performed slowly in order to prevent destruction of the alveolar wall. The amount of air injected into the resected lung should ideally be such that the pleura on the surface of the resected lung is fully stretched by slowly injecting air. When air has been injected successfully, you will feel resistance to the syringe. This CT image allows for the intraoperative verification of the lesion and surgical margin from multiple angles without damaging the resected specimen.
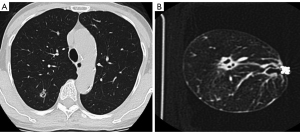
We performed our novel technique in 12 patients who underwent thoracoscopic pulmonary wedge resection for metastatic lung cancer with pure solid or primary lung cancer with ground-glass attenuation. The lesions were reproducibly confirmed to be the same size and morphology on preoperative and intraoperative CT of the resected specimen (Figure 1A,1B). However, the surgical margin on intraoperative CT apparently shrank after formalin fixation among overall patients (84.6%±6.8% of the intraoperative values, n=12). Thus, the pathologically determined surgical margin should be distinguished from the intraoperatively measured surgical margin, which occurs due to shrinkage of the lung tissue caused by formalin. This information can be useful if understood before surgery.
This novel method is associated with some difficulty, as inflation must be performed slowly and over time until the pleura is firmly and fully stretched. If the resected specimen is inflated quickly, the alveolar structure breaks down, and a clear CT image cannot be obtained. Ideally, after inflation, CT should be performed quickly before air leaks out. It takes about 10 minutes until the specimen is transported to the CT room and the CT images can actually be reviewed; this time can be shortened if you can cooperate with the radiologist.
In our previous validation study, we evaluated only wedge resection cases; however, this method may also be adapted for use in segmentectomy. It was newly confirmed that the use of automatic suture for the segment surface can be applied in the same way as wedge resection. However, in segmentectomy—where the segment surface is created using an electrocautery scalpel—air leakage after the specimen is inflated is a concern. This can be managed by applying glue or other products that will not affect the pathology results to the separation surface or by attaching a sheet to the surface. This is considered to be a simple and useful method of evaluating the completeness of resection during surgery. Even if the preoperatively planned surgical margin cannot be secured, this method will allow staple lines with an insufficient surgical margin to be identified and will aid in the performance of additional resection.
Complete resection during reduction surgery can be achieved by ingenious marking the tumor, and intraoperative confirmation can be performed with this method.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was a standard submission to the journal. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-22-1149/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sato M. Precise sublobar lung resection for small pulmonary nodules: localization and beyond. Gen Thorac Cardiovasc Surg 2020;68:684-91. [Crossref] [PubMed]
- Ichinose J, Mun M, Matsuura Y, Nakao M, Okumura S. Efficiency of thoracoscopic palpation in localizing small pulmonary nodules. Surg Today 2019;49:921-6. [Crossref] [PubMed]
- Ueda K, Aoki M, Kamimura G, Imamura N, Tokunaga T, Suzuki S, Sato M. Intraoperative cone-beam computed tomography to secure the surgical margin in pulmonary wedge resection for indistinct intrapulmonary lesions. JTCVS Tech 2022;13:219-28. [Crossref] [PubMed]
- Sawabata N, Ohta M, Matsumura A, Nakagawa K, Hirano H, Maeda H, Matsuda HThoracic Surgery Study Group of Osaka University. Optimal distance of malignant negative margin in excision of nonsmall cell lung cancer: a multicenter prospective study. Ann Thorac Surg 2004;77:415-20. [Crossref] [PubMed]
- Kamimura G, Ueda K, Suzuki S, Maeda K, Hakamada H, Sato M. Intraoperative computed tomography of a resected lung inflated with air to verify safety surgical margin. Quant Imaging Med Surg 2022;12:1281-9. [Crossref] [PubMed]


