
A cross-calibration study using a novel dual X-ray absorptiometry system for bone mineral density measurements with the European Spine Phantom
Introduction
Osteoporosis is one of the most common bone metabolism diseases. It is associated with decreased bone mass and trabecular thinning, which leads to increased bone fragility and gradually resulting in bone fractures (1-4). Zeng et al. (5) reported an osteoporosis prevalence of 29.1% in older women and 6.5% in older men aged >50 years, equating to an estimated population-wide prevalence of 49.3 million and 10.9 million people, respectively. The fragility fracture is the major complication of osteoporosis and is responsible for increased morbidity, mortality, and medical costs. Detecting changes in bone density early and accurately is particularly critical. Dual-energy X-ray absorptiometry (DEXA) is the most commonly used equipment to measure bone mineral density (BMD) for identifying the risk of osteoporosis (6). For DEXA, short-term precision (CV%) and phantom-based accuracy studies are among the most important routine quality control (QC) procedures (7). Furthermore, compared with quantitative computed tomography (CT), DEXA has a low radiation dose and is readily available (3,8-11).
The SONIALVISION SMIT is a fluoroscopic imaging system capable of DEXA using the smart BMD application. Compared to other DEXA implements, the SONIALVISION SMIT includes several notable updates (12). First, this DEXA apparatus contains a novel reference database (Japanese women) that is different from the young adult (age 20–39 years) BMD values for Chinese and White US populations at the spinal and femur skeletal sites. Second, the movement of the examination table and the tube can be adjusted by the console and the buttons beside the examination table so that it can be set quickly to the starting position of the bone densitometer. Furthermore, it is possible to perform simpler and more reproducible positioning by confirming the imaging range using the field light and the low-dose fluoroscopy function. Finally, due to the short scanning time of only about 10 seconds, the risk of patient movement is low, reducing the need for repeated scans.
Significant differences have been observed in bone density measurements achieved using densitometers from different vendors compared to when using different models from the same vendor. Hence, the International Society for Clinical Densitometry (ISCD) recommends that any hardware upgrade or replacement of an old DEXA system by the same or different vendor should be preceded by cross-calibration of the DEXA, especially for implementations of the DEXA systems such as the SONIALVISION SMIT.
It is well known that the clinical routine includes calibration of the DEXA systems only with a manufacturer’s phantom for daily QC, making it necessary to verify the reliability of BMD measurements in human participants. In this study, we carried out cross-calibration between the SMIT, Discovery A, and Lunar iDXA for BMD measurements of an anthropomorphic European Spine Phantom (ESP) (4,13). Furthermore, we transformed BMD measurements made with the Discovery A and Lunar iDXA to SMIT measurements to allow for consistent assessment of bone density across the DEXA measurement systems.
In this study, BMD measurement with SONIALVISION SMIT has shown good short-term precision in the lumbar spine. Compared with the Discovery A or iDXA, small but significant differences in BMD have been observed at the lumbar spine, and cross-calibration equations may be required for the spine. This suggests that a follow-up study should be performed using novel DEXA equipment because of the longitudinal stability over time of the SMIT, or an investigation into interoperator measurement precision with increased experience using the SMIT should be conducted. Therefore, this study aimed to establish cross-calibration equations and verify the SONIALVISION SMIT via the cross-calibration of different DEXA scans.
Methods
Phantom
An anthropomorphic ESP (QRM GmbH, Möhrendorf, Germany) consists of water-equivalent resin containing 3 vertebral inserts with different BMD quantities. The BMD was defined as the amount of calcium hydroxyapatite (HA) per volume unit of bone. When measured on DEXA, these lumbar spine vertebral inserts (L1–3) represent an areal bone mineral density (aBMD) of 0.5 (osteoporosis), 1.0 (osteopenia), and 1.5 g/cm2 (normal bone mass) HA (14). The International DEXA Standardization Committee recommended the ESP as a possible standard for use in DEXA (15).
BMD measurement
The BMD measurements using Smart BMD software (version 01.13.03; Shimadzu, Kyoto, Japan) of the SONIALVISION SMIT system (Shimadzu, Kyoto, Japan), the Discovery A Pencil Beam DEXA scanner (software version 13.5.3.3; Hologic Inc., Bedford, MA, USA), and the Lunar iDXA Fan Beam DEXA scanner with a 64-channel detector (software version encore 16; GE Healthcare, Chicago, IL, USA). All scans were performed by the same operator to decrease the potential introduction of interoperator differences.
Imaging protocols
The 3 DEXA scanners used a linear X-ray fan beam with switched-pulse dual-energy (100/140 kVp) and a multielement detector array. The standard mode was used for measurements. The scan times were 10, 10, and 47 seconds with an exposure of 0.62, 0.04, and 0.146 mGy for the lumbar spine scans, respectively.
Study design
The ESP (ESP-145) was placed on the scanner table and aligned along the long axis of the table, as shown in Figure 1. To minimize the potential operator bias, all scans on the 3 devices were performed by the same examiner. ESP was carefully scanned 10 times with repositioning to calculate the short-term precision error [coefficients of variation, CV% = (SD/mean) ×100%] of the equipment. Linear regression equations were applied to cross-calibrate the Discovery A and iDXA to the SMIT in terms of the densitometric standards in the ESP with BMD value. This study was approved by the local institutional review board (No. 2021-KY-1222-002).
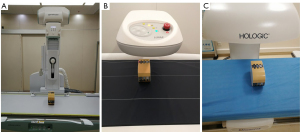
Image analysis
For analysis, a rectangular region of interest (ROI) was automatically drawn over each vertebral of ESP to segment the bone region and quantify the aBMD in g/cm2. However, all BMD analyses were thoroughly checked for random measurement errors (i.e., ROI errors, metal artifacts, and misidentification of the vertebral body) and were manually corrected if needed. In this study, the QC procedures on the phantom were carried out according to the manufacturer’s recommendations.
Statistical analysis
Data analysis was performed using GraphPad Prism version 8.0 for Windows (GraphPad Software Inc., La Jolla, CA, USA). The data were checked for normality using a Shapiro-Wilk test and are presented as the mean and SD. The Welch test in a one-way analysis of variance (ANOVA) with a post-hoc Tamhane T2 test was used to analyze the difference in ESP BMD measurements with the SMIT, Discovery A, and Lunar iDXA.
By constructing linear regression models around the ESP measurements by SMIT, Discovery A, and Lunar iDXA, we generated equations for BMD cross-calibration with each of the instruments. The statistical quality of the model was evaluated by the appropriate statistical term and standard error of the estimate (SEE). The multiple regression models were assessed using correlation (r) and SEE. A Bland-Altman analysis plotted the average of the 2 measurements on the x-axis and the difference between them on the y-axis. To help identify statistical population trends, the mean and 95% confidence intervals (CIs) were overlaid on the plot. The Bland-Altman method was applied to evaluate the bias among the 3 devices. A two-tailed P value <0.05 was considered statistically significant.
Results
As shown in Figure 2, the boxplot analysis indicated that the data did not include any outliers. The data in each group followed a normal distribution according to the Shapiro-Wilk test (P>0.05). There were statistically significant differences in L1 (Welch F=4.896; P=0.023), L2 (Welch F=447.9; P<0.0001), and L3 (Welch F=1,621; P<0.0001) among the different devices. The ESP scans indicated that SMIT BMD value measured 0.8% higher (P=0.696), 7.2% higher (P<0.0001), and 1.1% lower (P=0.201) than did the Discovery A in L1, L2, and L3, respectively. The SMIT BMD value also measured 3.5% higher (P=0.019), 7.4% lower (P<0.0001), and 25.6% lower (P<0.0001) than did the Lunar iDXA in the L1, L2, and L3, respectively (Table 1). The CV% of the phantom BMD value was slightly higher when measured with the SMIT (1.901–2.264%) than with the Discovery A (0.695–0.958%) or Lunar iDXA (1.278–1.366%).

Table 1
| Vertebra | BMD, ESP-145 (g/cm2) |
BMD | ||
|---|---|---|---|---|
| SMIT | Discovery A | Lunar iDXA | ||
| L1 | 0.5 | |||
| Mean (SD) (g/cm2) | 0.526 (0.010)a | 0.522 (0.005)a | 0.508 (0.015)a | |
| CV% | 1.901 | 0.958 | 0.958 | |
| L2 | 1.0 | |||
| Mean (SD) (g/cm2) | 1.016 (0.023)b | 0.947 (0.007)b | 1.098 (0.015)b | |
| CV% | 2.264 | 0.739 | 1.366 | |
| L3 | 1.5 | |||
| Mean (SD) (g/cm2) | 1.281 (0.021)c | 1.295 (0.009)c | 1.721 (0.022)c | |
| CV% | 1.639 | 0.695 | 1.278 | |
a,b,c, one-way ANOVA between the SMIT, Discovery A, and Lunar iDXA in the L1, L2, and L3, respectively (P<0.05). ANOVA, analysis of variance; SMIT, SONIALVISION SMIT; iDXA, Lunar iDXA; BMD, bone mineral density; ESP-145, European Spine Phantom no.1 45; SD, standard deviation; CV, coefficients of variation.
As shown in Table 2, the cross-calibration equations indicated r ranging from 0.933 to 0.984 and SEE ranging from 0.004 to 0.008 for the L1-3 on the different devices (P<0.0001).
Table 2
| Vertebra | Equation | r | SEE | P |
|---|---|---|---|---|
| L1 | BMD SMIT =1.881 × Discovery A − 0.457 | 0.941 | 0.004 | <0.0001 |
| BMD SMIT =0.604 × Lunar iDXA + 0.219 | 0.933 | 0.004 | <0.0001 | |
| L2 | BMD SMIT =3.276 × Discovery A − 2.087 | 0.948 | 0.008 | <0.0001 |
| BMD SMIT =1.534 × Lunar iDXA − 0.668 | 0.984 | 0.004 | <0.0001 | |
| L3 | BMD SMIT =2.170 × Discovery A − 1.529 | 0.945 | 0.007 | <0.0001 |
| BMD SMIT =0.906 × Lunar iDXA − 0.278 | 0.941 | 0.007 | <0.0001 |
BMD, bone mineral density; SEE, standard error of the estimate; ESP, European Spine Phantom; SMIT, SONIALVISION SMIT; iDXA, Lunar iDXA.
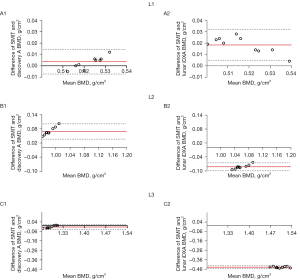
Bland-Altman analysis revealed good agreement between the SMIT and Discovery A or Lunar iDXA for BMD measurement at the L1-3 (Figure 3). Almost all data points were within the 95% limits of agreement of the ESP BMD measurements.
Discussion
The QC of BMD measurements is essential to maintaining consistency and mainly involves the inspection of equipment and assessment of the radiographer’s expertise. The QC process of a device includes both the short-term daily QC and the long-term dynamic QC (16,17). Daily QC involves inspecting the device condition every day using the manufacturer’s device-specified phantom. However, changes in the BMD value should be followed-up by a general phantom, such as the ESP. Zemel et al. (18) reported that most hospitals do not know where their machine falls within the range of intermachine variability, which may affect the diagnosis of bone-threatening conditions in patients. Based on the ESP BMD measurements, this paper highlighted the systematic differences between the SMIT, Discovery A, and Lunar iDXA devices (P<0.0001). Zemel et al. (18) reported that the coefficient of variation of aBMD values was 1.8% in different clinical centers. Patel et al. (19) reported that the CV% for different generations of Hologic scanners varied from 0.7% to 1.34% for the lumbar spine. Similar to the findings of a previous study (20), the CV% of the BMD value was slightly higher when measured with the SMIT (1.901–2.264%) than with the Discovery A (0.695–0.958%) and Lunar iDXA (0.278–1.366%). The ISCD recommends correction equations be used if the difference between 2 densitometers exceeds 1% (21). In this paper, the CV% of all BMD values with the SMIT were beyond 1% (1.901–2.264%); therefore, calibration should be carried out again to set the difference within 1%. Kim et al. (22) reported that the quantitative comparison of 3 devices should be carried out via cross-calibration. In this study, cross-calibration was carried out by a single radiologic technologist. This study aimed to establish cross-calibration equations and verify the SMIT by cross-calibration with different DEXA scans. The BMD of the ESP was measured using the existing (Discovery A and Lunar iDXA) and replaced (SMIT) devices 10 times each to obtain the mean BMD values.
Saarelainen et al. (20) reported that the iDXA showed higher values than did the Lunar Prodigy at high BMD values, whereas the opposite was found at low BMD values. Similar to a previous study, the iDXA-measured BMD values in L1, L2, and L3 were 3.5% (0.018 g/cm2) lower, 7.4% (0.082 g/cm2) higher, and 25.6% (0.44 g/cm2) higher than those measured with the SMIT in this paper. Reid et al. (23) reported that Hologic scanners tended to underestimate the nominal BMD, while Lunar scanners overestimated this value. Similar to a previous study, the Discovery A-measured BMD values in the L1, L2, and L3 were 0.8% (0.004 g/cm2) lower, 7.2% (0.069 g/cm2) lower, and 1.1% (0.014 g/cm2) higher than those measured using the SMIT in this paper. This study indicated that the SMIT and Discovery A tended to be lower at high BMD values compared to the Lunar iDXA. The ISCD recommends that phantom-based cross-calibration system from different devices is essential after replacement of the DEXA. To obtain more accurate measurements, individual calibration equations were derived for each machine in previous studies (4,5,24). Similar to the findings of Genant et al. (4), the correlation of the patients’ spinal BMD values was excellent for each of the 3 scanner pairs. In this study, the regression models of the ESP measurements for the SMIT showed a strong positive correlation with the BMD values (vs. Discovery A, r=0.941–0.948; vs. iDXA, r=0.933–0.984). However, the regression slope and intercept were different, demonstrating the need for cross-calibration. For different DEXA devices, individual calibration equations were found to be necessary to fit the observed values with the given densities (25). Cross-calibration also decreased the systematic errors between the 3 instruments.
Hind et al. reported that Bland-Altman analyses on BMD values showed small but significant positive biases at the lumbar spine (0.005) (26). The Bland-Altman analysis conducted by Choi et al. (27) showed good agreement between the Prodigy and iDXA. Krueger et al. (28) reported that the lumbar spine BMD was highly correlated with a correlation coefficient (R2) of 0.98. Additionally, Bland-Altman analysis demonstrated an aBMD bias of –0.003 g/cm2, confirming equipment similarity. In this paper, Bland-Altman analyses showed small biases in the BMD measurements (g/cm2) of the ESP (SMIT vs. Discovery A range –0.014 to 0.069; SMIT vs. iDXA range –0.440 to 0.018), which were comparable with those reported by previous studies. The Bland-Altman results also indicated that cross-calibration equations may be required at this site.
The increasing incidence of osteoporosis and fractures partly reflects the rapid aging of China’s population (3). In the Asian esophageal cancer belt, most of the published findings on esophageal cancer risk factors have come from Chinese studies (29-31). In China, gastric cancer is the main malignancy of the digestive tract, which seriously threatens the health of Chinese people (32). In this study, the novel DEXA is suitable for older adults who have gastrointestinal disease indications and can be used to perform BMD screening during the gastrointestinal examination. This study showed that cross-calibration is essential, especially novel DEXA equipment is used to measure BMD. This is particularly beneficial for long-term follow-up epidemiological studies on osteoporosis and multisite equipment studies based on bone densitometry.
This study had several limitations that should be noted. First, we only considered 1 operator and only collected the scans in 1 session. In real-world clinical practice, different technicians perform the inspections. Therefore, an assessment of the technician’s operating error is required. The DXA technologist precision assessments, least significant change (LSC) calculations, and recommended precision thresholds were derived from the Adult Official Positions of the ISCD (as updated in 2019). Second, human participants were not included in this study. We appreciated it not only focus directly on BMD measures but also on osteoporosis diagnosis. In this study, only BMD measures were studied through ESP.
In conclusion, a strong agreement for BMD measurement was established between the 3 DEXA systems. Cross-calibration equations for lumbar spine BMD values need to be applied to transform the Hologic Discovery A or GE Lunar iDXA measurements into SONIALVISION SMIT measurements, so as to comply with ISCD standards for patient continuity of care in assessment during clinical diagnosis.
Acknowledgments
Funding: This study was supported by the grants from the Special Plan 2022 for Introducing Foreign Intelligence with Henan Province (No. HNGD2022033).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-22-619/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was approved by the local institutional review board (No. 2021-KY-1222-002).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Chen P, Li Z, Hu Y. Prevalence of osteoporosis in China: a meta-analysis and systematic review. BMC Public Health 2016;16:1039. [Crossref] [PubMed]
- Guo Z, Du X, Wang L, Li K, Jiao J, Guglielmi G, Zhurakivska K, Lo Muzio L, Blake GM, Cheng X. Measurements of volumetric bone mineral density in the mandible do not predict spinal osteoporosis. Dentomaxillofac Radiol 2020;49:20190280. [Crossref] [PubMed]
- Cheng X, Zhao K, Zha X, Du X, Li Y, Chen S, et al. Opportunistic Screening Using Low-Dose CT and the Prevalence of Osteoporosis in China: A Nationwide, Multicenter Study. J Bone Miner Res 2021;36:427-35. [Crossref] [PubMed]
- Genant HK, Grampp S, Glüer CC, Faulkner KG, Jergas M, Engelke K, Hagiwara S, Van Kuijk C. Universal standardization for dual x-ray absorptiometry: patient and phantom cross-calibration results. J Bone Miner Res 1994;9:1503-14. [Crossref] [PubMed]
- Zeng Q, Li N, Wang Q, Feng J, Sun D, Zhang Q, Huang J, Wen Q, Hu R, Wang L, Ma Y, Fu X, Dong S, Cheng X. The Prevalence of Osteoporosis in China, a Nationwide, Multicenter DXA Survey. J Bone Miner Res 2019;34:1789-97. [Crossref] [PubMed]
- Jankowski LG, Warner S, Gaither K, Lenchik L, Fan B, Lu Y, Shepherd J. Cross-calibration, Least Significant Change and Quality Assurance in Multiple Dual-Energy X-ray Absorptiometry Scanner Environments: 2019 ISCD Official Position. J Clin Densitom 2019;22:472-83. [Crossref] [PubMed]
- Frimeth J, Galiano E, Webster D. Some physical and clinical factors influencing the measurement of precision error, least significant change, and bone mineral density in dual-energy x-ray absorptiometry. J Clin Densitom 2010;13:29-35. [Crossref] [PubMed]
- Li X, Li X, Li J, Jiao X, Jia X, Zhang X, Fan G, Yang J, Guo J. The accuracy of bone mineral density measurement using dual-energy spectral CT and quantitative CT: a comparative phantom study. Clin Radiol 2020;75:320.e9-320.e15. [Crossref] [PubMed]
- Zhao Y, Li K, Duanmu Y, Wang L, Xu X, Zhang Y, Tang J, Zhang Y, Li Z, Hind K, Blake GM, Cheng X. Accuracy, Linearity and Precision of Spine QCT vBMD Phantom Measurements for Different Brands of CT Scanner: A Multicentre Study. J Clin Densitom 2022;25:34-42. [Crossref] [PubMed]
- Cheng X, Yuan H, Cheng J, Weng X, Xu H, Gao J, Huang M, Wáng YXJ, Wu Y, Xu W, Liu L, Liu H, Huang C, Jin Z, Tian W. Chinese expert consensus on the diagnosis of osteoporosis by imaging and bone mineral density. Quant Imaging Med Surg 2020;10:2066-77. [Crossref] [PubMed]
- Woisetschläger M, Hägg M, Spångeus A. Computed tomography-based opportunistic osteoporosis assessment: a comparison of two software applications for lumbar vertebral volumetric bone mineral density measurements. Quant Imaging Med Surg 2021;11:1333-42. [Crossref] [PubMed]
- Takemoto T, Oguchi T, Oda K. Comparison of novel DXA system, Shimazu SONIALVISION G4, with GE-Lunar PRODIGY. J Bone Miner Metab 2021;39:1041-7. [Crossref] [PubMed]
- Pearson D, Cawte SA, Green DJ. A comparison of phantoms for cross-calibration of lumbar spine DXA. Osteoporos Int 2002;13:948-54. [Crossref] [PubMed]
- Wu Y, Jiang Y, Han X, Wang M, Gao J. Application of low-tube current with iterative model reconstruction on Philips Brilliance iCT Elite FHD in the accuracy of spinal QCT using a European spine phantom. Quant Imaging Med Surg 2018;8:32-8. [Crossref] [PubMed]
- Kalender WA, Felsenberg D, Genant HK, Fischer M, Dequeker J, Reeve J. The European Spine Phantom--a tool for standardization and quality control in spinal bone mineral measurements by DXA and QCT. Eur J Radiol 1995;20:83-92. [Crossref] [PubMed]
- Faulkner KG, McClung MR. Quality control of DXA instruments in multicenter trials. Osteoporos Int 1995;5:218-27. [Crossref] [PubMed]
- Blunt BA, Jones D, Svensen RK, Hans DB, Feinblatt JD, Genant HK. Good clinical practice and audits for dual X-ray absorptiometry and X-ray imaging laboratories and quality assurance centers involved in clinical drug trials, private practice, and research. J Clin Densitom 1998;1:323-37. [Crossref] [PubMed]
- Zemel BS, Wasserman H, Kelly A, Fan B, Shepherd J, Lappe J, Gilsanz V, Oberfield S, Winer KK, Kalkwarf HJ. Intermachine differences in DXA measurements vary by skeletal site, and impact the assessment of low bone density in children. Bone 2020;141:115581. [Crossref] [PubMed]
- Patel R, Blake GM, Rymer J, et al. Long-term precision of DXA scanning assessed over seven years in forty postmenopausal women. Osteoporos Int 2000;11:68-75. [Crossref] [PubMed]
- Saarelainen J, Hakulinen M, Rikkonen T, Kröger H, Tuppurainen M, Koivumaa-Honkanen H, Honkanen R, Hujo M, Jurvelin JS. Cross-Calibration of GE Healthcare Lunar Prodigy and iDXA Dual-Energy X-Ray Densitometers for Bone Mineral Measurements. J Osteoporos 2016;2016:1424582. [Crossref] [PubMed]
- Shepherd JA, Lu Y, Wilson K, Fuerst T, Genant H, Hangartner TN, Wilson C, Hans D, Leib ES. Cross-calibration and minimum precision standards for dual-energy X-ray absorptiometry: the 2005 ISCD Official Positions. J Clin Densitom 2006;9:31-6. [Crossref] [PubMed]
- Kim HS, Yang SO. Quality Control of DXA System and Precision Test of Radio-technologists. J Bone Metab 2014;21:2-7. [Crossref] [PubMed]
- Reid DM, Mackay I, Wilkinson S, Miller C, Schuette DG, Compston J, Cooper C, Duncan E, Galwey N, Keen R, Langdahl B, McLellan A, Pols H, Uitterlinden A, O'Riordan J, Wass JA, Ralston SH, Bennett ST. Cross-calibration of dual-energy X-ray densitometers for a large, multi-center genetic study of osteoporosis. Osteoporos Int 2006;17:125-32. [Crossref] [PubMed]
- Yu W, Zhang Z, Pan W, Guan W, Lin Q, Xia W, Li T, Hsieh E. Comparison of Differences in Bone Mineral Density Measurement With 3 Hologic Dual-Energy X-Ray Absorptiometry Scan Modes. J Clin Densitom 2021;24:645-50. [Crossref] [PubMed]
- Watson LPE, Venables MC, Murgatroyd PR. An Investigation Into the Differences in Bone Density and Body Composition Measurements Between 2 GE Lunar Densitometers and Their Comparison to a 4-Component Model. J Clin Densitom 2017;20:498-506. [Crossref] [PubMed]
- Hind K, Cooper W, Oldroyd B, Davies A, Rhodes L. A cross-calibration study of the GE-Lunar iDXA and prodigy for the assessment of lumbar spine and total hip bone parameters via three statistical methods. J Clin Densitom 2015;18:86-92. [Crossref] [PubMed]
- Choi YJ, Lee BJ, Lim HC, Chung YS. Cross-calibration of iDXA and Prodigy on spine and femur scans in Korean adults. J Clin Densitom 2009;12:450-5. [Crossref] [PubMed]
- Krueger D, Vallarta-Ast N, Checovich M, Gemar D, Binkley N. BMD measurement and precision: a comparison of GE Lunar Prodigy and iDXA densitometers. J Clin Densitom 2012;15:21-5. [Crossref] [PubMed]
- The global, regional, and national burden of oesophageal cancer and its attributable risk factors in 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol 2020;5:582-97. [Crossref] [PubMed]
- Wang LD, Zhou FY, Li XM, Sun LD, Song X, Jin Y, et al. Genome-wide association study of esophageal squamous cell carcinoma in Chinese subjects identifies susceptibility loci at PLCE1 and C20orf54. Nat Genet 2010;42:759-63. [Crossref] [PubMed]
- He J, Chen WQ, Li ZS, Li N, Ren JS, Tian JH, Tian WJ, Hu FL, Peng JExpert Group of China Guideline for the Screening, Early Detection and Early Treatment of Esophageal Cancer. Work Group of China Guideline for the Screening, Early Detection and Early Treatment of Esophageal Cancer. China guideline for the screening, early detection and early treatment of esophageal cancer (2022, Beijing). Zhonghua Zhong Liu Za Zhi 2022;44:491-522. [PubMed]
- He J, Chen WQ, Li ZS, Li N, Ren JS, Tian JH, Tian WJ, Hu FL, Peng JExpert Group of China Guideline for the Screening, Early Detection and Early Treatment of Gastric Cancer. Working Group of China Guideline for the Screening, Early Detection and Early Treatment of Gastric Cancer. China guideline for the screening, early detection and early treatment of gastric cancer (2022, Beijing). Zhonghua Zhong Liu Za Zhi 2022;44:634-66. [PubMed]


