
Benign fibrous histocytoma of femur: a case report
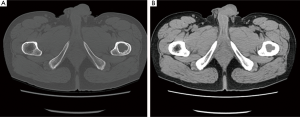
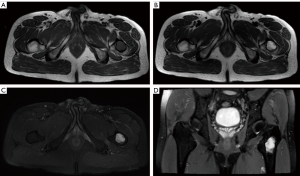
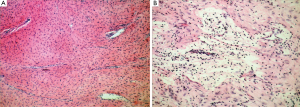
A 43-year-old man presented with dull pain of his left inguinal region for one month. His medical history and laboratory examination were unremarkable. Radiography revealed an oval unilocular radiolucent lesion in the left proximal femur with marginal sclerosis (Figure 1). CT scan and three-dimensional reconstruction of left hip joint demonstrated a slightly lobulated osteolytic lesion in the left femur, measured 2.6 cm × 2.6 cm × 4.5 cm, demarcated with an integrated sclerosis ring (Figure 2A). The lesion appeared homogeneous soft-tissue density similar to that of the skeletal muscle (Figure 2B). MRI showed that the lesion was isointense on T1WI (Figure 3A), heterogeneous hyperintense on both T2WI and fat-saturated T2WI, with hypointense ring in circumference on both T1WI and T2WI (Figure 3B,C,D). A bone cyst or BFH was suspected. The intrabony lesion was carefully and completely curetted by the orthopedic surgeon and the defect was thereafter filled with bone grafts. It was a yellowish-white solid mass on gross examination. Histologically, the mass was consisted of spindle-shaped cells arranged in a whorled or storiform pattern and scattered histiocytic cells were noted among the spindle cells (Figure 4A,B). From these findings, the final diagnosis of BFH was established.

Acknowledgements
Disclosure: The authors declare no conflict of interest.


