
The “impossibly difficult airway” for anesthesiologists and otolaryngologists: a case description
Introduction
The management of difficult airways (DAs) with dyspnea is important for patients with advanced tumors of the oropharynx and neck. The American Society of Anesthesiologists’ (ASA) guidelines for the management of DAs emphasize the use of multiple techniques, including facemask ventilation, the awake intubation algorithm, surgical cricothyrotomy/tracheostomy, and extracorporeal membrane oxygenation (ECMO) (1). Practitioners and patients are assisted by the various guidelines for the management of DAs. However, there is a lack of published evidence examining whether implementing airway algorithms changes clinical practice or patient outcomes. Moreover, there is a lack of consensus on which airway management approaches should be endorsed. Therefore, we still need to refine and update the guidelines for the management of DAs. To date, various challenging cases have been reported and solved by anesthesiologists and otolaryngologists, although differences exist in the techniques and strategies used for the management of DAs (2-5). However, the descriptions of the specific DA types, which have not been successfully resolved by anesthesiologists and otolaryngologists except through ECMO, have not been incorporated into standard protocols. Individual airway management is distinctive in patients with DAs. Clinical decision-making is supported by preoperative imaging studies and airway evaluation.
We present a case of a DA that was not successfully resolved by anesthesiologists and otolaryngologists. The imaging studies of the DA of the case are analyzed and explained in detail. Based on our relevant analysis, we recommend implementing ECMO and a multidisciplinary approach when a patient presents with acute dyspnea and advanced neck tumors. We also recommend that neck computed tomography (CT) be used to identify DAs similar to that observed in our case.
Case presentation
In January 2021, a 47-year-old male patient (180 cm; 80 kg) presented at the First Hospital, China Medical University with dyspnea and dysphagia. He had a 2-month history of a progressively enlarging right cervical mass. He also had a history of hypertension and hepatitis B but no heart and cerebrovascular diseases. He was diagnosed with dyspnea associated with oropharyngeal and neck masses.
After reviewing the neck CT scan (27 January 2021), continuous low-flow oxygen, vital sign monitoring, methylprednisolone, Mucosolvan, and antibiotics were administered. The patient developed severe dyspnea and orthopnea 3 hours post-admission. Subsequently, he was scheduled to undergo emergency endotracheal intubation or tracheotomy to maintain airway patency in the operating room.
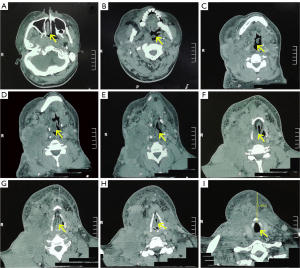
His initial vital signs in the operating room were as follows: blood pressure, 170/95 mmHg; heart rate, 110 beats/min; and peripheral oxygen saturation, 99%. Based on the neck CT findings, the anesthesiologists found that the right side of the epiglottis and the piriform fossa, and the posterior pharyngeal walls, were invaded by a diffuse mass. The oropharyngeal space was deviated to the left, above the glottis plane (Figure 1A-1F), but the glottis was without obvious tumor invasion (Figure 1G,1H). Further, the airway in the subglottic plane was unobstructed and had no obvious stenosis (Figure 1I). Awake fiberoptic bronchoscope (FOB) nasal intubation under topical airway anesthesia was considered.
Preoperatively, the patient was administered penehyclidine hydrochloride (1 mg) and methylprednisolone (80 mg) intravenously. Additionally, continuous 100% oxygen was administered, and invasive blood pressure measurement was performed. Then, topical anesthesia (1% tetracaine) was provided through an atomizer. Various airway devices (facemask, laryngeal mask airway, direct laryngoscopy, video-assisted laryngoscopy, FOB, Shikani optical stylet, rigid bronchoscope, and airway exchange catheter) were also available. The first attempt (awake FOB nasal intubation) was unsuccessful due to secretions, distortions in the anatomy, and dyspnea. The patient suddenly lost consciousness and entered pulmonary arrest. Epinephrine and atropine were administered, and cardiopulmonary resuscitation was performed. The facemask ventilation, laryngeal mask airway, video-assisted laryngoscopy, FOB, and tracheostomy were unsuccessful.
Finally, the anesthesiologists and otolaryngologists placed a rigid bronchoscope in the airway, inserted an airway exchange catheter, and used this to facilitate the successful placement of a 7.0 endotracheal tube. Postoperatively, the patient exhibited unstable vital signs and a high probability of brain injury caused by the continuous hypoxemia that lasted for 50 minutes.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was provided by the family member of patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Despite the recommendations from the ASA standard guidelines, there is substantial heterogeneity in the management of DAs. For example, although the presence of a large multinodular goiter, awake FOB has been successfully used to secure the DA (2). In a case of severe tracheal stenosis, a bilateral superficial cervical plexus block with dexmedetomidine sedation has also been used (3). Although it is essential to adhere to international guidelines, each case must be assessed individually to enable the most suitable course of management for each DA to be selected.
In our case, trained anesthesiologists and otolaryngologists, different airway devices, and rigorous vital signs monitoring were initially available. Considering the signs and symptoms indicative of a DA and the neck CT in this patient, awake FOB intubation was considered. Awake cricothyroidotomy/tracheostomy and ECMO were also considered for this patient. In one report, awake tracheostomy was recommended to secure the airway with a sizable malignant thyroid tumor, leading to a glottis aperture of 3×5 mm and dislocation of the larynx to the left (4). However, in our case, awake cricothyroidotomy/tracheostomy was challenging due to the diffuse mass (about 7.091 cm from the trachea to the skin), bleeding tendency, and distorted anatomy. In another report, ECMO was recommended in a case of severe airway stenosis (4.9 mm at the narrowest portion) (5). However, in our case, it was also difficult to perform ECMO due to the expensive cost and its questionable feasibility in patients with malignant tumors.
In some circumstances, for the predicted impossible airways, ECMO might represent a safer option to maintain oxygenation (6). ECMO can secure a definitive airway in a controlled environment for patients with severe airway obstruction (7). Nevertheless, the use of ECMO has not been incorporated into standard guidelines because the types of DAs that it is suitable for remain unclear. Kim et al. (8) recommended that ECMO be performed if the tracheal patency is less than 5 mm. However, in our case, the patient experienced a bad outcome even though we followed the guidelines and implemented an appropriate strategy. Airway patency is challenging to maintain when there are structural variations in the oropharyngeal space in the upper airway, even when consciousness and spontaneous ventilation are maintained. Awake FOB in this patient may not have been successful on the first attempt because any stimulation could cause spasms and complete the airway obstruction. Therefore, the patient’s survival might have improved if ECMO had been used before airway intervention. This makes ECMO a suitable method of solving dyspnea in palliative care for patients with advanced tumors of the oropharynx and neck.
In conclusion, the prior use of ECMO should be seriously considered before attempting airway intervention for patients similar to the presentation in the current case who have DAs caused by acute dyspnea and advanced neck tumors, as shown by CT. Moreover, the safe management of DAs is best achieved through a multidisciplinary approach, including anesthesiologists, otolaryngologists, and radiologists, among other specialists.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-22-507/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was provided by the family member of patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Apfelbaum JL, Hagberg CA, Connis RT, Abdelmalak BB, Agarkar M, Dutton RP, Fiadjoe JE, Greif R, Klock PA, Mercier D, Myatra SN, O'Sullivan EP, Rosenblatt WH, Sorbello M, Tung A. 2022 American Society of Anesthesiologists Practice Guidelines for Management of the Difficult Airway. Anesthesiology 2022;136:31-81. [Crossref] [PubMed]
- Kaur H, Kataria AP, Muthuramalingapandian M, Kaur H. Airway Considerations in Case of a Large Multinodular Goiter. Anesth Essays Res 2017;11:1097-100. [Crossref] [PubMed]
- Cho AR, Kim HK, Lee EA, Lee DH. Airway management in a patient with severe tracheal stenosis: bilateral superficial cervical plexus block with dexmedetomidine sedation. J Anesth 2015;29:292-4. [Crossref] [PubMed]
- Hohn A, Kauliņš T, Hinkelbein J, Kauliņa K, Kopp A, Russo SG, Kohlen S, Schröder S. Awake tracheotomy in a patient with stridor and dyspnoea caused by a sizeable malignant thyroid tumor: a case report and short review of the literature. Clin Case Rep 2017;5:1891-5. [Crossref] [PubMed]
- Ikeda Y, Saito Y, Kadomura T, Yamada R, Shibuya S, Itoh H, Ishiwa D, Tsuji K, Nagashima Z, Segawa S. Extracorporeal membrane oxygenation for the anesthetic management of a patient with severe airway stenosis caused by thyroid carcinoma invasion. Surg Today 2021;51:2000-5. [Crossref] [PubMed]
- Law JA, Duggan LV, Asselin M, Baker P, Crosby E, Downey A, Hung OR, Kovacs G, Lemay F, Noppens R, Parotto M, Preston R, Sowers N, Sparrow K, Turkstra TP, Wong DT, Jones PMCanadian Airway Focus Group. Canadian Airway Focus Group updated consensus-based recommendations for management of the difficult airway: part 2. Planning and implementing safe management of the patient with an anticipated difficult airway. Can J Anaesth 2021;68:1405-36. [Crossref] [PubMed]
- Malpas G, Hung O, Gilchrist A, Wong C, Kent B, Hirsch GM, Hart RD. The use of extracorporeal membrane oxygenation in the anticipated difficult airway: a case report and systematic review. Can J Anaesth 2018;65:685-97. [Crossref] [PubMed]
- Kim CW, Kim DH, Son BS, Cho JS, Kim YD. I H, Ahn HY. The Feasibility of Extracorporeal Membrane Oxygenation in the Variant Airway Problems. Ann Thorac Cardiovasc Surg 2015;21:517-22. [Crossref] [PubMed]


