
A case report of colonic stent placement without X-ray control in the COVID-19 era: a practical method or a mistake?
Introduction
Colonic stenting is used for the management of colorectal obstruction as a palliative and perioperative treatment in surgical patients. This approach can be useful in emergency settings and accommodates the optimal management of a patient’s condition by decompressing the obstruction and allowing the passage of stools and gases in the safest way. A retrospective study by Zhou et al. in 2020 demonstrated that colonic stent placement without fluoroscopy is as safe and effective as the conventional, fluoroscopically-guided approach (1). According to the recommendations of the European Society of Gastrointestinal Endoscopy (ESGE), colonic stenting should be performed with the combined use of endoscopy and fluoroscopy (2). However, is colonic stenting feasible in the absence of an X-ray? Further, is this justified?
From March to July 2020 and in January 2021 our hospital was re-purposed to provide care for patients with coronavirus disease 2019 (COVID-19). All X-ray equipment was intensively used, and thus access to the X-ray operating room and equipment for stenting was limited. By that time, we had performed more than 220 colonic stenting procedures and more than 400 esophageal and stomach stenting procedures. Despite the pandemic, the coloproctological hospital still admitted a limited number of patients on an elective and emergency basis in a separate building, which also housed the computed tomography (CT) room. During these 6 months, 13 stenting procedures [5 in curative (stent bridge-to-surgery) and 8 in palliative settings] were successfully performed, with relief of obstructive symptoms, under endoscopic control without fluoroscopic guidance. We present the following case in accordance with the CARE reporting checklist (available at https://qims.amegroups.com/article/view/10.21037/qims-22-319/rc).
Case presentation
An 81-year-old woman was admitted in January 2021 with complaints of abdominal pain, bloating, and stool retention for up to 6 days. Blood analysis revealed leukocytosis of up to 18×109 L with left shift, an abnormally high erythrocyte sedimentation rate (ESR) of up to 30 mm/h, a 30% increase in hematocrit (Ht) concentration, hyponatremia (95 mmol/L), hypokalemia (3 mmol/L), an increase in urea concentration of up to 270 mg/dL, and an increase in creatinine of up to 2,700 mg/dL. Moreover, the patient had severe concomitant chronic heart failure [New York Heart Association (NYHA) 3], hypertension stage II (grade 3) with a risk of cardiovascular complications of grade 4 (very high), as well as atherosclerosis of the coronary and cerebral arteries. An emergency CT abdominal scan revealed an irregular focal thickening of the wall of the rectosigmoid junction of up to 7 mm and over a length of 18 mm. The lesions suspected of metastases were not defined.
At the medical case conference, a minimally invasive intervention was recommended to decompress the intestine and, if possible, prepare the patient for radical surgery, taking into consideration her age, condition, and somatic status with decompensated concomitant illness. We decided to perform bowel decompression by placing a self-expandable metallic stent (SEMS) via colonoscopy without fluoroscopic monitoring. The length of the stent was selected according to the CT data, specifically, the length of the tumor along the intestine plus 4 cm. The patient was informed about all potential complications and interventions that might be necessary.
Colonoscopy (without active carbon dioxide insufflation) of the rectosigmoid area showed circumferential tumor infiltration with narrowing of the lumen to approximately 3 mm. A biopsy sample was taken. Subsequent histological examination confirmed the diagnosis of a well-differentiated adenocarcinoma (G1).
Using the “seeking” approach, a metal guidewire with a diameter of 0.035” and a straight atraumatic tip was advanced through the tumor stenosis into the distal part of the descending colon under endoscopic control. During placement of the guidewire, we could see the flow of liquid intestinal contents coming from the proximal dilated part of the intestine, which was indicative of reaching the proximal margin of the stenosis. A BVM Medical EGIS colorectal double-covered stent (BVM Medical; Cook, United Kingdom) of 24-mm diameter and 60-mm length was placed in a delivery container and advanced over the guidewire, under endoscopic control. The stent was placed 2 cm distal to the tumor and properly oriented by video (through the transparent wall of the container) (Video 1). Within 1–2 minutes after the opening of the partial stent, an abundance of liquid stools and gases was observed passing through the stent lumen. The patient noticed an improvement in the symptoms of colonic obstruction, including a reduction in abdominal pain, bloating, and stool retention.
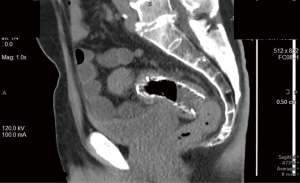
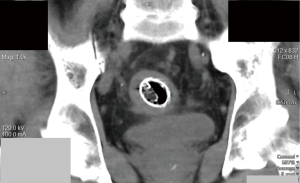
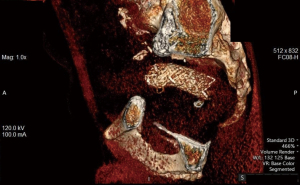
Immediately after stenting, the patient underwent abdominal CT. There were no signs of free gas in the abdominal cavity. Intestinal pneumatization was moderately enhanced on the right side. In the area of the rectosigmoid transition, the shadow of the stent was determined: it was symmetrically opened and had an hourglass-shape with a “waist” of up to 5 mm (Figures 1-3).
All procedures performed in this study were in accordance with the ethical standards of the institution and the Helsinki Declaration (as revised in 2013). Written informed consent was provided by the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
The most common approach to the treatment of patients with neoplastic obstruction of the left colon is the formation of a double-barreled stoma followed by resection of the intestine and lymphadenectomy. Another approach is to perform resection of the obstructive colon with colostomy, followed by lymphadenectomy and reconstructive surgery (3). In both situations, patients undergo 2 major abdominal surgeries with general anesthesia and endotracheal intubation. The latest ESGE guidelines (2020) consider stenting in patients with apparently resectable colorectal neoplasia. Specifically, the ESGE recommends stenting as a bridge to surgery and an alternative to emergency resection in patients with potentially curable left-sided obstructive colon cancer and that stenting should be discussed as a treatment option (strong recommendation, high quality evidence) with the patient in a shared decision-making process A stoma is also considered a valid option, and the ESGE suggests that a decompressing stoma as a bridge to elective surgery is a valid option if the patient is not a candidate for colonic stenting or when stenting expertise is not available. In palliative patients, the ESGE recommends colonic stenting as the preferred treatment for palliation of malignant colonic obstruction (2).
Colonic stents are placed under combined endoscopic and fluoroscopic guidance, which is necessary for the safety of the procedure. We completely agree with this statement since performing a stent placement without both types of guidance can lead to complications such as bleeding and perforation (4,5). A limitation of this method is that it cannot be used independently of X-ray control, which is still required after the procedure.
However, our forced clinical experience has shown that in desperate situations and in cases of severely impacted patients, an experienced endoscopic team can perform colonic stenting without direct X-ray navigation (provided there is the appropriate selection of stent design and size according to findings on a preliminary CT scan), if an X-ray is unavailable due to unforeseen circumstances. All 13 colonic stentings we conducted in this way successfully provided decompression of the intestines without any complications. In 5 patients, radical surgery was performed as a second step, and in 8 patients, stenting became the final method of palliative decompression, after which patients received chemotherapy.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://qims.amegroups.com/article/view/10.21037/qims-22-319/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-22-319/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institution and with the Helsinki Declaration (as revised in 2013). Written informed consent was provided by the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Zhou Y, Zhang X, Kang J, Zhang X, Song Y. Safety and Efficacy of Through-the-Scope Placement of Colonic Self-expandable Metal Stents Without Fluoroscopic Guidance: A Retrospective Cohort Study. Surg Laparosc Endosc Percutan Tech 2020;30:430-4. [Crossref] [PubMed]
- van Hooft JE, Veld JV, Arnold D, Beets-Tan RGH, Everett S, Götz M, van Halsema EE, Hill J, Manes G, Meisner S, Rodrigues-Pinto E, Sabbagh C, Vandervoort J, Tanis PJ, Vanbiervliet G, Arezzo A. Self-expandable metal stents for obstructing colonic and extracolonic cancer: European Society of Gastrointestinal Endoscopy (ESGE) Guideline - Update 2020. Endoscopy 2020;52:389-407. [Crossref] [PubMed]
- Charyshkin AL, Keshyan EA. Method of stoma formation in patients with acute intestinal obstruction. Ul'yanovskiy mediko-biologicheskiy zhurnal 2021;1:98-104
- Mitra V, Hu M, Majumdar D, Krishnan V, Chaudhury B, Hancock J, Dwarakanath D. Safety and efficacy of self-expandable metal stents for obstructive proximal and distal large bowel cancer. J R Coll Physicians Edinb 2017;47:30-4. [Crossref] [PubMed]
- Kim JH, Ku YS, Jeon TJ, Park JY, Chung JW, Kwon KA, Park DK, Kim YJ. The efficacy of self-expanding metal stents for malignant colorectal obstruction by noncolonic malignancy with peritoneal carcinomatosis. Dis Colon Rectum 2013;56:1228-32. [Crossref] [PubMed]


