
Correlation between direction of pedicle screw and restoration of lumbar degenerative scoliosis in degenerative lumbar spondylolisthesis: a retrospective study
Introduction
Degenerative lumbar spondylolisthesis (DLS) is defined as the slippage of a lumbar vertebra over the subjacent vertebra without a disruption of the pars interarticularis. Loss of disc height and reduced segmental lordosis in DLS is linked to intervertebral disc degeneration (1). Lumbar degenerative scoliosis, which occurs in DLS, also mainly results from degenerative changes of the intervertebral disc, the pathological process of which involves changes of asymmetric intervertebral space that related to vertebral rotation and/or lateral translation in the spondylolisthesis segment (2-4). According to the classification of lumbar Cobb angle in lumbar degenerative scoliosis (Cobb angle ≥10° or ≤20°), about 20.8% of patients with DLS have lumbar degenerative scoliosis (5,6). Prior surgical approaches have focused on correcting sagittal alignment, but coronal degenerative changes of lumbar degenerative scoliosis in the spondylolisthesis segment have received little attention clinically (7-9). Lumbar degenerative scoliosis with a disc wedging angle more than 3° and lateral translation has been reported to have a higher reoperation rate and inferior clinical outcomes in patients receiving decompression-only surgery (6,10).
Surgical pedicle screws can be used to correct lumbar alignment. An upper pedicle screw in transforaminal lumbar interbody fusion (TLIF) surgery inserted at a slight downward angle to the lower endplate in single-segment fusion facilitates the restoration of sagittal alignment, and the direct vertebral rotation technique achieves correction of the coronal curve through forces exerted on the pedicle screw in the direction opposite to the coronal curve (11-13). With high stiffness and strength, pedicle screws perform well in correcting both sagittal alignment in patients with DLS and coronal alignment in patients with scoliosis (14). Although TLIF is a common technique for patients with DLS, the effect of TLIF on patients with DLS and lumbar degenerative scoliosis remains uncertain.
Surgeons have endeavored to investigate the cost-effective improvement of the surgical technique in the treatment of patients with DLS. To our knowledge, the direction of the upper and lower pedicle screws in single-level unilateral TLIF had not been studied from the perspective above. Accordingly, our preliminary study aimed to determine the correlation between the direction of the pedicle screw and the restoration of lumbar degenerative scoliosis, which may optimize the surgical intervention. We hypothesized that significant improvement could be achieved both radiographically and clinically in patients with DLS with lumbar degenerative scoliosis undergoing single-level unilateral TLIF. Moreover, we speculated that intraoperative adjustment of the direction of the upper and/or lower pedicle screws would be associated with the correction of lumbar degenerative scoliosis. We present the following article in accordance with the STROBE reporting checklist (available at https://qims.amegroups.com/article/view/10.21037/qims-22-483/rc).
Methods
Study design and consent
This retrospective cohort study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the ethics board of Tongji Hospital of Tongji University (No. K-2017-008), and individual consent for this retrospective analysis was waived.
Patient population
Medical information from the electronic medical records at the spine department in Shanghai Tongji hospital were screened for patients’ information from July 1, 2015, to April 30, 2021 (this study was based on complete patients’ information that had been recorded before the beginning of the study).
The inclusion criteria were the following: (I) single-level unilateral TLIF for the diagnosis of DLS with lumbar degenerative scoliosis (Cobb angle ≥10° or ≤20°, along with disc wedging angle >3°, and/or lateral translation >0 mm), (II) age ≥18 and ≤75 years, (III) available complete clinical and radiographic data, and (IV) follow-up of at least 1 year.
Meanwhile, the exclusion criteria were the following: (I) conditions with a history of spinal surgery, retrolisthesis, spinal tumor, spinal fracture; (II) receiving multiple segmental and/or bilateral operation and experiencing failure of internal fixation and a second operation; (III) accompanied by severe osteoporosis, severe degeneration of the adjacent intervertebral disc (Pfirrmann V), or unequal leg length exerting obvious influence on the lumbar degenerative scoliosis.
Patients’ demographic and clinical information including age, body mass index (BMI), sex ratio, spondylolisthesis segment, operative time, blood loss, complications, fusion rate, and follow-up were collected.
Surgical intervention
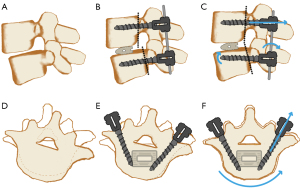
Single-level unilateral TLIF and posterior pedicle screw and rod instrumentation were performed in all patients. After general anesthesia and placement of the hips in a fully extended, prone position, a C-arm was used to identify the spondylolisthesis segment. After local disinfection, a posterior midline incision was made. The paraspinal muscles were dissected to expose the posterior column of the segment. Unilateral laminectomy and partial facetectomy were conducted in the symptomatic side; the disc was then exposed and removed following the protection of the thecal sac and nerve root by a cotton pad. A model tester cage was inserted into intervertebral space to gradually distract the space and test the cage size. The insertion of the first 2 polyaxial pedicle screws was achieved in the side contralateral to the decompression side. The entry point of the 2 pedicle screws was selected as the intersection between the isthmic crest and the accessory process crest of the vertebra. Pedicle screws were inserted into the vertebrae along the direction of pedicle, and the sagittal angle was adjusted within the vertebral arch as requested. The parallel direction was achieved by placing the pedicle screw parallel to the pedicle, the cranial direction was achieved by placing the pedicle screw toward the upper endplate but not destroying the cortical bone of pedicle, and the caudad direction was achieved by placing the pedicle screw toward the lower endplate without destruction of the cortical bone. Then, the lower pedicle screw was prefixed on the prebent titanium rod, and the upper pedicle screw was preliminarily lifted for primary reduction while the distance between upper and lower pedicle screw was distracted and maintained. The prebent titanium rod was held as perpendicular as possible to the screw rod to ensure that the screw head was parallel to the screw rod. A parallel surface between the screw head and screw rod has been shown to have a higher pull-out stiffness compared with an angled position (15). Preparation of the endplate was then performed carefully, and a cage filled with crushed bone from the removed lamina and facet joint was subsequently inserted into the intervertebral space through the symptomatic side. Preparation of the endplate and the cage filled with crushed bone was implemented to promote better postoperative intervertebral fusion. The other 2 polyaxial pedicle screws were inserted into the pedicle ipsilateral to the decompression side and tied with a prebent titanium rod in the same manner as described previously. Both upper pedicle screws were then lifted simultaneously for further reduction of the spondylolisthesis vertebra, which was followed by further tightening between the set screw and screw rod of the lower polyaxial pedicle screws. Finally, axial compression was applied to all 4 polyaxial pedicle screws to secure the cage and fusion construct, and the set screws were tightened.
Radiographic and clinical evaluations
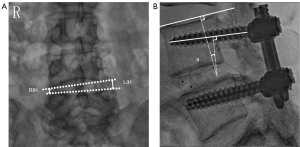
Radiographic and clinical data of the included patients were gathered and analyzed preoperatively, postoperatively, and at the final follow-up. Radiographs of anterior–posterior and lateral lumbar images were obtained, which included sagittal parameters (13), including Taillard index, average intervertebral height (AIH), slip angle (SA), lumbar lordosis (LL), sacral slope (SS), and coronal parameters (5,16), as well as Cobb angle, disc wedging angle (DWA), lateral translation, degree of vertebral rotation (DVR), direction of lateral curve (DLC), and left and right intervertebral height (LIH, RIH) (Figure 1A). Coronal asymmetric intervertebral space was demonstrated by the intervertebral height difference (IHD) between the medial and lateral margin of the indexed intersegmental space (IHD:|RIH-LIH|) (17). Implant parameters included the angle of the upper/lower pedicle screws (Figure 1B), and the horizontal position of cage (%, normalized to endplate size) (18).
Radiographic measurements were performed on X-ray images using a custom-written MATLAB program (MathWorks, Natick, MA, USA) (18). Intraclass correlation coefficient (ICC) was used to evaluate the consistency of pedicle screw-related complications and segmental fusion based on computed tomography (CT) 1 year after surgery between 2 visits. If the findings were inconsistent, a further evaluation was reached by group discussion.
Clinical outcomes were assessed using the visual analog scale for back pain (VAS-BP), VAS for leg pain (VAS-LP), and Oswestry disability index (ODI).
Statistical analysis
Data analysis was conducted using SPSS software (version 21.0; IBM Corp., Armonk, NY, USA). Continuous data that conformed to a normal distribution (Shapiro-Wilk normality test) are presented as mean ± standard deviation (SD); otherwise, data are presented as median [25% interquartile range (IQR), 75% IQR]. Postoperative and final follow-up clinical and radiographic data were compared with preoperative values using Dunnett test of analysis of variance, whereas the comparison of DVR was performed using Kruskal-Wallis test. The preliminary correlation between ΔIHD (postoperative IHD – preoperative IHD) and relevant factors, including ΔLL (postoperative LL – preoperative LL), ΔDVR (postoperative DVR – preoperative DVR), preoperative Cobb angle, preoperative DWA, preoperative DLC, angle of upper and lower pedicle screws, and the horizontal position of the cage was analyzed by univariable linear regression analysis.
All factors with a P value <0.1 were selected and entered simultaneously into the multivariable linear regression analysis to reveal the independent factors related to ΔIHD. The indirect effect of independent variables on ΔIHD was evaluated using mediation analysis. Specifically, we developed a mediation model by controlling covariates and using the Hayes PROCESS v2.16.3, Model 4 with 5,000 bootstrap resamples in SPSS (19). For all tests, a bilateral P value <0.05 was deemed to be statistically significant.
Results
Demographic outcomes
A total of 57 patients (21 men, 36 women; 63.33±9.21 years of age; BMI 25.14±3.38 kg/m2) were followed up for 15.16±3.09 months. Among the 57 patients, 48 had L4 spondylolisthesis, 8 had L5 spondylolisthesis, and 1 had L3 spondylolisthesis. The operative time and amount of blood loss were 207.54±51.17 min and 227.19±169.85 mL, respectively. The fusion rate was 80.70% (46/57). Complications occurred in 15 patients in total, with no patients undergoing reoperation during the follow-up. The ICC was 0.837 [95% confidence interval (CI): 0.738–0.901], and there was no need for group discussion (Table 1).
Table 1
| Characteristic | N=57 |
|---|---|
| Age, years | 63.33±9.21 |
| BMI, kg/m2 | 25.14±3.38 |
| Sex ratio (M:F) | 21:36 |
| Spondylolisthesis segment | |
| L3 | 1 |
| L4 | 48 |
| L5 | 8 |
| Operative time, min | 207.54±51.17 |
| Blood loss, mL | 227.19±169.85 |
| Complications, n | |
| Neural injury | 1 |
| Dural tear | 1 |
| Screw loosening | 13 |
| Fusion rate, % | 80.70 (46/57) |
| Follow-up, months | 15.16±3.09 |
Data are presented as mean ± SD or number. SD, standard deviation; BMI, body mass index; M, male; F, female.
Clinical outcomes
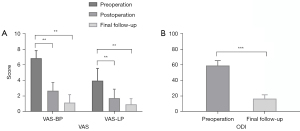
The preoperative VAS-BP and VAS-LP scores of patients were 6.86±0.97 and 3.98±1.57, respectively, the postoperative scores were lower at 2.70±1.05 and 1.75±1.15, respectively (P=0.006 and P=0.003), and the final follow-up scores were 1.18±1.02 and 0.96±0.73, respectively (P=0.001 and P=0.002; Figure 2). The ODI scores of patients reduced from 59.16±6.40 preoperatively to 16.91±4.91 at the final follow-up (P<0.001).
Radiographic outcomes
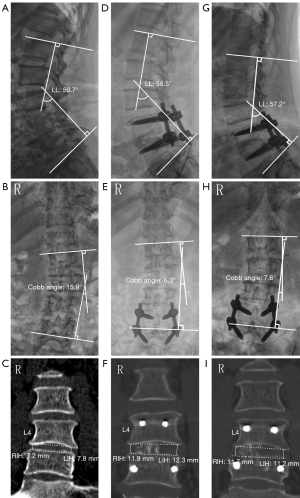
The radiographic results are summarized in Table 2. When compared with preoperative values, values at postoperative stage were characterized by a lower Taillard index (5.96%±3.90% vs. 14.74%±4.59%; P<0.001), Cobb angle (7.09°±1.60° vs. 13.52°±2.79°; P=0.003), DWA (1.14°±0.35° vs. 3.12°±0.73°; P<0.001), and lateral translation (0.58±0.23 vs. 1.32±0.44 mm; P=0.006), but higher AIH (14.50±3.96 vs. 12.02±4.30 mm; P=0.02), SA (11.12°±5.88° vs. 8.80°±7.12°; P=0.04), SS (39.08°±9.50° vs. 26.58°±14.27°; P<0.001), LIH (10.90±3.75 vs. 8.59±3.24 mm; P=0.03), and RIH (11.82±2.69 vs. 8.76±3.13 mm; P=0.01); the LL was similar pre-and postoperatively (44.94°±12.57° vs. 37.23°±26.15°, P=0.19). Moreover, all parameters at the final follow-up regressed mildly and non-significantly (Figure 3). Additionally, the DVR of the rank variable showed a significant decrease from Nash-Moe grade I preoperatively to grade 0 both postoperatively and at the final follow-up (both P<0.001).
Table 2
| Sagittal plane | Coronal plane | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Taillard index (%) | AIH (mm) | SA (°) | LL (°) | SS (°) | Cobb angle (°) | DWA (°) | Lateral translation (mm) | LIH (mm) | RIH (mm) | ||
| Preop | 14.74±4.59 | 12.02±4.30 | 8.80±7.12 | 37.23 ±26.15 | 26.58 ±14.27 | 13.52±2.79 | 3.12±0.73 | 1.32±0.44 | 8.59±3.24 | 8.76±3.13 | |
| Postop | 5.96±3.90* | 14.50±3.96* | 11.12±5.88* | 44.94 ±12.57 | 39.08 ±9.50* | 7.09±1.60* | 1.14±0.35* | 0.58±0.23* | 10.90±3.75* | 11.82±2.69* | |
| Final follow-up | 6.12±3.90* | 14.39±4.04* | 10.99±5.74* | 44.78±12.47 | 38.71±9.56* | 8.12±1.67* | 1.34±1.07* | 0.72±0.15* | 10.80±3.78* | 11.73±2.75* | |
Data are presented as mean ± standard deviation. Compared to preoperative values, *P<0.05. AIH, average intervertebral height; SA, slip angle; LL, lumbar lordosis; SS, sacral slope; DWA, disc wedging angle; LIH, left intervertebral height; RIH, right intervertebral height; Preop, preoperation; Postop, postoperation.
Outcome of linear regression analysis and mediation analysis
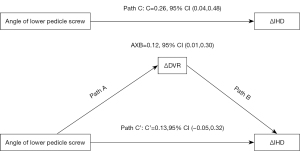
In the univariable linear regression analysis, ΔDVR, preoperative DWA, and angle of the lower pedicle screws were further considered for multiple linear regression analysis (Table 3). Multivariable linear regression analysis showed a positive impact of ΔDVR (B=1.55; P<0.001) and preoperative DWA (B=0.47; P=0.002) on ΔIHD, whereas there was no significant effect of the angle of the lower pedicle screws (B=0.13, P=0.14) on ΔIHD (Table 3), suggesting that a mediating variable exists in the correlation between the angle of the lower pedicle screw (angle 1.35°±8.46°) and ΔIHD. Moreover, ΔDVR was more appropriate for further mediation analysis as the mediating variable than was preoperative DWA according to the timeline. In the mediation analysis after adjustment for preoperative DWA, the total effect of the angle of the lower pedicle screw on ΔIHD was significant (C=0.26; 95% CI: 0.04–0.48). When ΔDVR was included, the direct effect on ΔIHD was not significant (C’=0.13; 95% CI: –0.05 to 0.32), whereas the indirect effect of the angle of the lower pedicle screw through ΔDVR was significant (AXB =0.12; 95% CI: 0.01–0.30; Figure 4).
Table 3
| Variable | Univariable analysis | Multivariable analysis | |||
|---|---|---|---|---|---|
| B (standard error) | P value | B (standard error) | P value | ||
| ΔLL | 0.02 (0.01) | 0.16 | – | – | |
| ΔDVR | 2.23 (0.25) | <0.001 | 1.55 (0.27) | <0.001 | |
| Pre-Cobb angle | 0.04 (0.09) | 0.64 | – | – | |
| Pre-DWA | 1.03 (0.15) | <0.001 | 0.47 (0.15) | 0.002 | |
| Prelateral translation | 0.24 (0.11) | 0.15 | – | – | |
| Pre-DLC | −0.52 (0.54) | 0.34 | – | – | |
| Angle of upper pedicle screw | 0.18 (0.13) | 0.16 | – | – | |
| Angle of lower pedicle screw | 0.54 (0.11) | <0.001 | 0.13 (0.09) | 0.14 | |
| Horizontal position of cage | −0.03 (0.03) | 0.28 | – | – | |
Δ, postoperative value − preoperative value; IHD, intervertebral height difference; LL, lumbar lordosis; DVR, degree of vertebral rotation; Pre, preoperative; DWA, disc wedging angle; DLC, direction of lateral curve.
Discussion
Preliminary clinical evaluation showed that TLIF was relatively safe with a reasonable operative time, blood loss, few complications but no reoperation, and an acceptable fusion rate during the follow-up when compared with those of previous studies (20-22). The clinical efficacy of surgery was also assessed, wherein relief in back and leg pain continued from after surgery to the final follow-up. Moreover, significant improvement of sagittal alignment was obtained as evidenced by the Taillard index, AIH, SA, and SS postoperatively, and at the final follow-up. The correction of sagittal alignment was in line with the findings of a previous study (23), wherein reduction in TLIF surgery favored the restoration of sagittal balance. Reduction of DLS reduces the forward displacement of the vertebra and favors the insertion of a large cage to increase intervertebral height (24). Moreover, successful reduction makes it easier to apply pressure on the rod and allows a large increase in SA to be achieved (25). Furthermore, SA is closely associated with SS and LL, and the restoration of SA helps to correct SS and LL (11). Combined with the fact that the center of gravity shifts toward the normal physiological line following reduction (25), the LL also showed an increase; however, this increase was statistically nonsignificant in our study. The reduction of spondylolisthesis improves sagittal balance to prevent the occurrence of compensation for spinal–pelvic malformations (26,27). In addition, loss of LL can accelerate coronal deformity and is a risk factor for lumbar scoliosis progression, reinforcing the necessity of correcting the sagittal alignment (28). Significant results were also found in the correction of Cobb angle, DWA, lateral translation, and DVR in lumbar degenerative scoliosis postoperatively and at the final follow-up. Patients with DLS with lumbar degenerative scoliosis adjust their posture by pelvic rotation and tilt to compensate for their sagittal imbalance, thus aggravating the decrease in LL and SS (29). The intradiscal pressure increases as lordosis decreases, which can exacerbate low back pain (30). Furthermore, the asymmetric intervertebral space and vertebral rotation in lumbar degenerative scoliosis typically cause asymmetric loading and progression of degeneration, which results in the deterioration of the lateral curve and eventual coronal imbalance (31). The destruction of joint capsules and facet joints frequently causes mono- or multidirectional instability, including deterioration of coronal alignment and anterior spondylolisthesis related to lumbar stenosis and neurogenic symptoms (32-34). These associations further demonstrate the significance of correcting lumbar degenerative scoliosis in patients with DLS. All of the radiographic parameters at the final follow-up had regressed mildly compared with postoperatively, which can perhaps be explained as the lack of muscle exercise which plays an important role in lumbar stability (35).
The correction of Cobb angle, DWA, and lateral translation in the study suggested that TLIF surgery benefited the restoration of asymmetric intervertebral space. Meanwhile, there is a necessity to identify which implant factor most impacts restoration of asymmetric intervertebral space. Due to effect of the off-center placement of the cage on the coronal curve correction noted in previous study (36), we analyzed the horizontal position of the cage in the univariable linear regression analysis but found no significant effect on ΔIHD, suggesting that the proximity to midline of the cage had no significant effect on the correction of asymmetric intervertebral space. However, multivariable linear regression and mediation analyses revealed that preoperative DWA and the angle of the lower pedicle screw exerted positive direct and indirect effects on ΔIHD. The effect of preoperative DWA on ΔIHD showed that if an increase of 1° is present in preoperative DWA, 0.47 units more will occur in postoperative correction of asymmetric intervertebral space. However, a high preoperative DWA might have a negative impact since further correction of 0.47 units brings less than a 1° increase of change in preoperative DWA. A higher preoperative DWA implies more challenging intraoperative restoration of asymmetric intervertebral space. However, the angle of the lower pedicle screw was found to have a different relation. The indirect effect (AXB =0.12) of the angle of the lower pedicle screw on ΔIHD indicates that for each degree the lower pedicle screw was oriented toward upper endplate, the asymmetric intervertebral space was corrected by 0.12 units, suggesting that the insertion of the lower pedicle screw could be angled upward toward the upper endplate intraoperatively and may benefit the restoration of IHD. A “vicious cycle” occurs in asymmetric degeneration, asymmetric loading, and asymmetric deformity, which manifests as asymmetric intervertebral space, vertebral rotation, and scoliosis in lumbar degenerative scoliosis (37-41). Meanwhile, according to the clinical experience of Du et al., slightly deeper placement of the pedicle screw more toward the concave side than toward the convex side helps to reduce the vertebral rotation, which is important in scoliosis resolution (40). Therefore, the phenomenon concerning the angle of the lower pedicle screw in our study could be explained as follows: when the lower pedicle screws were inserted toward the upper endplate, the range of motion of the screw head would be in a backward and downward position, and the titanium bar that was locked with the screw head perpendicularly could also be inclined further backward to a certain extent, thus leading to further reduction of the spondylolisthesis vertebra. More force was applied to the concave side of the spondylolisthesis vertebra, especially when a much greater cranial angle of the lower pedicle screw was used on the concave side. Vertebral rotation was then further corrected via the cranial direction of the lower pedicle screw, which aided the restoration of the asymmetric intervertebral space, thus helping further correct lumbar degenerative scoliosis (Figure 5). However, although some correlation was found between the cranial direction of the polyaxial pedicle screw and the restoration of the asymmetric intervertebral space, achievement of this requires a much further incline of the titanium bar and a greater reduction of the spondylolisthesis vertebra, which means that the screw head should be as parallel or as inclined backward to the screw rod as possible. The flexibility of the screw head of the polyaxial pedicle screw, which is designed for complex situations, indicates that the effect of reduction of spondylolisthesis and restoration of asymmetric intervertebral space may be somewhat weakened when the screw head is not parallel or inclined backward to the screw rod, and a much greater effect may occur when the screw head of the monoaxial pedicle screw, which is parallel to the screw rod, is applied.
In addition, some studies on the biomechanics of pedicle screw direction have shown that a cranial direction of the pedicle screw results in less pull-out stiffness, less bending moments, and higher peak and average stresses on pedicle screws compared with a caudad trajectory (42-44). Meanwhile, a biomechanical study revealed that a cranial direction could produce less stress concentration and more bending on the screw-rod system in comparison with parallel and caudad direction (45). The different conclusions of these studies might have arisen due the variability across samples and methods. Although the cranial direction was preferred in these studies, the placement point and path of these pedicle screws differed (some studies used Krag trajectory on human or animal vertebrae; some just applied a cranial direction on synthetic bone, and others used a finite element method). Furthermore, the methods used in these studies included pull-out test, torque test, and static loading, which were away from the tension–compression–bending fatigue loading on the pedicle screws in vivo (46-48). In other words, insertion methods of pedicle screw and loading modes in these studies were not the same as the path of and loading on the polyaxial pedicle screws completely, meaning that these results may not be applicable to this study. Despite the lack of biomechanical investigation for mechanical properties of cranial direction, clinical results at about 1-year follow-up were in a reasonable range compared with previous studies, which is relatively acceptable.
This study has several limitations. First, only 57 patients were included and analyzed retrospectively, and thus a study with a larger sample size adopting a prospective design is needed. Second, due to the flexibility of the screw head of polyaxial pedicle screw, achievement of a further incline of the titanium bar and increased reduction of spondylolisthesis vertebra requires the maximum possible parallelism or backward incline of the screw head to screw rod. This phenomenon may not always occur in a polyaxial pedicle screw but rather in a monoaxial pedicle screw, meaning that the effect of the direction of a monoaxial pedicle screw on the restoration of lumbar degenerative scoliosis may be stronger. Third, the lack of a corresponding biomechanical study makes it difficult to evaluate the long-term biomechanical properties of the pedicle screw in the cranial direction. Fourth, the approximately 1 year of follow-up in this study is shorter than that of some previous studies, meaning that some complications, like reoperation rate, adjacent segment degeneration, and pedicle screw break, which are typically reported after 2 years of follow-up, might not have been encountered (5,49,50). Fifth, the requirement of complete clinical and radiographic data in the inclusion criteria might have introduced some selection bias. In addition, this kind of TLIF surgical technique cannot be transposed to the treatment of patients with severe lumbar degenerative scoliosis because the lumbar degenerative scoliosis of the patients in our study was mild. However, severe lumbar degenerative scoliosis usually requires multilevel surgery. Finally, radiographs including the pelvis were not obtained, and we were unable to assess sagittal alignment comprehensively.
Conclusions
TLIF surgery is an effective approach for patients with DLS to yield improvements in clinical and radiographic outcomes. As for the DLS recognized as radiographic lumbar degenerative scoliosis preoperatively, the cranial direction of the lower pedicle screws in single-level unilateral TLIF surgery may be associated with a better postoperative restoration of lumbar degenerative scoliosis.
Acknowledgments
Funding: This work was supported by the Clinical Research Plan of SHDC (No. SHDC2020CR2035B), the National Natural Science Foundation of China (No. 81873774), the Shanghai Municipal Health Commission Program (No. 201940244), and the Jiading District Science and Technology Committee project (No. JDKW-2020-0039).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://qims.amegroups.com/article/view/10.21037/qims-22-483/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-22-483/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The retrospective cohort study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the ethics board of Tongji Hospital of Tongji University (No. K-2017-008), and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Iguchi T, Nishida K, Ozaki T, Kitagawa A, Tsumura N, Kakutani K, Yurube T, Kuroda R. Grade three disc degeneration is a critical stage for anterior spondylolisthesis in lumbar spine. Eur Spine J 2012;21:2134-9. [Crossref] [PubMed]
- Silva FE, Lenke LG. Adult degenerative scoliosis: evaluation and management. Neurosurg Focus 2010;28:E1. [Crossref] [PubMed]
- Takahashi T, Hanakita J, Watanabe M, Kawaoka T, Takebe N, Kitahara T. Lumbar alignment and clinical outcome after single level asymmetrical transforaminal lumbar interbody fusion for degenerative spondylolisthesis with local coronal imbalance. Neurol Med Chir (Tokyo) 2014;54:691-7. [Crossref] [PubMed]
- Jie Z, Yonghong Y. Effects of intervertebral disc and articular facet joint on occurrence and development of degenerative scoliosis: a biomechanical analysis on cadaveric spine. Chinese Journal of Spine and Spinal Cord 2018;28:826-31.
- Pan W, Zhao JL, Xu J, Zhang M, Fang T, Yan J, Wang XH, Zhou Q. Lumbar alignment and patient-reported outcomes after single-level transforaminal lumbar interbody fusion for degenerative lumbar spondylolisthesis with and without local coronal imbalance. J Neurosurg Spine 2020;34:464-70. [Crossref] [PubMed]
- Kato M, Namikawa T, Matsumura A, Konishi S, Nakamura H. Radiographic Risk Factors of Reoperation Following Minimally Invasive Decompression for Lumbar Canal Stenosis Associated With Degenerative Scoliosis and Spondylolisthesis. Global Spine J 2017;7:498-505. [Crossref] [PubMed]
- Kepler CK, Hilibrand AS, Sayadipour A, Koerner JD, Rihn JA, Radcliff KE, Vaccaro AR, Albert TJ, Anderson DG. Clinical and radiographic degenerative spondylolisthesis (CARDS) classification. Spine J 2015;15:1804-11. [Crossref] [PubMed]
- Hohenhaus M, Volz F, Merz Y, Watzlawick R, Scholz C, Hubbe U, Klingler JH. The challenge of measuring spinopelvic parameters: inter-rater reliability before and after minimally invasive lumbar spondylodesis. BMC Musculoskelet Disord 2022;23:104. [Crossref] [PubMed]
- Li R, Shao X, Li X, Liu Y, Jiang W. Comparison of clinical outcomes and spino-pelvic sagittal balance in degenerative lumbar spondylolisthesis: Minimally invasive oblique lumbar interbody fusion (OLIF) versus transforaminal lumbar interbody fusion (TLIF). Medicine (Baltimore) 2021;100:e23783. [Crossref] [PubMed]
- Seo JY, Ha KY, Hwang TH, Kim KW, Kim YH. Risk of progression of degenerative lumbar scoliosis. J Neurosurg Spine 2011;15:558-66. [Crossref] [PubMed]
- Kong LD, Zhang YZ, Wang F, Kong FL, Ding WY, Shen Y. Radiographic Restoration of Sagittal Spinopelvic Alignment After Posterior Lumbar Interbody Fusion in Degenerative Spondylolisthesis. Clin Spine Surg 2016;29:E87-92. [Crossref] [PubMed]
- Lee SM, Suk SI, Chung ER. Direct vertebral rotation: a new technique of three-dimensional deformity correction with segmental pedicle screw fixation in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2004;29:343-9. [Crossref] [PubMed]
- Xi X, Zeng Z, Li F, Wang C, Ma B, Xie N, Tsai TY, Li G, Yu Y, Cheng L. Caudad Insertion of Pedicle Screws Facilitates Interbody Distraction During Spondylolisthetic Vertebrae Restoration: A Retrospective Study. Pain Ther 2021;10:1537-50. [Crossref] [PubMed]
- La Maida GA, Peroni DR, Ferraro M, Della Valle A, Vitali C, Misaggi B. Apical vertebral derotation and translation (AVDT) for adolescent idiopathic scoliosis using screws and sublaminar bands: a safer concept for deformity correction. Eur Spine J 2018;27:157-64. [Crossref] [PubMed]
- Çetin E, Özkaya M, Güler ÜÖ, Acaroğlu E, Demir T. Evaluation of the Effect of Fixation Angle between Polyaxial Pedicle Screw Head and Rod on the Failure of Screw-Rod Connection. Appl Bionics Biomech 2015;2015:150649. [Crossref] [PubMed]
- Nash CL Jr, Moe JH. A study of vertebral rotation. J Bone Joint Surg Am 1969;51:223-9. [Crossref] [PubMed]
- Park JS, Park SJ, Lee CS, Yum TH, Kim BT. Radiologic prognostic factors of curve progression in early degenerative lumbar scoliosis. J Neurosurg Spine 2021;34:557-63. [Crossref] [PubMed]
- Li F, Zhan X, Xi X, Zeng Z, Ma B, Xie N, Zhu R, Tsai TY, Li G, Yu Y, Cheng L. Do the positioning variables of the cage contribute to adjacent facet joint degeneration? Radiological and clinical analysis following intervertebral fusion. Ann Transl Med 2021;9:776. [Crossref] [PubMed]
- Bockorny K, Youssef-Morgan CM. Entrepreneurs' Courage, Psychological Capital, and Life Satisfaction. Front Psychol 2019;10:789. [Crossref] [PubMed]
- Parker SL, Mendenhall SK, Shau DN, Zuckerman SL, Godil SS, Cheng JS, McGirt MJ. Minimally invasive versus open transforaminal lumbar interbody fusion for degenerative spondylolisthesis: comparative effectiveness and cost-utility analysis. World Neurosurg 2014;82:230-8. [Crossref] [PubMed]
- Liu J, Deng H, Long X, Chen X, Xu R, Liu Z. A comparative study of perioperative complications between transforaminal versus posterior lumbar interbody fusion in degenerative lumbar spondylolisthesis. Eur Spine J 2016;25:1575-80. [Crossref] [PubMed]
- Galbusera F, Volkheimer D, Reitmaier S, Berger-Roscher N, Kienle A, Wilke HJ. Pedicle screw loosening: a clinically relevant complication? Eur Spine J 2015;24:1005-16. [Crossref] [PubMed]
- Bai X, Chen J, Liu L, Li X, Wu Y, Wang D, Ruan D. Is reduction better than arthrodesis in situ in surgical management of low-grade spondylolisthesis? A system review and meta analysis. Eur Spine J 2017;26:606-18. [Crossref] [PubMed]
- Takami M, Taiji R, Okada M, Minamide A, Hashizume H, Yamada H. Lateral lumbar interbody fusion after reduction using the percutaneous pedicle screw system in the lateral position for Meyerding grade II spondylolisthesis: a preliminary report of a new lumbar reconstruction strategy. BMC Musculoskelet Disord 2021;22:17. [Crossref] [PubMed]
- Heo DH, Jang JW, Lee JK, Park CK. Slippage reduction of lumbar spondylolisthesis using percutaneous pedicle screw with reduction fixation system after interbody fusion: A comparison with traditional open fusion and pedicle screw fixation. J Clin Neurosci 2019;67:156-62. [Crossref] [PubMed]
- Longo UG, Loppini M, Romeo G, Maffulli N, Denaro V. Evidence-based surgical management of spondylolisthesis: reduction or arthrodesis in situ. J Bone Joint Surg Am 2014;96:53-8. [Crossref] [PubMed]
- Su K, Luan J, Wang Q, Yang Y, Mei W, Zhang Z. Radiographic Analysis of Minimally Invasive Transforaminal Lumbar Interbody Fusion versus Conventional Open Surgery on Sagittal Lumbar-Pelvic Alignment for Degenerative Spondylolisthesis. World Neurosurg 2019;124:e733-9. [Crossref] [PubMed]
- Faraj SS, Holewijn RM, van Hooff ML, de Kleuver M, Pellisé F, Haanstra TM. De novo degenerative lumbar scoliosis: a systematic review of prognostic factors for curve progression. Eur Spine J 2016;25:2347-58. [Crossref] [PubMed]
- Han F, Weishi L, Zhuoran S, Qingwei M, Zhongqiang C. Sagittal plane analysis of the spine and pelvis in degenerative lumbar scoliosis. J Orthop Surg (Hong Kong) 2017;25:2309499016684746. [Crossref] [PubMed]
- Lord MJ, Small JM, Dinsay JM, Watkins RG. Lumbar lordosis. Effects of sitting and standing. Spine (Phila Pa 1976) 1997;22:2571-4. [Crossref] [PubMed]
- Sapkas G, Efstathiou P, Badekas AT, Antoniadis A, Kyratzoulis J, Meleteas E. Radiological parameters associated with the evolution of degenerative scoliosis. Bull Hosp Jt Dis 1996;55:40-5. [PubMed]
- Epstein JA, Epstein BS, Jones MD. Symptomatic lumbar scoliosis with degenerative changes in the elderly. Spine (Phila Pa 1976) 1979;4:542-7. [Crossref] [PubMed]
- Shapiro GS, Taira G, Boachie-Adjei O. Results of surgical treatment of adult idiopathic scoliosis with low back pain and spinal stenosis: a study of long-term clinical radiographic outcomes. Spine (Phila Pa 1976) 2003;28:358-63. [Crossref] [PubMed]
- Yasuda H, Matsumura A, Terai H, Toyoda H, Suzuki A, Dozono S, Nakamura H. Radiographic evaluation of segmental motion of scoliotic wedging segment in degenerative lumbar scoliosis. J Spinal Disord Tech 2013;26:379-84. [Crossref] [PubMed]
- Finta R, Nagy E, Bender T. The effect of diaphragm training on lumbar stabilizer muscles: a new concept for improving segmental stability in the case of low back pain. J Pain Res 2018;11:3031-45. [Crossref] [PubMed]
- Heary RF, Karimi RJ. Correction of lumbar coronal plane deformity using unilateral cage placement. Neurosurg Focus 2010;28:E10. [Crossref] [PubMed]
- Peterson JB, Wenger DR. Asymmetric spondylolisthesis as the cause of childhood lumbar scoliosis--can new imaging modalities help clarify the relationship? Iowa Orthop J 2008;28:65-72. [PubMed]
- Shin JH, Wang S, Yao Q, Wood KB, Li G. Investigation of coupled bending of the lumbar spine during dynamic axial rotation of the body. Eur Spine J 2013;22:2671-7. [Crossref] [PubMed]
- Kim DB, Shin MH, Kim JT. Vertebral Body Rotation in Patients with Lumbar Degenerative Scoliosis: Surgical Implication for Oblique Lumbar Interbody Fusion. World Neurosurg 2018;S1878-8750(18)32896-1. Epub ahead of print. [Crossref] [PubMed]
- Du CZ, Zhu ZZ, Wang Y, Li S, Xu L, Wang B, Qiu Y, Sun X. Curve Characteristics and Response of Sciatic and Olisthesis Scoliosis Following L5/S1 Transforaminal Lumbar Interbody Fusion in Adolescent Lumbar Spondylolisthesis. Neurosurgery 2021;88:322-31. [Crossref] [PubMed]
- Aebi M. The adult scoliosis. Eur Spine J 2005;14:925-48. [Crossref] [PubMed]
- Yuan Q, Han X, Han X, He D, Liu B, Tian W. Krag versus Caudad trajectory technique for pedicle screw insertion in osteoporotic vertebrae: biomechanical comparison and analysis. Spine (Phila Pa 1976) 2014;39:B27-35. [Crossref] [PubMed]
- Youssef JA, McKinley TO, Yerby SA, McLain RF. Characteristics of pedicle screw loading. Effect of sagittal insertion angle on intrapedicular bending moments. Spine (Phila Pa 1976) 1999;24:1077-81. [Crossref] [PubMed]
- Molinari L, Falcinelli C, Gizzi A, Di Martino A. Effect of pedicle screw angles on the fracture risk of the human vertebra: A patient-specific computational model. J Mech Behav Biomed Mater 2021;116:104359. [Crossref] [PubMed]
- Song M, Sun K, Li Z, Zong J, Tian X, Ma K, Wang S. Stress distribution of different lumbar posterior pedicle screw insertion techniques: a combination study of finite element analysis and biomechanical test. Sci Rep 2021;11:12968. [Crossref] [PubMed]
- Cho W, Cho SK, Wu C. The biomechanics of pedicle screw-based instrumentation. J Bone Joint Surg Br 2010;92:1061-5. [Crossref] [PubMed]
- Tan JS, Kwon BK, Dvorak MF, Fisher CG, Oxland TR. Pedicle screw motion in the osteoporotic spine after augmentation with laminar hooks, sublaminar wires, or calcium phosphate cement: a comparative analysis. Spine (Phila Pa 1976) 2004;29:1723-30. [Crossref] [PubMed]
- Nowak B. Experimental study on the loosening of pedicle screws implanted to synthetic bone vertebra models and under non-pull-out mechanical loads. J Mech Behav Biomed Mater 2019;98:200-4. [Crossref] [PubMed]
- Ye J, Yang S, Wei Z, Cai C, Zhang Y, Qiu H, Chu T. Incidence and Risk Factors for Adjacent Segment Disease After Transforaminal Lumbar Interbody Fusion in Patients with Lumbar Degenerative Diseases. Int J Gen Med 2021;14:8185-92. [Crossref] [PubMed]
- Butt MF, Farooq M, Mir B, Dhar AS, Hussain A, Mumtaz M. Management of unstable thoracolumbar spinal injuries by posterior short segment spinal fixation. Int Orthop 2007;31:259-64. [Crossref] [PubMed]


