
Haglund’s syndrome: a case description
Introduction
Haglund’s syndrome is a common cause of heel pain that remains poorly understood in the clinic. Haglund’s deformity specifically refers to a bony bump (Haglund’s lesion) of the posterosuperior calcaneus. It is also commonly known as ‘retrocalcaneal exostosis’ and ‘pump bump’, terms which were first coined by Patrick Haglund in 1928 (1). Haglund’s syndrome refers to a series of symptoms caused by impingement of Haglund’s deformity, bursa, and Achilles tendon. It is difficult to differentiate between Haglund’s syndrome and other causes of heel pain. Imageology is of great value in the diagnosis of Haglund’s syndrome. Magnetic resonance imaging (MRI) can determine the site, extent, and severity of heel pain and assist with identifying the etiology due to its superior soft tissue contrast and multiplanar imaging, which is of great significance in guiding clinical diagnosis and treatment. Here, we report a case of a patient with Haglund’s syndrome, including the follow-ups after surgical treatment.
Case presentation
A 52-year-old female, with no previous surgical history, presented with bilateral heel pain, which had been present for more than 2 years and had become aggravated within the past 3 days (especially the right ankle).
Physical examination
A visible and palpable ‘pump bump’ on both posterior heels, with redness, local heat, swelling, tenderness, and a decreased range of motion was observed.
Laboratory tests
The results of laboratory tests [routine blood tests, biochemistry, coagulation, and rheumatoid factor (RF)] were within the normal ranges.
Imaging findings
Plain radiographs
On a lateral heel radiograph in a standing position (right), a parallel pitch line (PPL) was used to determine the prominence of the bony bump (Haglund’s deformity). The lower pitch line was tangent to the medial tuberosity and anterior tubercle of the calcaneus. The upper line was drawn parallel to the lower line, tangent to the posterior lip of the articular facet. A bony bump above the upper PPL was abnormal, denoted as +PPL. The projection bone cortex was intact. There was an increased density of the posterior soft tissues at the level of the Achilles tendon insertion (Figure 1A).
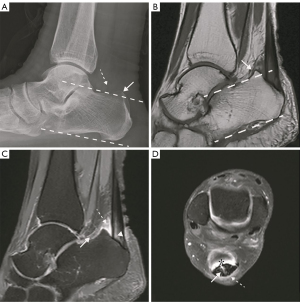
MRI
A sagittal T1-weighted non-fat suppressed image of the right ankle showed a bony bump on the posterosuperior calcaneus (Figure 1B). Sagittal (Figure 1C) and axial (Figure 1D) proton density-weighted (PD) fat suppression images showed abnormally increased PD signal intensity in the region of retrocalcaneal and retro-Achilles bursae, indicating retrocalcaneal and retro-Achilles bursitis, respectively. Furthermore, the region of insertion of the Achilles tendon showed thickening (10 mm) and was partially torn. Moreover, the adjacent soft tissue showed slight edema.
The combination of the above examination results supported the diagnosis of Haglund’s Syndrome (2,3).
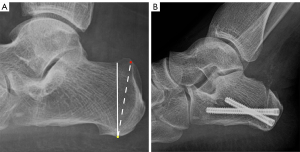
Treatment
The patient received surgical treatment, as conservative treatment is not effective for more than 6 months (4). A closing wedge calcaneal osteotomy was performed. For proper correction, the orientation, angle, and width of the wedge must be predefined based on the preoperative lateral radiograph (Figure 2A). The dorsal exit point of the posterior arm was at the middle of the posterior superior prominence. The plantar exit point of the posterior arm was posterior to the plantar calcaneal tubercle. The anterior arm was approximately 90° to the planta starting at the plantar calcaneal tubercle. Preserving the attachment of the Achilles tendon is important during the operation. The surgical technique was as follows. After administration of general anesthesia, an oblique incision under the lateral malleolus, about 5 cm long, was made. The ankle joint was plantar flexed, and the Achilles tendon and the bony bump were identified by sharp and blunt dissection. The surgical findings were as follows: A bony bump about 5 cm × 4 cm in size at the posterosuperior calcaneus and Achilles tendon thickening with high tension and which was partially torn at the insertion were found. The proliferative and inflammatory retrocalcaneal bursa was cleared, and then the superior aspect of the tuberosity was removed with an osteotome, until there was no obvious impact between the posterosuperior calcaneus and the Achilles tendon at dorsiflexion. The wedge calcaneal osteotomy was guided by C-arm imaging. The wedge was completed with the longer blade. Osteotomy guide pins were placed from lateral to medial for linear and parallel cuts. A threaded Kirschner wire was used to aid wedge removal, and then reduction forceps were used to connect the calcaneal tubercle closely with the calcaneal body. Under C-arm imaging guidance, two 5.5 mm (length 55 and 40 mm) titanium hollow screws (made by Double Medical Technology Inc., Xiamen, China) were cannulated in the direction of the cuboid bone and subtalar joint (Figure 2B). Postoperatively, the patient was advised to avoid weightbearing for a period of 6 weeks.
Follow-up
The patient recovered well after the operation and was walking normally 3 months later.
All procedures performed in this study were in accordance with the ethical standards of the institutional Ethics Committee of the First Hospital of Hunan University of Chinese Medicine (No. HN-LL-KY-2021-019-01) and with the Helsinki Declaration (as revised in 2013). Written informed consent was provided by the patient for publication of this case report and the accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Haglund’s syndrome refers to a series of symptoms (Achilles tendinosis, retrocalcaneal bursitis, retro-Achilles bursitis, and a ‘pump-bump’) caused by impingement of Haglund’s deformity, bursa, and the Achilles tendon. It is a common cause of heel pain and often occurs in middle-aged women, often bilaterally. Haglund’s syndrome is clinically characterized by a prominent swelling with chronic pain and signs of inflammation, including redness, tenderness, and warmth at the posterosuperior calcaneus (5-7). However, the clinically detected pump-bump is not diagnostic of Haglund’s syndrome, as it may mimic other heel pain caused by other diseases such as systemic arthropathies, including rheumatoid arthritis and Reiter’s syndrome. Imageology is of great value for the diagnosis of Haglund’s syndrome.
Haglund’s syndrome is characterized radiographically by a bony bump with intact cortical, retrocalcaneal bursitis, retro-Achilles bursitis, Achilles tendinitis (degeneration or tear), and adjacent soft tissue edema (1).
A plain radiograph in a lateral standing position is helpful to assess the posterosuperior calcaneus bony bump of the calcaneum, the Haglund’s deformity. Some radiographic assessment methods have been proposed since Haglund’s deformity was first described in 1928. Conventional X-ray measurement methods, namely PPL, calcaneal pith angle (CPA), and Fowler-Philip angle (FPA) are commonly used in clinical practice (8-10). To date, researchers have designed and perfected many new radiographic measurements for the diagnosis of Haglund’s deformity, such as X/Y calcaneal ratio, but more research is required to validate these approaches (11,12). However, a plain radiograph does not show changes of adjacent soft tissue. An MRI allows superior soft tissue contrast and multiplanar imaging, is noninvasive, and can clearly display the shape and signal of calcaneus, Achilles tendon, and surrounding structures, and it can be helpful for diagnosis and presurgical planning (7).
Conservative treatments such as training modification (eccentric exercise), extra-corporeal shock wave therapy (ESWT), nonsteroidal anti-inflammatory medication (NSAIDs), and electrotherapy (microcurrent and microwave), are the first choices for patients with Haglund’s syndrome (13-16). Surgery is recommended when conservative treatment has been ineffective after at least 6 months (4,17,18).
In summary, Haglund’s syndrome is one of the clinical causes of heel pain but is poorly understood, and it is difficult to differentiate clinically from other conditions. It is essential to distinguish focal from systemic causes of heel pain. Imageology plays an important role in the diagnosis of Haglund’s syndrome.
Acknowledgments
Funding: This study received funding from the National Natural Science Foundation of China (No. 81603482), the Hunan Natural Science Foundation (No. 2016JJ6115), the China Postdoctoral Science Foundation (No. 2017M622586), the Hunan Province Science and Technology Talent Support Project - Young Outstanding Science and Technology Worker Training Program (No. 2022TJ-N05), the Key Discipline Construction Project of Hunan University of Chinese Medicine (No. 4901-020000200806), and the Hunan Province “Domestic First-class Cultivation Discipline” Open Fund Project of Integrated Traditional Chinese and Western Medicine (No. 2020ZXYJH62).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-22-736/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional ethics committee of the First Hospital of Hunan University of Chinese Medicine (No. HN-LL-KY-2021-019-01) and with the Helsinki Declaration (as revised in 2013). Written informed consent was provided by the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Pavlov H, Heneghan MA, Hersh A, Goldman AB, Vigorita V. The Haglund syndrome: initial and differential diagnosis. Radiology 1982;144:83-8. [Crossref] [PubMed]
- Vaishya R, Agarwal AK, Azizi AT, Vijay V. Haglund's Syndrome: A Commonly Seen Mysterious Condition. Cureus 2016;8:e820. [Crossref] [PubMed]
- Xu JH, Ding SL, Chen B, Wu SC. Modified Bunnell suture expands the surgical indication of the treatment of Haglund's syndrome heel pain with endoscope. Exp Ther Med 2018;15:4817-21. [Crossref] [PubMed]
- Maffulli N, Longo UG, Kadakia A, Spiezia F. Achilles tendinopathy. Foot Ankle Surg 2020;26:240-9. [Crossref] [PubMed]
- Rodríguez-Sanz D, Tovaruela-Carrión N, López-López D, Palomo-López P, Romero-Morales C, Navarro-Flores E, Calvo-Lobo C. Foot disorders in the elderly: A mini-review. Dis Mon 2018;64:64-91. [Crossref] [PubMed]
- López-López D, Pérez-Ríos M, Ruano-Ravina A, Losa-Iglesias ME, Becerro-de-Bengoa-Vallejo R, Romero-Morales C, Calvo-Lobo C, Navarro-Flores E. Impact of quality of life related to foot problems: a case-control study. Sci Rep 2021;11:14515. [Crossref] [PubMed]
- Narváez JA, Narváez J, Ortega R, Aguilera C, Sánchez A, Andía E. Painful heel: MR imaging findings. Radiographics 2000;20:333-52. [Crossref] [PubMed]
- Lu CC, Cheng YM, Fu YC, Tien YC, Chen SK, Huang PJ. Angle analysis of Haglund syndrome and its relationship with osseous variations and Achilles tendon calcification. Foot Ankle Int 2007;28:181-5. [Crossref] [PubMed]
- Singh R, Rohilla R, Siwach RC, Magu NK, Sangwan SS, Sharma A. Diagnostic significance of radiologic measurements in posterior heel pain. Foot (Edinb) 2008;18:91-8. [Crossref] [PubMed]
- Bulstra GH, van Rheenen TA, Scholtes VA. Can We Measure the Heel Bump? Radiographic Evaluation of Haglund's Deformity. J Foot Ankle Surg 2015;54:338-40. [Crossref] [PubMed]
- Tourné Y, Baray AL, Barthélémy R, Moroney P. Contribution of a new radiologic calcaneal measurement to the treatment decision tree in Haglund syndrome. Orthop Traumatol Surg Res 2018;104:1215-9. [Crossref] [PubMed]
- Tang SC, Tu KC, Liao WJ, Hsu CT, Shih HT, Tung KK, Wu MH, Wang SP. Novel Radiographic Measurements for Operatively Treated Haglund's Deformity. Tomography 2022;8:284-92. [Crossref] [PubMed]
- Rhim HC, Kim MS, Choi S, Tenforde AS. Comparative Efficacy and Tolerability of Nonsurgical Therapies for the Treatment of Midportion Achilles Tendinopathy: A Systematic Review With Network Meta-analysis. Orthop J Sports Med 2020;8:2325967120930567. [Crossref] [PubMed]
- Longo UG, Ronga M, Maffulli N. Achilles Tendinopathy. Sports Med Arthrosc Rev 2018;26:16-30. [Crossref] [PubMed]
- Silbernagel KG, Hanlon S, Sprague A. Current Clinical Concepts: Conservative Management of Achilles Tendinopathy. J Athl Train 2020;55:438-47. [Crossref] [PubMed]
- van der Vlist AC, Winters M, Weir A, Ardern CL, Welton NJ, Caldwell DM, Verhaar JAN, de Vos RJ. Which treatment is most effective for patients with Achilles tendinopathy? A living systematic review with network meta-analysis of 29 randomised controlled trials. Br J Sports Med 2021;55:249-56. [Crossref] [PubMed]
- López-López D, Becerro-de-Bengoa-Vallejo R, Losa-Iglesias ME, Palomo-López P, Rodríguez-Sanz D, Brandariz-Pereira JM, Calvo-Lobo C. Evaluation of foot health related quality of life in individuals with foot problems by gender: a cross-sectional comparative analysis study. BMJ Open 2018;8:e023980. [Crossref] [PubMed]
- Yuen WLP, Tan PT, Kon KKC. Surgical Treatment of Haglund's Deformity: A Systematic Review and Meta-Analysis. Cureus 2022;14:e27500. [Crossref] [PubMed]


