
Osteoporotic-like vertebral fracture with less than 20% height loss is associated with increased further vertebral fracture risk in older women: the MrOS and MsOS (Hong Kong) year-18 follow-up radiograph results
Introduction
The bone composition of the spine, which is predominantly trabecular bone, is prone to the thinning and microarchitectural changes associated with osteoporosis. Osteoporotic vertebral fracture (OVF) is the most common osteoporotic fracture. Assessment of OVF status, in addition to bone mineral density (BMD), provides important information to aid in predicting fracture risk in older women and men. It is important to identify OVF, so that appropriate investigation, prevention, and treatment can be instigated, both for women and men. However, the clinical relevance of ‘minimal’ grade (<20% vertebral height loss, i.e., Genant grade 0.5) OVF or ‘mild’ grade OVF has not been well clarified (1,2). Some ‘milder’ OVF can also be clinically relevant. Siris et al. (3) reported that at any given BMD T-score, the risk of incident vertebral, non-vertebral, and any fracture depended heavily on prevalent radiographic OVF status. Johansson et al. (4) reported that, in older women and after adjustment for clinical risk factors and BMD, Genant grade 1 OVFs identified on lateral spine imaging with dual-energy x-ray absorptiometry are associated with incident major osteoporotic fractures. In the Canada-wide STeroid-Associated Osteoporosis in the Pediatric Population (STOPP) study, Alos et al. (5) noted that the presence of Genant grade 1 vertebral fracture (VF) at baseline (BL) in children with leukemia was independently associated with an increased risk of new fractures in the first 12 months following chemotherapy initiation.
We argued that, though minimal grade OVFs may not have immediate further fragility fracture consequences, they can be a biomarker of compromised bone quality (2). In a recent study conducted among older women, we reported among 38 vertebrae in 27 cases which had anterior wedging deformity with height loss of <20% while without radiographic endplate depression, 28 vertebrae (28/38, 73.7%) demonstrated endplate depression on computed tomography (CT), thus suggesting these deformities were more likely to be osteoporotic (6). In our osteoporotic fractures in women (MsOS) (Hong Kong) year-14 follow-up (FU), out of 150 female participants, five women were identified as having BL minimal osteoporotic-like vertebral fracture (OLVF). There was a trend that these minimal OLVF subjects had incident VF risk similar to that of the subjects with BL apparent OLVF (i.e., ≥20% height loss), higher than female subjects without BL OLVF (7).
Osteoporotic fractures in men (MrOS) and MsOS (Hong Kong) represents the first large-scale prospective cohort study conducted on bone health in East Asians. At BL, 2,000 Chinese men and 2,000 Chinese women ≥65 years were recruited from the local communities from August 2001 to March 2003. The recruitment criteria were structured so that the study results from the cohort would be applicable to a broad population of similarly aged community-dwelling men and women. The BL, year-4 FU, and year-14 FU radiographic OVF characteristics of MrOS (Hong Kong) and MsOS (Hong Kong) participants have been published (7-11). Hereby we present the year-18 spine radiograph FU results. For the current study, we were particularly interested in whether, after a longer period of FU, women with ‘minimal’ grade OLVF had a higher incident VF risk than those without BL OLVF.
Methods
The study cohort
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study protocol was approved by the Chinese University of Hong Kong Ethics Committee. Written informed consent was obtained from all subjects. During December 2019 to December 2021, a year-18 FU was carried out with invitations sent to all contactable MrOS (Hong Kong) and MsOS (Hong Kong) subjects. Spine radiography was performed on 146 male participants (62.7% of men who attended this round of FU) and 156 female participants (66.1% of women who attended this round of FU), who were willing to participate. Two male cases with insufficient radiograph quality were not included in the final analysis. Among these participants, 81 males and 51 females have also had the year-14 FU spine imaging. Anti-osteoporosis medication history was checked among the participants for radiography, nine women had taken anti-osteoporosis medication at some time points during the FU. At BL, femoral neck, total hip, and lumbar spine areal BMDs were measured with a QDR-4500W densitometer (Hologic Inc., Waltham, MA, USA).
Radiographic analysis of OVF
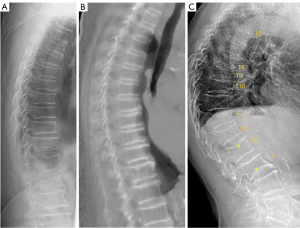
The digitalized format of radiographs was available for analysis. Both the BL and year-18 FU radiographs were read simultaneously for each subject (thus, the BL radiographs were re-read). Thoracic and lumbar vertebrae (T4–L5) were evaluated for OVF with an extended version of Genant semi-quantitative (SQ) method with the following criteria (12): (I) minimal grade refers to radiological OVF with <20% height loss, which would be theoretically equivalent to SQ grade 0.5; the diagnosis of this grade rely on a distinct fracture-like change of a vertebra’s morphology (as compared with its expected shape considering those of the neighboring vertebrae); (II) mild grade is the same as Genant SQ mild grade (≥20–25% height loss); (III) SQ moderate grade is divided into two subgrades: ≥25%–1/3 height loss and ≥1/3–40% height loss; (IV) SQ severe grade is divided into two subgrades: ≥40%–2/3 height loss and with ≥2/3 height loss (collapsed grade). SQ moderate grade is subdivided into two grades because vertebral deformities (VDs) with >1/3 height loss are always associated with positive endplate and/or cortex fracture (ECF) sign radiographically (2,13). A subdivision of SQ grade 3 facilitates the recording of severe OVF progression (such as a 45% height loss progresses to 75% height loss). In this study, the term ‘OLVF’ is used for OVF, as only based on spine radiograph it is not possible to diagnose a VD as OVF absolutely in every case. Non-fractural changes of the vertebrae shape were evaluated to systematically exclude deformities such as developmental changes and degenerative remodeling (2,14-16). None of the spines was diagnosed as having pathological fractures or diseases other than degenerative or osteoporotic change.
Acquired short vertebra (aSV) was defined as with decreased vertebral anterior and middle heights, while without anterior wedging and bi-concave changes, i.e., middle height and anterior height were reduced to the same extent (2,6). These aSVs did not include those with known causes of degenerative osteoarthritis (2,17) and congenital causes (18). Only those with at least two adjacent aSVs were recorded as aSV cases. Degenerative osteoarthritis of vertebrae, also mostly involving multiple vertebrae, can cause reduced vertebral height, but typically appears anteriorly wedged without endplate depression, and often accompanied by osteophytes and disc space narrowing (2,17). A congenital short vertebra usually has unique shapes morphologically and can be accompanied by compensating overgrow of neighboring vertebrae (14,18).
The primary reading was conducted by an experienced reader (YXJW), and then compared with the earlier BL readings. A further second reading was provided by a trained biomedical engineer. The final diagnosis was made in consensus, with discussion among involved readers.
Criteria for incident VF and VF progression
To define the progression of a BL OLVF, a further height decrease of at least 15% vertebral height was required. A new incident VF was defined as a qualitative OLVF occurred in a vertebra that was not deformed at BL (i.e., grade 0), and which could be either a change from grade 0 at BL to mild grade OLVF or above (mostly with ≥15% height loss) at FU, or a change from grade 0 at BL to minimal OLVF with the appearance of ECF during FU. Both OLVF progression and incident OLVF were considered ‘incident VF’. To avoid over-diagnosis, a change from grade 0 at BL to minimal OLVF without a radiographic ECF sign during FU was not considered a new fracture incident.
Statistical analysis
In this study, after considering there was no high-energy trauma event history and the morphology of the involved vertebrae, the OLVFs and incident VFs were assumed to be osteoporotic cause. Data were processed using GraphPad Software (GraphPad Software Inc. San Diego, CA, USA). Continuous variables were tested by Mann-Whitney U test, and categorical variables were analyzed by chi-square test or Fisher exact test. Tests were two-sided. A P value of less than 0.05 was considered statistically significant.
Results
At year-18 FU, the mean (± standard deviation) age was 87.4±3.1 years for males and 87.0±3.2 years for females. The prevalence of OLVF at FU timepoint is shown in Figure 1A. Males had more minimal or mild grade OLVFs, and while females had more severer grade OLVFs. For females had OLVF of >1/3 height loss, the chance of having multiple OLVFs per case increased (Figure 1B).

As there were few subjects in each OLVF subcategory, reading results were grouped into grade 0, minimal OLVF (with <20% vertebral height loss), and apparent OLVF (with ≥20% vertebral height loss), and the results are shown in Table 1. For subjects without BL OLVF, 12.5% of males and 27.1% of females (P<0.0001) had incident VF by year-18, indicating female’s incident VF rate was twice as much as that of males. In those with apparent OLVF at BL, female’s incident VF rate was three times as much as that of males (66.7% vs. 20%, P=0.005). For females, subjects with minimal OLVF (n=27, all did not have ECF sign) had incident VF risk during FU similar to the subjects with BL apparent OLVF, higher than female subjects without BL OLVF (59.3% vs. 27.1%, P=0.0015). Compared with the subjects without BL OLVF, female subjects with BL minimal OLVF had an odds ratio of 3.9 (95% CI: 1.6–9.3) of developing incident VF. For both males and females, subjects with apparent BL OLVF had a lower mean hip BMD at BL than those without OLVF. Moreover, female subjects with minimal BL OLVF had a lower mean BL hip BMD than those without OLVF (0.716±0.109 vs. 0.773±0.105 g/cm2, P=0.012).
Table 1
| Baseline OLVF grading | Males (n=144) | Females (n=156) | |||||
|---|---|---|---|---|---|---|---|
| Grade 0 (no OLVF) | Minimal OLVF* | Apparent OLVF | Grade 0 (no OLVF)¶ | Minimal OLVF*¶ | Apparent OLVF¶ | ||
| Case, n (%) | 104 (72.2) | 20 (13.9) | 20 (13.9) | 114 (73.1) | 27 (17.3) | 15 (9.6) | |
| Incident VF shown at year-18 | 12.5% (13/104)A,B,K | 20% (4/20)A,C | 20% (4/20)B,C,L | 27.1% (31/114)D,E,K | 59.3% (16/27)D,F | 66.7% (10/15)E,F,L | |
| BL age (years) no incident VF cases | 68.8±2.8 | 67.9±3.1 | 70.7±4.8 | 68.7±3.3 | 69.7±2.9 | 68.6±3.5 | |
| BL age (years) with Incident VF cases | 68.2±2.8 | 66±0.82 | 69.8±1.5 | 69.4±3.1 | 70.1±2.4 | 68.4±3.1 | |
| BL hip BMD all cases in the grade | 0.897±0.108H | 0.882±0.088 | 0.837±0.140H | 0.773±0.105I,J | 0.716±0.109I | 0.683±0.074J | |
| BL hip BMD no Incident VF cases | 0.903±0.107G | 0.876±0.094 | 0.848±0.134 | 0.770±0.109 | 0.702±0.090 | 0.736±0.046 | |
| BL hip BMD with Incident VF cases | 0.856±0.110G | 0.906±0.062 | 0.791±0.154 | 0.781±0.093 | 0.728±0.126 | 0.636±0.061 | |
| Reported incident VF at year-14§ | 7.9% (18/229) | 8% (2/25) | 17.6% (3/17) | 14.3% (18/126) | 60% (3/5)# | 52.6% (10/19) | |
¶, only nine females had anti-osteoporosis medication during the FU. For grade 0 subjects, five had taken anti-osteoporosis medication, four had no incident VF during FU. For minimal OLVF subjects, two had taken anti-osteoporosis medication, both had incident VF during FU. For apparent OLVF subjects, two had taken anti-osteoporosis medication, with one had incident VF during FU and one did not have incident VF; *, none of the OLVF had endplate and/or cortex fracture sign at baseline; #, out of the year-14 FU five cases with minimal VD at BL, one was also included in year-18 FU; §, data from year-14 FU presented here for reference [see reference (7) for details]. A: P>0.05; B: P>0.05; C: P>0.05; D: P=0.0015; E: P=0.002; F: P>0.05. G: P>0.05; H: P=0.037; I: P=0.012; J: P=0.001; K: P<0.0001; L: P=0.005. Minimal OLVF, OLVF with <20% height loss; apparent OLVF, OLVF with ≥20% height loss. OLVF, osteoporotic-like vertebral fracture; BL, baseline; VF, vertebral fracture; BMD, bone mineral density; FU, follow-up.
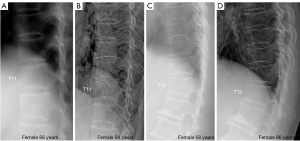
Multiple aSVs cases are shown in Table 2 (Figure 2 shows an example). Multiple aSVs prevalence among females was not higher than that among males. For males and females, there were 6 cases (4.5%, 6/133) and 3 cases (2.1%, 3/142) respectively developed aSV during FU. For both males and females, subjects with aSV tended to have lower BMD measures (measured at BL) that those without aSV. Subjects with aSVs were more likely to be associated with OLVF at BL. However, subjects with aSVs did not demonstrate increased incident fracture risk during the FU for other vertebrae, both for males and females. For males with and without aSV, 11.8% and 15% have incident fracture of other vertebrae. For females with and without aSV, 35.3% and 34.5% have incident fracture of other vertebrae.
Table 2
| Gender | Study subjects | No aSVs | With aSVs |
|---|---|---|---|
| Males, BL assessment | Proportion of cases at BL | 92.4% (133/144) | 7.6% (11/144)¶ |
| Mean age at BL (years) | 68 | 69.5 | |
| Femoral neck BMD at BL (P=0.096)# | 0.708±0.101 | 0.666±0.66 | |
| Total hip BMD at BL (P=0.337)# | 0.889±0.112 | 0.858±0.110 | |
| Lumbar spine BMD at BL (P=0.169)# | 0.954±0.145 | 0.905±0.90 | |
| Males, FU assessment | Proportion of cases at FU | 88.2% (127/144) | 11.8% (17/144) |
| Mean age at FU (years) | 87.3 | 88.5 | |
| % cases with no OLVF at BL (P=0.002)# | 76.4% (97/127) | 41.2% (7/17) | |
| % cases with minimal OLVF at BL (P=0.049)# | 11.8% (15/127) | 29.4% (5/17) | |
| % cases with apparent OLVF at BL (P=0.049)# | 11.8% (15/127) | 29.4% (5/17) | |
| % cases, 18 years FU period had no incident VF | 85.% (108/127) | 88.2% (15/17) | |
| % cases, 18 years FU period had incident VF | 15.0% (19/127) | 11.8% (1/17) | |
| Females, BL assessment | Proportion of cases at BL | 91.0% (142/156) | 9.0% (14/156)¶ |
| Mean age at BL (years) | 68.9 | 70.2 | |
| Femoral neck BMD at BL (P=0.282)# | 0.623±0.103 | 0.593±0.080 | |
| Total hip BMD at BL (P=0.173)# | 0.756±0.108 | 0.738±0.099 | |
| Lumbar spine BMD at BL (P=0.591)# | 0.786±0.146 | 0.767±0.105 | |
| Females, FU assessment | Proportion of cases at FU | 89.1% (139/156) | 10.9% (17/156) |
| Age at FU (years) | 86.9 | 87.8 | |
| % cases with no OLVF at BL (P=0.002)# | 76.3% (106/139) | 41.2% (7/17) | |
| % cases with minimal OLVF at BL (P=0.001)# | 14.4% (20/139) | 47.1% (8/17) | |
| % cases with apparent OLVF at BL (P=0.750)# | 9.4% (13/139) | 11.8% (2/17) | |
| % cases, 18 years FU period had no incident VF | 65.5% (91/139) | 64.7% (11/17) | |
| % cases, 18 years FU period had incident VF | 34.5% (48/139) | 35.3% (6/17) |
(P)#, comparing the cases with aSV and cases without aSV; ¶, for males, 11 case (64.7%) had short vertebrae at baseline, for females, 14 case (82.4%) had short vertebrae at baseline. This indicates for males and females, there were 6 cases and 3 cases respectively developed aSV during FU. BL, baseline; FU, follow-up; OLVF, osteoporotic-like vertebral fracture; VF, vertebral fracture; BMD, bone mineral density (unit, gram/cm2); aSVs, acquired short vertebrae.
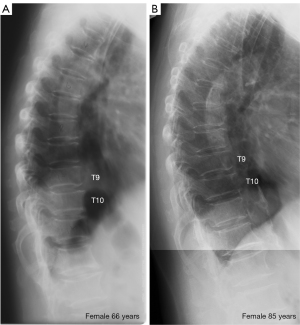
In five male cases, recovery from minimal or mild grades OLVF to normal shape was observed in five vertebrae (one vertebra/case). Recovery from minimal OLVF to normal shape was observed in four vertebrae in four female cases (Figure 3, one vertebra/case). None of these subjects reported anti-osteoporosis medication.
Discussion
The most important strength of this study is its long FU period, and this study was performed on subjects of very advanced age. Men and women of similar age and from the same community-based population were investigated using the same methodology. Despite the limited number of participants, this study provides clinically relevant insights into the pathophysiology of OVF among elderly populations. One of the most important findings of this study is that minimal grade OLVF in older females was associated with increased further VF risk. Minimal OLVF without ECF sign was seen among 27 females at BL, and among them 16 cases (59.3%) had incident VF during FU, which was higher than those without OLVF (27.1%) and close to those with apparent OLVF (66.7%). Female subjects with minimal OLVF also had a BL mean hip BMD lower than those without OLVF at BL. This result supports our earlier year-14 FU result though that study had fewer minimal OLVF cases (Table 1). This is also consistent with our recent report that, among older females, the majority of anterior wedging deformities with height loss of <20% were osteoporotic fracture (6). At FU, males had a higher proportion of minimal and mild grades OLVFs, while females had a higher proportion of severer grades OLVFs (Figure 1A). This is also consistent with the known male-female OVF difference (19).
It is also interesting that, among the 156 female cases, we were able to identify 27 cases who had ECF sign negative minimal grade OLVF and had a lower BMD on average at BL, and among them 16 cases had incident VF during FU. This result contrasts with other reports favoring all OVFs should demonstrate endplate fracture. Our results on minimal grade OLVF should be understood considering these three points: (I) as we noted earlier (2), osteoporotic OVFs without achieving 20% height loss threshold (i.e., grade 0.5) have been commonly classified as Genant grade 1 OVF by colleagues trained in University of California at San Francisco (UCSF), USA, thus, some of our minimal grade OLVFs could be classified as Genant grade 1 OLVF by other readers if the 20% height loss threshold is not strictly followed; (II) our study had a very long FU period of 18 years; (III) due to our experience in the area of OVF assessment, we trust we have been geared to identify true OVFs while excluding other OVF mimics. It is possible some other reports on OVF could be contaminated by OVF mimics (2,20-22).
One of the goals of the current study is to analyze whether multiple aSVs is an osteoporosis phenomenon. The definition of aSV in this study is likely to be different from other reports (23,24), since common mimics have been excluded already in this study and according to our definition, aSV should not be wedging or bi-concave shaped. An illustration of the differentiation of multiple aSVs and multiple OVFs is further demonstrated in Figure 4. In one our earlier study (11), analyzing four elderly female cases with of 2, 2, 3, 3 adjacent aSVs (per case) respectively, it was shown that all these 10 vertebrae did not have endplate depression on CT, instead aSV could be associated with osteoarthritic/endplate inflammatory changes. On the other hand, distinct singular aSV may be an appearance of OVF (2,6). In another recent study we analyzed thoracic spine among 408 female patients and 374 male patients who had lateral chest radiographs unrelated to spine disorders, we noted that among the in total 449 male and female cases aged ≤34 years, there was only one female case had multiple aSVs (note aSVs commonly occur in thoracic spine rather than lumbar spine). For the group ≥45 years, 15.6% of males (mean age: 54.8 years) had multiple aSVs while only 1.5% of the females (mean age: 50.2 years) had multiple aSVs (18). Based on the demographics of the subjects, we suggested that physical labor such as weight-bearing could be associated with multiple aSVs (18). With our current study we had a few relevant observations. Firstly, multiple aSVs prevalence among females was not higher than that of males, which was consistent with our earlier results. Assuming Hong Kong residents had less chance of weight-bearing labor history, and the males in this study were much older than the older group subjects in our earlier study (88.2 vs. 50.2 years), the lower short vertebras (SVs) prevalence among Hong Kong males [11.8% vs. 15.6% (18)] further supports that physical labor could be associated with an increased prevalence of aSVs. Both for males and females, a trend of lower mean BMD was noted for subjects with aSVs than those without aSVs. It is probably not surprising that multiple aSVs were associated with other OLVFs, assuming low energy trauma and weakened bone quality, etc. may facilitate the development of aSVs. On these aspects, it may look counterintuitive that in this study the subjects with multiple aSVs did not demonstrate an increased incident fracture risks during the FU for other vertebrae. This could be due to the limited sample size. Overall, taking together the evidence described above, we may suggest multiple aSVs itself is ‘primarily’ not an osteoporosis phenomenon (particularly considering its prevalence is not higher among females), and not ‘strongly’ associated with increased fracture risk for other vertebrae. On the other hand, multiple aSVs more likely occur among low BMD subjects than among normal bone strength subjects.
In our report on adolescents and middle-aged subjects, we suggest that fracture shaped vertebral deformity (FSVD), which we postulate are due to micro-fracture associated with physical stress, can repair and heal (18). However, that was not a study with FU. Radiographs from the current study with direct evidence confirmed that, even among older subjects, OLVF repairs (Figure 3). Thus, OLVF repairing, healing, and maybe then re-fracture, likely constitute a continuous and dynamic process. However, we expect the OLVF repairing and healing are under-documented in the current study. It is difficult to confirm some partial levels of recovery. Some OLVFs might have maintained their severity unchanged due to the repairing and healing process, i.e., their severity would have progressed if without repairing and healing.
There are a number of limitations to this study. The primary limitation of this study is its limited sample size. For males, few VF incidences occurred both in the minimal OLVF group and in the apparent OLVF group, thus statistical difference cannot be meaningfully assessed. The participants in this study were slightly younger than the BL average (at BL, approximately 68.8 years in this study vs. approximately 72.5 years for the mean). The participants in this study are expected to be healthier and more mobile than the cohort BL averages. Considering the advanced age of the participants, this would be an unavoidable bias toward healthier subjects who were more likely to participate in this study. Nine women had taken anti-osteoporosis medication, thus theoretically they should be excluded from the analysis. However, the number of participants who had taken anti-osteoporosis medication was small and the regularity of their medication-taking could not be confirmed (more likely the medication was irregular), we consider that excluding them will not alter the conclusion of this study. We did not quantitatively evaluate multiple aSV progression during the FU period. While this study suggests multiple aSVs were not strongly associated with increased incident VF risk for other vertebrae, further studies investigating the clinical relevance of multiple aSVs are desirable. In this study, the same as other literature, after excluding OVF mimics, the OLVFs and incident VFs were assumed to be osteoporotic cause. However, milder FSVD and mild incident radiographic VF can also occasionally occur in subjects with normal bone strength (18). However, statistically speaking, the fracture shaped vertebral deformities and incident VFs in our older subjects were more likely to be osteoporotic fracture, and our results should be considered in statistical sense.
Conclusions
In conclusions, 144 males and 156 females of MrOS and MsOS (Hong Kong) study participants had spine radiography at year-18 FU. For subjects without BL OLVF, females’ incident VF rate was twice that of males, while for subjects with apparent BL OLVF, females’ incident VF rate was three times that of males. Older females with BL minimal OLVF have increased incident VF risk. Multiple aSVs more likely occur among lower BMD subjects than among normal bone strength subjects, but the multiple aSVs phenomenon is not strongly associated with increased incident VF risk. This study demonstrated that OLVF among older subjects can repair and heal.
Acknowledgments
Dr. Min Deng and Mr. Ben-Heng Xiao, both with Department of Imaging and Interventional Radiology, the Chinese University of Hong Kong, provided additional OLVF readings and discussions during the course of this study.
Funding: This study was supported by Hong Kong ITSP project (No. ITS/334/18).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-2022-06/coif). YXJ Wáng serves as the Editor-in-Chief of Quantitative Imaging in Medicine and Surgery. He is the founder of Yingran Medicals Ltd., which develops medical image-based diagnostics software. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study protocol was approved by the Chinese University of Hong Kong Ethics Committee. Written informed consent was obtained from all subjects.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Lentle B, Koromani F, Brown JP, Oei L, Ward L, Goltzman D, Rivadeneira F, Leslie WD, Probyn L, Prior J, Hammond I, Cheung AM, Oei EH. Vertebral Fracture Research Groups of the CaMos, STOPP, and Rotterdam Studies. The Radiology of Osteoporotic Vertebral Fractures Revisited. J Bone Miner Res 2019;34:409-18. [Crossref] [PubMed]
- Wáng YXJ. An update of our understanding of radiographic diagnostics for prevalent osteoporotic vertebral fracture in elderly women. Quant Imaging Med Surg 2022;12:3495-514. [Crossref] [PubMed]
- Siris ES, Genant HK, Laster AJ, Chen P, Misurski DA, Krege JH. Enhanced prediction of fracture risk combining vertebral fracture status and BMD. Osteoporos Int 2007;18:761-70. [Crossref] [PubMed]
- Johansson L, Sundh D, Magnusson P, Rukmangatharajan K, Mellström D, Nilsson AG, Lorentzon M. Grade 1 Vertebral Fractures Identified by Densitometric Lateral Spine Imaging Predict Incident Major Osteoporotic Fracture Independently of Clinical Risk Factors and Bone Mineral Density in Older Women. J Bone Miner Res 2020;35:1942-51. [Crossref] [PubMed]
- Alos N, Grant RM, Ramsay T, Halton J, Cummings EA, Miettunen PM, et al. High incidence of vertebral fractures in children with acute lymphoblastic leukemia 12 months after the initiation of therapy. J Clin Oncol 2012;30:2760-7. [Crossref] [PubMed]
- Du EZ, Wáng YXJ. CT detects more osteoporotic endplate depressions than radiograph: a descriptive comparison of 76 vertebrae. Osteoporos Int 2022;33:1569-77. [Crossref] [PubMed]
- Wáng YXJ, Che-Nordin N, Leung JCS, Man Yu BW, Griffith JF, Kwok TCY. Elderly men have much lower vertebral fracture risk than elderly women even at advanced age: the MrOS and MsOS (Hong Kong) year 14 follow-up radiology results. Arch Osteoporos 2020;15:176. [Crossref] [PubMed]
- Kwok AW, Gong JS, Wang YX, Leung JC, Kwok T, Griffith JF, Leung PC. Prevalence and risk factors of radiographic vertebral fractures in elderly Chinese men and women: results of Mr. OS (Hong Kong) and Ms. OS (Hong Kong) studies. Osteoporos Int 2013;24:877-85. [Crossref] [PubMed]
- Deng M, Zeng XJ, He LC, Leung JCS, Kwok AWL, Griffith JF, Kwok T, Leung PC, Wáng YXJ. Osteoporotic Vertebral Fracture Prevalence in Elderly Chinese Men and Women: A Comparison of Endplate/Cortex Fracture-Based and Morphometrical Deformity-Based Methods. J Clin Densitom 2019;22:409-19. [Crossref] [PubMed]
- Wáng YXJ, Che-Nordin N, Deng M, Leung JCS, Kwok AWL, He LC, Griffith JF, Kwok TCY, Leung PC. Osteoporotic vertebral deformity with endplate/cortex fracture is associated with higher further vertebral fracture risk: the Ms. OS (Hong Kong) study results. Osteoporos Int 2019;30:897-905. [Crossref] [PubMed]
- Wáng YXJ, Che-Nordin N, Deng M, Griffith JF, Leung JCS, Kwok AWL, Leung PC, Kwok TCY. Elderly males with or without existing osteoporotic vertebral fracture have much lower future vertebral fracture risk than elderly females: the MrOS (Hong Kong) year-4 follow-up spine radiograph study. Osteoporos Int 2019;30:2505-14. [Crossref] [PubMed]
- Wáng YXJ, Diacinti D, Yu W, Cheng XG, Nogueira-Barbosa MH, Che-Nordin N, Guglielmi G, Ruiz Santiago F. Semi-quantitative grading and extended semi-quantitative grading for osteoporotic vertebral deformity: a radiographic image database for education and calibration. Ann Transl Med 2020;8:398. [Crossref] [PubMed]
- Deng M, Kwok TCY, Leung JCS, Leung PC, Wáng YXJ. All osteoporotically deformed vertebrae with >34% height loss have radiographically identifiable endplate/cortex fracture. J Orthop Translat 2018;14:63-6. [Crossref] [PubMed]
- Wáng YXJ, Santiago FR, Deng M, Nogueira-Barbosa MH. Identifying osteoporotic vertebral endplate and cortex fractures. Quant Imaging Med Surg 2017;7:555-91. [Crossref] [PubMed]
- Wáng YXJ. Osteoporotic Vertebral Deformity: Radiological Appearances and Their Association With a History of Trauma and the Risk of Further Fragility Fracture. Can Assoc Radiol J 2021;72:585. [Crossref] [PubMed]
- Wáng YXJ, Deng M, He LC, Che-Nordin N, Santiago FR. Osteoporotic vertebral endplate and cortex fractures: A pictorial review. J Orthop Translat 2018;15:35-49. [Crossref] [PubMed]
- Abdel-Hamid Osman A, Bassiouni H, Koutri R, Nijs J, Geusens P, Dequeker J. Aging of the thoracic spine: distinction between wedging in osteoarthritis and fracture in osteoporosis--a cross-sectional and longitudinal study. Bone 1994;15:437-42. [Crossref] [PubMed]
- Ma JB, Wáng YX. Prevalence of vertebral deformity among young and middle-aged population of mixed city dwellers and rural residents. J Thorac Dis 2022; [Crossref]
- Wáng YXJ, Lentle BC. Radiographic osteoporotic vertebral fractures in elderly men: a brief review focusing on differences between the sexes. Quant Imaging Med Surg 2020;10:1863-76. [Crossref] [PubMed]
- Lentle BC, Prior JC. Osteoporotic vertebral fracture (OVF): diagnosis requires an informed observer. Osteoporos Int 2022;33:1409-10. [Crossref] [PubMed]
- Lentle BC, Berger C, Brown JP, Probyn L, Langsetmo L, Hammond I, Hu J, Leslie WD, Prior JC, Hanley DA, Adachi JD, Josse RG, Cheung AM, Kaiser SM, Towheed T, Kovacs CS, Wong AKO, Goltzman D. Vertebral Fractures: Which Radiological Criteria Are Better Associated With the Clinical Course of Osteoporosis? Can Assoc Radiol J 2021;72:150-8. [Crossref] [PubMed]
- Wáng YXJ, Wang XR, Che-Nordin N, Xu FR, Huang QL. On the possibility of over-diagnosis of osteoporotic vertebral fracture at mid-thoracic level. J Thorac Dis 2019;11:5708-11. [Crossref] [PubMed]
- Ferrar L, Jiang G, Cawthon PM, San Valentin R, Fullman R, Lambert L, Cummings SR, Black DM, Orwoll E, Barrett-Connor E, Ensrud K, Fink HA, Eastell R. Osteoporotic Fractures in Men (MrOS) Study. Identification of vertebral fracture and non-osteoporotic short vertebral height in men: the MrOS study. J Bone Miner Res 2007;22:1434-41. [Crossref] [PubMed]
- Ferrar L, Jiang G, Armbrecht G, Reid DM, Roux C, Glüer CC, Felsenberg D, Eastell R. Is short vertebral height always an osteoporotic fracture? The Osteoporosis and Ultrasound Study (OPUS). Bone 2007;41:5-12. [Crossref] [PubMed]


