
Reproducibility of the anorectal angle with transperineal ultrasound
Introduction
The anorectal angle (ARA) is a mechanism that influences in anal continence along with the sphincteric function, distensibility of the rectum, fecal consistency, intestinal motility and the integrity of the innervation of the different structures involved. The ARA delimits the anorectal junction created from the impression of the puborectalis muscle at the posterior edge of the rectum (1). At rest, the ARA is more acute, favoring passive continence (1). However, during voluntary defecation, the coordination between the ARA (becoming more obtuse) and sphincteric relaxation is crucial to achieve emptying of the rectum, without a significant lowering of the pelvic floor (1,2). Measurement of the ARA has been used as a predictor of post-surgical continence (3) and as a method to assess the adequate function of the striated muscle complex (3). The ARA is modified in patients with continence issues and, in addition, it has also been observed that age, body mass index and parity can affect the ARA (4). In fact, patients with levator ani muscle (LAM) avulsion have a wider ARA than patients without LAM avulsion (5).
The ARA has been assessed with different imaging methods and its measurement has traditionally been based on defecography or magnetic resonance studies (6-11). However, these imaging tests are not the only way to evaluate the ARA, and recently, it has been shown that ultrasound is comparable to defecography for the study of ARA (12). The wide interobserver variation of ARA measurements by defecography suggests that its assessment may be of limited clinical value (13). However, this interobserver variation has been lessened in a subsequent publication (7). Different ultrasound methodologies have also been used for ARA assessment and have been validated as alternatives for the ARA measurement, such as three-dimensional (3D) endovaginal ultrasound (14) and 3D transperineal ultrasound (5). The difference between them lies in the fact that 3D transperineal ultrasound (5) does not require the introduction of ultrasound transducers inside the anal canal, as occurs with 3D endovaginal probe (14). Therefore, it is reasonable to think that the use of transperineal ultrasound can provide more reproducible ARA measurements, something that has not been established by 3D endovaginal probe (14) or defecography (7,13). Therefore, our objective is to determine the intraobserver and interobserver variability of transperineal ultrasound for the assessment of ARA.
Methods
Study population
A retrospective observational study was performed with data acquired from patients that had been included in a previous study (5). Forty patients were randomly selected from the previously described study (5), including 20 patients with LAM avulsion and 20 patients without LAM avulsion. All patients were primiparous, had delivered vaginally at term, had given written informed consent to participate in the study and did not have pelvic floor corrective surgery. There were different obstetric and fetal parameters analyzed for each patient.
Examination method
The offline acquisition and analysis of the volumes [previously described (15)] was performed 6 months after delivery, by a single examiner with specific training in 3D pelvic floor ultrasound (JA García-Mejido) with a 500® Toshiba Aplio (Toshiba Medical Systems Corp., Tokyo, Japan) ultrasound with a PVT-675MV 3D abdominal probe. Three volumes were acquired for each patient: at rest, in Valsalva and at maximum contraction. Avulsion was defined based on the maximum contraction image in the multislice mode (16,17). Complete avulsion was diagnosed when there was abnormal insertion of the LAM in the 3 central slices. In unclear cases, a levator-urethra gap >2.5 cm was used to define an abnormal insertion (18).
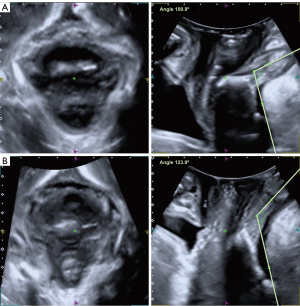
The study of the ARA was performed in the mid-sagittal plane, visualizing the anorectal canal, the anorectal junction and the rectal ampulla. The measurement of the ARA was obtained following the methodology previously described for defecography and magnetic resonance studies (6,7). The assessment was performed at rest, Valsalva and maximum contraction, defining the ARA as the angle between the posterior and distal edge of the rectum and the central axis of the anal canal (6-11) (Figure 1). The measurements were initially performed by explorer 1 (E1), then by explorer 2 (E2) and finally again by E1, leaving a one-month interval between the different explorations. Both the patient data and the data obtained by each explorer were anonymized and each scan performed by the explorers (E1 and E2) was stored in the ultrasound scanner’s memory. The only person who extracted all the data, unified it in tables and knew the identity of the patients whose volumes were studied, was the main researcher (JA García-Mejido).
Sample size
The sample size was based on the determination of the intraclass correlation coefficient (ICC) as a measure of the reliability of the measurements of the two explorers for the evaluation of the ARA with transperineal ultrasound. For the sample size calculation, we assumed a worst-case expected ICC value of 0.60 (based on previous experience), a 95% confidence interval, an accuracy or range of 0.2 and two measurements/observers. To meet these requirements, it was necessary to include at least 40 women in the study. Because LAM avulsion modifies the ARA (19), the decision was to include half of the patients with LAM avulsion (n=20) and half without LAM avulsion (n=20).
Statistical analysis
The values obtained were analyzed by calculating ICCs with 95 % confidence interval (CI); an ICC value <0.20 was considered poor, 0.21–0.40 was considered fair, 0.41–0.60 was considered moderate, 0.61–0.80 was considered good, and 0.81–1.00 was considered to have an excellent reliability (20). The Bland-Altman 95% limits of agreement (LOA) method (20) was used to assess mean interobserver difference (“bias”). To assess significant bias, the 95% CI of the bias in each case was used to determine if the bias differed from zero. Statistical analysis was performed with IBM SPSS Statistics 26 software.
Ethical approval
The study was approved by Andalucia’s Board of Biomedicine Ethics Committee, with codes 0545-N-18, 0153-N-17 and 3004/2012. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). All patients gave their written informed consent before starting the study.
Results
Our study population included 40 patients, 20 with LAM avulsion and 20 without LAM avulsion. The mean age of the patients included was 31.10±4.45 years, they had presented a vaginal delivery at 39.80±1.02 weeks of gestation, being 11 (27.5%) of them induced labors. Epidural analgesia was present in 38 (95.0%) cases, in which the mean epidural analgesia time was 391.78±184.30 min. The second stage labor time was 111.18±88.22 min, episiotomy was performed in 31 (77.50%) cases and perineal tears were present in 13 (32.5%). The newborns had a mean weight of 3,386.00±364.51 g with a mean fetal head circumference of 34.72±1.37 cm.
The intraobserver variability for the measurement of ARA studied with transperineal ultrasound established between the two scans performed by E1 are reflected in Table 1 (Figure 1). Excellent reliability was observed for all measurements of ARA at rest, Valsalva and maximal contraction, with ICC ranging from 0.968 to 0.975 in the overall population, ranging from 0.929 to 0.966 in patients without LAM avulsion and ranging from 0.982 to 0.975 in patients with LAM avulsion.
Table 1
| Variables | E1 (first assessment) | E1 (second assessment) | P | 95% CI | ICC (95% CI) |
|---|---|---|---|---|---|
| All (n=40) | |||||
| Anorectal angle (º) | |||||
| Rest, mean ± SD | 120.8±7.3 | 121.1±7.9 | 0.568 | −1.10; 0.61 | 0.968 (0.939; 0.983) |
| Valsalva, mean ± SD | 119.9±8.3 | 120.3±8.9 | 0.345 | −1.42; 0.51 | 0.969 (0.940; 0.983) |
| Maximum contraction, mean ± SD | 116.1±9.0 | 116.4±9.0 | 0.432 | −1.25; 0.55 | 0.975 (0.953; 0.987) |
| Without LAM avulsion (n=20) | |||||
| Anorectal angle (º) | |||||
| Rest, mean ± SD | 120.1±5.6 | 119.9±5.6 | 0.794 | −1.18; 1.52 | 0.929 (0.820; 0.972) |
| Valsalva, mean ± SD | 120.5±6.7 | 119.9±7.3 | 0.320 | −0.61; 1.77 | 0.966 (0.914; 0.987) |
| Maximum contraction, mean ± SD | 113.1±8.5 | 113.2±8.5 | 0.867 | −1.67; 1.42 | 0.961 (0.901; 0.984) |
| With LAM avulsion (n=20) | |||||
| Anorectal angle (º) | |||||
| Rest, mean ± SD | 121.6±8.8 | 122.3±9.7 | 0.250 | −1.82; 0.50 | 0.982 (0.953; 0.993) |
| Valsalva, mean ± SD | 119.2±9.7 | 120.7±10.5 | 0.047 | −2.96; −0.02 | 0.975 (0.938; 0.990) |
| Maximum contraction, mean ± SD | 119.0±8.6 | 119.6±8.5 | 0.269 | −1.65; 0.48 | 0.982 (0.954; 0.993) |
ARA, anorectal angle; CI, confidence interval; E1, explorer 1; ICC, intraclass correlation coefficient; LAM, levator ani muscle; SD, standard deviation.
The interobserver variability for the measurement of the ARA studied with transperineal ultrasound obtained between the means of the two scans performed by E1 compared to the measurements acquired by E2 are reflected in Table 2 (Figure 2). Superb reliability was observed in all measurements of ARA at rest, Valsalva and maximal contraction, with the ICC ranging from 0.971 to 0.979 in the overall population, varying between 0.953 and 0.976 in patients without LAM avulsion and fluctuating between 0.977 and 0.983 in patients with LAM avulsion.
Table 2
| Variables | E1 | E2 | P | 95% CI | ICC (95% CI) |
|---|---|---|---|---|---|
| All (n=40) | |||||
| Anorectal angle (º) | |||||
| Rest, mean ± SD | 121.0±7.5 | 122.3±7.4 | 0.001 | −2.03, −0.57 | 0.976 (0.955, 0.987) |
| Valsalva, mean ± SD | 120.1±8.5 | 121.0±9.1 | 0.069 | −1.82, 0.07 | 0.971 (0.945, 0.985) |
| Maximum contraction, mean ± SD | 116.2±8.9 | 117.9±9.9 | <0.0005 | −2.57, −0.82 | 0.979 (0.959, 0.989) |
| Without LAM avulsion (n=20) | |||||
| Anorectal angle (º) | |||||
| Rest, mean ± SD | 129.0±5.4 | 121.3±5.2 | 0.016 | −2.38, −0.28 | 0.953 (0.882, 0.982) |
| Valsalva, mean ± SD | 120.2±6.9 | 121.1±7.8 | 0.172 | −2.28, 0.44 | 0.959 (0.897, 0.984) |
| Maximum contraction, mean ± SD | 113.2±8.3 | 114.7±9.1 | 0.016 | −2.81, −0.33 | 0.976 (0.940, 0.991) |
| With LAM avulsion (n=20) | |||||
| Anorectal angle (º) | |||||
| Rest, mean ± SD | 121.9±9.2 | 123.2±9.2 | 0.026 | −2.37, −0.17 | 0.983 (0.958, 0.993) |
| Valsalva, mean ± SD | 120.0±10.0 | 120.8±10.4 | 0.245 | −2.26, 0.61 | 0.977 (0.941, 0.991) |
| Maximum contraction, mean ± SD | 119.3±8.5 | 121.1±9.9 | 0.010 | −3.16, −0.48 | 0.975 (0.938, 0.990) |
ARA, anorectal angle; CI, confidence interval; E1, explorer 1; E2, explorer 2; ICC, intraclass correlation coefficient; LAM, levator ani muscle; SD, standard deviation.

Discussion
The intraobserver and interobserver variability for ARA measurement studied with transperineal ultrasound has been excellent at rest, Valsalva and maximal contraction. This could suggest that this methodology for measuring ARA is more reproducible than those previously described (7,13,14). Study using defecography in asymptomatic patients showed that there was a wide inter-observer variation in the assessment of ARA (21). In fact, they advised that defecographic measurements should be interpreted with caution when assessing the patient (21). Subsequently, it was defined that measurement of ARA with defecography is influenced by the experience of the investigator, the analysis method and the anorectal characteristics (22). This low reproducibility of ARA calculation has come to question the clinical value of ARA (23). However, when we compared defecography versus magnetic resonance imaging (MRI) we observed that MRI offers a more accurate and more comfortable measurement for the patient than defecography (24). This aspect could be due to the fact that MRI better assesses the anatomical landmarks for ARA measurement. For this reason, we believe that our results are so favorable since transperineal ultrasound allows us to more precisely delimit the anatomical structures involved in the measurement of ARA, as can be seen in Figure 1. Santoro et al. (14) proved that the overall interobserver repeatability for ARA was moderate (ICC, 0.472) and the interdisciplinary repeatability for ARA was fair to moderate (ICC, 0.204–0.434). However, Santoro et al. (14) used 3D endovaginal ultrasound for the measurement of ARA, and this technique could modify the anatomical morphology because it is an intracavitary probe technique unlike transperineal ultrasound, as proposed in our research.
The value of the ARA has been a much-discussed value, and there have been many attempts to standardize the modifications that the ARA undergoes during the course of a woman’s life. It has been defined that the normal ARA ranges between 94 and 114 degrees at rest, and it changes between 15 and 20 degrees during defecation or contraction (15). The importance of ARA in the late development of mild pathology, such as dyssynergia or anismus, and of more severe conditions, such as fecal incontinence or anal prolapse, has been described (25). Furthermore, it has been observed that the ARA is closely related to the integrity of the LAM (5) and, therefore, we have designed a study to assess the interobserver and intraobserver variability in patients with and without LAM avulsion. This value of the ARA has not been correlated to current clinical practice, probably due to variations in its measurement when using conventional techniques (21-24); these variations are solved when using transperineal ultrasound, as we have observed in our research. Consequently, based on our data, we propose a new methodology for the measurement of ARA that may be transferable to routine clinical practice, this being the most noteworthy aspect of the study.
Our main strength lies in the good results obtained in the measurement of intraobserver and interobserver variability of ARA, establishing a simple methodology that can be applied in the examination room. However, our main limitation is that we need studies with a larger number of explorers, in a multicenter clinical trial, to verify the data we have obtained.
Conclusions
We have described excellent intraobserver and interobserver variability for ARA measurement by transperineal ultrasound.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-22-714/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Andalucia’s Board of Biomedicine Ethics Committee, with codes 0545-N-18, 0153-N-17 and 3004/2012. All patients gave their written informed consent before starting the study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Lalwani N, El Sayed RF, Kamath A, Lewis S, Arif H, Chernyak V. Imaging and clinical assessment of functional defecatory disorders with emphasis on defecography. Abdom Radiol (NY) 2021;46:1323-33. [Crossref] [PubMed]
- Sun D, Liao D, Chen SC, Wong C, Wah Leung W, Futaba K, Mak T, Ng S, Gregersen H. Mechanophysiological analysis of anorectal function using simulated feces in human subjects. J Adv Res 2020;28:245-54. [Crossref] [PubMed]
- Desai SN, Choudhury H, Joshi P, Pargewar S. Magnetic resonance imaging evaluation after anorectal pull-through surgery for anorectal malformations: a comprehensive review. Pol J Radiol 2018;83:e348-52. [Crossref] [PubMed]
- Tirumanisetty P, Prichard D, Fletcher JG, Chakraborty S, Zinsmeister AR, Bharucha AE. Normal values for assessment of anal sphincter morphology, anorectal motion, and pelvic organ prolapse with MRI in healthy women. Neurogastroenterol Motil 2018;30:e13314. [Crossref] [PubMed]
- García-Mejido JA, García-Pombo S, Fernández-Conde C, Borrero C, Fernández-Palacín A, Sainz-Bueno JA. The Role of Transperineal Ultrasound for the Assessment of the Anorectal Angle and Its Relationship with Levator Ani Muscle Avulsion. Tomography 2022;8:1270-6. [Crossref] [PubMed]
- Roos JE, Willmann JK, Weishaupt D, Lachat M, Marincek B, Hilfiker PR. Thoracic aorta: motion artifact reduction with retrospective and prospective electrocardiography-assisted multi-detector row CT. Radiology 2002;222:271-7. [Crossref] [PubMed]
- Choi JS, Wexner SD, Nam YS, Mavrantonis C, Salum MR, Yamaguchi T, Weiss EG, Nogueras JJ, Yu CF. Intraobserver and interobserver measurements of the anorectal angle and perineal descent in defecography. Dis Colon Rectum 2000;43:1121-6. [Crossref] [PubMed]
- Turnbull GK, Bartram CI, Lennard-Jones JE. Radiologic studies of rectal evacuation in adults with idiopathic constipation. Dis Colon Rectum 1988;31:190-7. [Crossref] [PubMed]
- Wald A, Caruana BJ, Freimanis MG, Bauman DH, Hinds JP. Contributions of evacuation proctography and anorectal manometry to evaluation of adults with constipation and defecatory difficulty. Dig Dis Sci 1990;35:481-7. [Crossref] [PubMed]
- Jorge JM, Wexner SD, Marchetti F, Rosato GO, Sullivan ML, Jagelman DG. How reliable are currently available methods of measuring the anorectal angle? Dis Colon Rectum 1992;35:332-8. [Crossref] [PubMed]
- Jorge JM, Ger GC, Gonzalez L, Wexner SD. Patient position during cinedefecography. Influence on perineal descent and other measurements. Dis Colon Rectum 1994;37:927-31. [Crossref] [PubMed]
- Yao YB, Yin HQ, Wang HJ, Liang HT, Wang B, Wang C. Is the transperineal ultrasonography approach effective for the diagnosis of rectocele? Gastroenterol Rep (Oxf) 2021;9:461-9. [Crossref] [PubMed]
- Ferrante SL, Perry RE, Schreiman JS, Cheng SC, Frick MP. The reproducibility of measuring the anorectal angle in defecography. Dis Colon Rectum 1991;34:51-5. [Crossref] [PubMed]
- Santoro GA, Wieczorek AP, Shobeiri SA, Mueller ER, Pilat J, Stankiewicz A, Battistella G. Interobserver and interdisciplinary reproducibility of 3D endovaginal ultrasound assessment of pelvic floor anatomy. Int Urogynecol J 2011;22:53-9. [Crossref] [PubMed]
- Lalwani N, Moshiri M, Lee JH, Bhargava P, Dighe MK. Magnetic resonance imaging of pelvic floor dysfunction. Radiol Clin North Am 2013;51:1127-39. [Crossref] [PubMed]
- Dietz HP, Bernardo MJ, Kirby A, Shek KL. Minimal criteria for the diagnosis of avulsion of the puborectalis muscle by tomographic ultrasound. Int Urogynecol J 2011;22:699-704. [Crossref] [PubMed]
- Dietz HP, Pattillo Garnham A, Guzmán Rojas R. Is it necessary to diagnose levator avulsion on pelvic floor muscle contraction? Ultrasound Obstet Gynecol 2017;49:252-6. [Crossref] [PubMed]
- Dietz HP, Garnham AP, Rojas RG. Is the levator-urethra gap helpful for diagnosing avulsion? Int Urogynecol J 2016;27:909-13. [Crossref] [PubMed]
- García-Mejido JA, Bonomi-Barby MJ, Armijo-Sánchez A, Borrero-Fernández C, Castro-Portillo L, Vargas-Broquetas M, Cañadas-Granados M, Sainz-Bueno JA. Metodología para el estudio ecográfico transperineal del suelo pélvico. Clin Invest Ginecol Obstet 2020;48:190-5. [Crossref]
- Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986;1:307-10. [Crossref] [PubMed]
- Goei R, van Engelshoven J, Schouten H, Baeten C, Stassen C. Anorectal function: defecographic measurement in asymptomatic subjects. Radiology 1989;173:137-41. [Crossref] [PubMed]
- Penninckx F, Debruyne C, Lestar B, Kerremans R. Intraobserver variation in the radiological measurement of the anorectal angle. Gastrointest Radiol 1991;16:73-6. [Crossref] [PubMed]
- Yang X, Partanen K, Farin P, Ji H, Soimakallio S. Reproducibility of five anorectal morphologic measurements in defecography. Acad Radiol 1994;1:224-8. [Crossref] [PubMed]
- Kruyt RH, Delemarre JB, Doornbos J, Vogel HJ. Normal anorectum: dynamic MR imaging anatomy. Radiology 1991;179:159-63. [Crossref] [PubMed]
- Bartolo DC, Paterson HM. Anal incontinence. Best Pract Res Clin Gastroenterol 2009;23:505-15. [Crossref] [PubMed]


