Use of 100 kV versus 120 kV in computed tomography pulmonary angiography in the detection of pulmonary embolism: effect on radiation dose and image quality
Introduction
After myocardial ischemia and stroke, pulmonary embolism (PE) is the third most common cause of cardiovascular death. Untreated chronic PE leads to an increase in morbidity and mortality (1). Currently, multislice computed tomography (CT) angiography is the first-line imaging modality for the diagnosis of patients with suspected PE, as it is safe, highly accurate and cost-effective (2-5). Previous studies have shown that CT pulmonary angiography (CTPA) has significantly increased the diagnostic accuracy in the detection of sub-segmental PE in clinical practice due to the improved spatial and temporal resolution that is available with multislice CT scanners (6-9).
The expanding use of multislice CT has also resulted in an increase in the frequency of procedures and radiation exposure to the patient compared to single-slice CT (10). This is due to the increased availability and shorter scan time as well as the fact that it can also be used to evaluate the mediastinal and parenchymal structures. High radiation dose associated with CTPA has raised serious concerns in the literature, and this is especially important in young female patients, who represent approximately 20% of the patients examined and may receive a substantial amount of radiation to their breast tissues (11,12). Thus, there is a need to reduce the radiation dose in patients, especially in those with low clinical probability of PE.
Low kilovoltage (kV) scanning has been widely applied in CT angiography as it better matches the effective energy of the X-ray beam to the maximum absorption that is close to the k-edge of iodine. Therefore, the low kV technique improves vascular enhancement by substantially increasing the relative vascular attenuation (in CT numbers) of contrast material and at the same time reduces radiation dose (13-15). The chest is an anatomic region that is well suited for the use of low kV techniques because of less-attenuating tissue in the lungs (11).
A low kV (80 or 100 kV) has been confirmed to be an effective technique for reduction of radiation dose in cardiac CT angiography and CTPA compared with the standard 120 kV protocol (16-18). Unlike previous studies which used relatively fixed mAs when applying the low kV protocol, we determined the effective mAs for the low kV protocol when compared to the standard protocol during CTPA examinations. The purpose of this study was to prospectively compare CTPA at a low kV (100 kV) with the standard 120 kV protocol on a 16-slice CT scanner, in terms of image quality assessment and radiation dose comparison. Despite the use of 16-slice CT scanner in this study, results were considered to have clinical value in minimizing radiation dose during CTPA examinations, in particular for some clinical centres in developing countries where 16-slice CT is still commonly used.
Materials and methods
Patient population
This study was approved by the local ethical research committee, and written informed consent was obtained from all patients before undergoing the procedure. Sixty-six patients (age range, 19-87 years, mean age 52.8 years) weighing ≤70 kg with clinical suspicion of PE was consecutively recruited for CTPA. Patients were excluded if they were under 18 years old, unable to hold their breath for at least 20 s, pregnant women and those with nephropathy and hypersensitivity to contrast media.
Group A consisting of 33 patients (age range, 17-86 years, mean age 50.8±18.9 years) was examined using 100 kV protocol, and group B comprising 33 patients (age range, 25-86 years, mean age 54.8±17.4 years) was examined using the standard 120 kV protocol. Patient demographics and comparisons of both groups are demonstrated in Table 1.
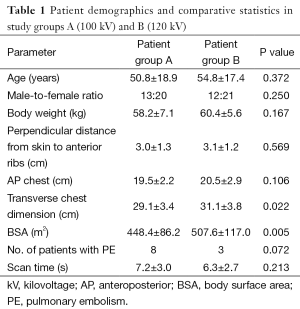
Full table
CT scanning protocol
All CTPA examinations were performed on a 16-slice CT scanner (Siemens Medical Systems, Muenchen, Germany). In both groups, 80-100 mL of non-ionic contrast medium (Iopamiro 370 Iopromide, Schering, Berlin, Germany) was injected onto the ante-cubital vein at 3-4 mL/s, and the scan was performed with a bolus tracking technique (Smart Prep) with a CT attenuation of 100 Hounsfield unit (HU) as the triggering threshold at right ventricle to initiate the scan.
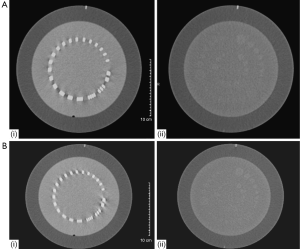
The scanning protocol for 16-slice CTPA was as follows: beam collimation 16 mm × 0.75 mm, gantry rotation of 0.42 s, table feed of 18 mm (pitch 1.5), slice thickness of 5.0 mm, reconstruction interval of 2.0 mm, with tube voltage of 120 kV and effective mAs (mAs/pitch) of 90. For the low dose 100 kV protocol, the value of effective mAs was determined by a phantom study (CATPHAN@ 500, Phantom Laboratory, Salem, NY, USA) (19). Using the 120 kV and 90 mAs as the standard reference, the 100 kV protocol was tested with a wide range of mAs, ranging from 70 to 135 mAs (Table 2). It was shown that 115 mAs was the most suitable one for the low dose CTPA as the image quality in terms of spatial and contrast resolution obtained based on this protocol is similar to that from the standard 120 kV protocol (Figure 1).
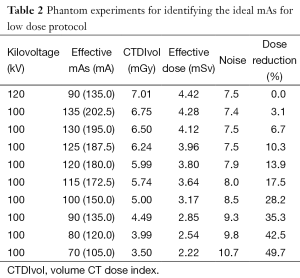
Full table
Quantitative measurement of image quality
To evaluate attenuation in the central pulmonary arteries, signal intensity (SI) (CT number in HU) was measured in the main pulmonary artery (MPA) by using a region of interest of at least 1.0 cm2 (±0.5 cm2). The maximum SI of peripheral pulmonary arteries was also evaluated close to the beginning and the end of each scan in a segmental or sub-segmental artery at an apical and a basal section. The maximum CT number was used as a proxy for vascular attenuation because the caliber of the peripheral vessels was too small to reliably set an intraluminal region of interest to determine the mean CT number.
Objective quantification of the image noise was measured in terms of the standard deviation (SD) in three homogeneous regions of interest measuring about 1.0 cm2 (±0.5 cm2) in the MPA that was free of motion or contrast material—induced artifacts.
The signal-to-noise ratio (SNR) was determined by dividing mean SImain pulmonary vessel with SD, while contrast-to-noise ratio (CNR) was calculated by dividing contrast enhancement (CT attenuation at the MPA minus CT attenuation at the paraspinal muscles) with image noise, that is, CNR = SImean pulmonary vessel−SImuscle/background noise. Background noise refers to the SD measured at the MPA.
Qualitative analysis of image quality
Two senior radiologists with more than 10 years of experience performed consensus interpretation of the CT images. Images were presented in random order to the observers who were blinded to the scanning protocols and patient details. After reviewing several previous studies, the reviewers predetermined the pulmonary artery settings based on consensus and used a window width (WW) between 1,200 and 1,400 and window level (WL) between 400 and 700 in order to compensate for increased attenuation within the pulmonary arteries at low kV setting. The mediastinum, liver and lungs were assessed in the mediastinal (WW 450, WL 100) and lung (WW 1,500; WL −500) window settings.
Images were subjectively assessed using a five-point scale ranging from 1 to 5:
- A score of 1: very poor image quality with no diagnostic information;
- A score of 2: low image quality that reduces the confidence in making diagnosis;
- A score of 3: moderate image quality sufficient to make diagnosis;
- A score of 4: good image quality clearly demonstrating anatomical structures;
- A score of 5: excellent image quality enabling excellent differentiation of even small anatomical structures.
The degree and effect of image noise and motion artefacts (MA) were similarly graded using a five-point scale with score 1 indicating massive artefacts, not possible to make diagnosis; score 2 marked artefacts, still not possible to make diagnosis; score 3 moderate artefacts, able to make diagnosis; score 4 mild artefacts, sufficient to make diagnosis; and score 5 no artefacts. Different anatomical areas were combined to rate the image noise and presence of MA only once per examination.
The degree of contrast enhancement of pulmonary arteries was also graded by using a five-point scale, and the subjective contrast enhancement score was determined by evaluating the main pulmonary arteries. A score of 1 indicating no enhancement, 2 slight enhancement, 3 good enhancement, 4 sufficient and 5 excellent enhancement.
Radiation dose measurements
Volume CT dose index (CTDIvol) and dose length product (DLP) was provided by the scanner console. Effective radiation dose was calculated by multiplying the DLP of the chest scan by a conversion coefficient (k =0.017 mSv/mGy/cm).
Statistical analysis
Continuous variables were presented as mean ± SD. Data analysis was performed by using SPSS version 17.0 (SPSS V17.0, Chicago, ILL). A Chi-square test was used to compare the sex distribution in both groups. The student t-test and one-way analysis of variance were used to analyse the multi-factor interactions. A P value of less than 0.05 was considered statistical significance.
Results
CTPA examinations in both groups were successfully performed in this study without any complications. A total of 792 segmental arteries (396 each in group A and group B) were analyzed. The percentage of segmental arteries that were considered to have sufficient quality for assessment of PE did not significantly differ between group A (mean, 91%±15%) and group B (mean, 91%±7%) (P=0.85).
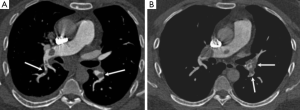
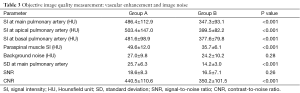
Both central pulmonary arteries (measured in the MPA) and peripheral arteries showed significantly higher enhancement with the 100 kV protocol than with the standard 120 kV protocol as shown in Figure 2. The mean CT attenuation in the MPA was 486±112.9 HU in group A, which is significantly higher than the 347.3±93.1 HU in group B (P<0.001), as shown in Figure 3.
In the peripheral pulmonary arteries at the level of the aortic arch and lung base, the maximum CT attenuation was 503.4±147.0 HU and 481.6±98.9 HU for group A, 399.5±82.2 HU and 377.6±79.8 HU for group B, with significant difference reached between these two groups (P<0.001) (Table 3).
Full table
Quantification of image noise and artefacts
Image noise measured at the central pulmonary arteries in group A was significantly higher than that in group B, as shown in Table 3. There was no significant difference in SNR between the group A and group B (P=0.26), however, the CNR measured in group A was significantly higher than that in group B (P<0.001).
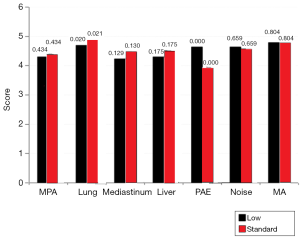
There was no significant difference for the subjective grading of image noise (mean score, 4.6 vs. 4.6; P=0.659) or of MA (mean score, 4.8 vs. 4.8; P=0.804) for the images acquired with 100 and 120 kV protocols, respectively. A summary of these findings are demonstrated in Figure 4.
Assessment of image quality
A consensual agreement was made between both of the reviewers for evaluation of image quality. Subjective scores for image quality were lower for the 100 kV protocol than for the 120 kV protocol, while the vascular enhancement was higher in the 100 kV protocol but the difference between the average scores were not significant.
Differences in subjective scoring did not reach significant differences for any of the five anatomic areas (MPA: P=0.43; lungs: P=0.02; mediastinum: P=0.13; liver parenchyma: P=0.18), except in the pulmonary artery enhancement (PAE), which is statistically significant different (P<0.001).
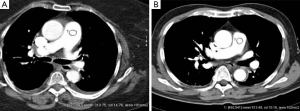
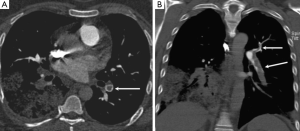
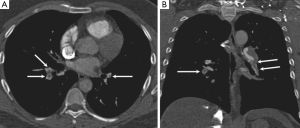
None of the CTPA scans was considered to have such low image quality that it would interfere with diagnosis (grades 1 or 2) for the anatomic regions evaluated. Figures 5 and 6 demonstrate the comparison of image quality at the central and peripheral pulmonary arteries between the two protocols.
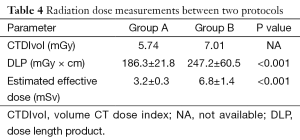
Patient radiation exposure
There was a significant difference noted in the DLP and estimated effective dose between group A and group B, with corresponding DLP of 186.3±21.8 mGycm and 247.2±60.5 mGycm, respectively; P<0.001), and estimated effective dose of 3.2±0.4 mSv vs. 6.8±1.4 mSv, respectively (P<0.001). The low kV protocol leads to an average reduction of estimated effective dose of approximately 53% (Table 4).
Full table
Discussion
The most important finding of this study is that a CTPA protocol with low tube voltage (100 kV) results in higher attenuation of the central and peripheral pulmonary arteries than a standard protocol. The low dose protocol produces a diagnostic confidence of PE detection that is not significantly different from the standard protocol, but using 53% less radiation dose.
With the rapid developments of CT techniques, CTPA was initially used as an adjunct and an alternative to other imaging modalities (20), and recently it is widely recognized as the method of choice for diagnosis of suspected PE due to its superior sensitivity and specificity to ventilation-perfusion isotope scanning (21,22). However the overall radiation dose has also been increased due to the extended scan ranges and to compensate for the increasing image noise in thin-section imaging. This has become a major concern among radiologists and physicians about keeping the radiation dose at minimum levels (23,24). Several dose-saving strategies have been proposed for reducing the radiation dose of CTPA, such as tube current modulation, lower kV, use of high-pitch protocol and application of shielding (9,10). The use of low kV protocols for CTPA has been increasingly investigated in the literature (10-14,16-18). Results of this study are in line with previous reports showing that improved vascular enhancement was achieved for both central and peripheral pulmonary arteries using 100 kV protocols (25,26). Although the image noise was higher in the low dose protocol due to a reduction in the total energy flux than that in the standard protocol, the SNR and CNR were slightly higher in the low dose group with improvement in image quality for the visualisation of pulmonary vessels, and this is also consistent with other studies (11,27).
This study was different from previous studies as a phantom study was conducted first to compensate for the increased noise that would be expected from reducing the tube current. The purpose of this preliminary study was to ensure that the images obtained with the low dose protocol would be of diagnostic quality while achieving reduction of radiation exposure. Thus, the radiation dose with the low dose protocol in this study is even lower than that acquired with a high-pitch 128-slice CT, as reported in a recent study (186.3 vs. 289.5 mGycm) (28). However, the effective dose of 3.2 mSv in this study is still higher than the 1.1 and 2.7 mSv with use of 80 and 100 kV protocols, according to a recent study by Viteri-Ramírez et al. based on dual-source CT imaging (29). Furthermore, iterative reconstruction (IR) is a recently introduced algorithm which has been confirmed to be an effective strategy in reducing image noise while improving image quality with significant reduction of radiation dose in CT scans (30-32). A combination of high-pitch protocol with low kVp and IR in CTPA examination has been found to reduce radiation dose by 52%, with contrast volume of 20 mL used in the low-dose protocol (33,34). Thus, there is still room for further reduction of radiation dose associated with CTPA.
Body weight and body mass index (BMI) are directly proportional to image noise and inversely related to arterial enhancement (35,36). Image noise increases with the increase of the body weight, whereas arterial enhancement decreases accordingly, and this is especially apparent in the peripheral vascular imaging. The two groups in this study were matched by gender, age, body weight and body surface area (BSA), thus precluding possible variations between the two groups in the vascular enhancement due to a different body habitus. This leaves the contrast medium administration (volume, concentration, injection rate) as the main factor directly associated with PAE (37). This study shows that 80-100 mL of non-ionic contrast medium delivered at 3-4 mL/s in 16-slice CT allows diagnostic image quality, however, the amount of contrast medium is more than the 60 mL of iodinated contrast medium used in 64-slice CT systems (29). It has been suggested that a combination of low kV with a decreased volume of contrast medium leads to increased vascular contrast enhancement (27,38), therefore, further studies are needed to focus on reduction of contrast medium while recommending a low dose protocol.
Some limitations in this study should be addressed. First, the study was performed on a 16-slice CT scanner, which is slower in terms of gantry rotation time than that of the recent models such as dual-source CT or 320-slice CT systems. Despite this limitation, sufficient image quality was acquired with both protocols at central and peripheral pulmonary arteries. The global trend in multislice CT imaging is that latest models such as dual-source CT or 256- or 320-slice CT scanners are increasingly installed in many clinical centers, however, 16-slice CT still plays an important role in daily clinical practice, especially in developing countries. Second, the number of patients with PE was low. Thus, the effect of 100 kV in PE detectability cannot be inferred from the present data. However, increased attenuation was observed at the peripheral pulmonary vessels with use of the low dose protocol, and this indicates that the diagnostic accuracy won’t be compromised even down to the level of segmental pulmonary arteries. Third, this low dose protocol was limited to individuals weighing ≤70 kg and may not be suitable for larger patients as increased image noise may deteriorate the image quality.
In conclusion, this study demonstrates that pulmonary CT angiography performed with 100 kV protocol results in a significant reduction in the radiation dose with high attenuation of the central and peripheral pulmonary arteries. Further studies should be conducted to investigate the diagnostic value of the low dose protocol in detecting segmental and subsegmental pulmonary emboli based on more advanced CT scanners.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Wittram C, Maher MM, Yoo AJ, Kalra MK, Shepard JA, McLoud TC. CT angiography of pulmonary embolism: diagnostic criteria and causes of misdiagnosis. Radiographics 2004;24:1219-38. [PubMed]
- Remy-Jardin M, Pistolesi M, Goodman LR, Gefter WB, Gottschalk A, Mayo JR, Sostman HD. Management of suspected acute pulmonary embolism in the era of CT angiography: a statement from the Fleischner Society. Radiology 2007;245:315-29. [PubMed]
- Perrier A, Roy PM, Sanchez O, Le Gal G, Meyer G, Gourdier AL, Furber A, Revel MP, Howarth N, Davido A, Bounameaux H. Multidetector-row computed tomography in suspected pulmonary embolism. N Engl J Med 2005;352:1760-8. [PubMed]
- Righini M, Le Gal G, Aujesky D, Roy PM, Sanchez O, Verschuren F, Rutschmann O, Nonent M, Cornuz J, Thys F, Le Manach CP, Revel MP, Poletti PA, Meyer G, Mottier D, Perneger T, Bounameaux H, Perrier A. Diagnosis of pulmonary embolism by multidetector CT alone or combined with venous ultrasonography of the leg: a randomised non-inferiority trial. Lancet 2008;371:1343-52. [PubMed]
- Stein PD, Fowler SE, Goodman LR, Gottschalk A, Hales CA, Hull RD, Leeper KV Jr, Quinn DA, Sos TA, Sostman HD, Tapson VF, Wakefield TW, Weg JG, Woodard PK. PIOPED II Investigators. Multidetector computed tomography for acute pulmonary embolism. N Engl J Med 2006;354:2317-27. [PubMed]
- Schoepf UJ, Costello P. CT angiography for diagnosis of pulmonary embolism: state of the art. Radiology 2004;230:329-37. [PubMed]
- Schoepf UJ. Diagnosing pulmonary embolism: time to rewrite the textbooks. Int J Cardiovasc Imaging 2005;21:155-63. [PubMed]
- Hoey ET, Gopalan D, Ganesh V, Agrawal SK, Qureshi N, Tasker AD, Clements L, Screaton NJ. Dual-energy CT pulmonary angiography: a novel technique for assessing acute and chronic pulmonary thromboembolism. Clin Radiol 2009;64:414-9. [PubMed]
- Nikolaou K, Thieme S, Sommer W, Johnson T, Reiser MF. Diagnosing pulmonary embolism: new computed tomography applications. J Thorac Imaging 2010;25:151-60. [PubMed]
- Kalra MK, Prasad S, Saini S, Blake MA, Varghese J, Halpern EF, Thrall JH, Rhea JT. Clinical comparison of standard-dose and 50% reduced-dose abdominal CT: effect on image quality. AJR Am J Roentgenol 2002;179:1101-6. [PubMed]
- Schueller-Weidekamm C, Schaefer-Prokop CM, Weber M, Herold CJ, Prokop M. CT angiography of pulmonary arteries to detect pulmonary embolism: improvement of vascular enhancement with low kilovoltage settings. Radiology 2006;241:899-907. [PubMed]
- Heyer CM, Mohr PS, Lemburg SP, Peters SA, Nicolas V. Image quality and radiation exposure at pulmonary CT angiography with 100- or 120-kVp protocol: prospective randomized study. Radiology 2007;245:577-83. [PubMed]
- Takahashi M, Maguire WM, Ashtari M, Khan A, Papp Z, Alberico R, Campbell W, Eacobacci T, Herman PG. Low-dose spiral computed tomography of the thorax: comparison with the standard-dose technique. Invest Radiol 1998;33:68-73. [PubMed]
- Diederich S, Lenzen H, Windmann R, Puskas Z, Yeibuz TM, Henneken S, Klaiber T, Eameri M, Roos N, Peters PE. Pulmonary nodules: experimental and clinical studies at low-dose CT. Radiology 1999;213:289-98. [PubMed]
- Oguchi K, Sone S, Kiyono K, Takashima S, Maruyama Y, Hasegawa M, Feng L. Optimal tube current for lung cancer screening with low-dose spiral CT. Acta Radiol 2000;41:352-6. [PubMed]
- Park EA, Lee W, Kang JH, Yin YH, Chung JW, Park JH. The image quality and radiation dose of 100-kVp versus 120-kVp ECG-gated 16-slice CT coronary angiography. Korean J Radiol 2009;10:235-43. [PubMed]
- Holmquist F, Nyman U. Eighty-peak kilovoltage 16-channel multidetector computed tomography and reduced contrast-medium doses tailored to body weight to diagnose pulmonary embolism in azotaemic patients. Eur Radiol 2006;16:1165-76. [PubMed]
- Szucs-Farkas Z, Kurmann L, Strautz T, Patak MA, Vock P, Schindera ST. Patient exposure and image quality of low-dose pulmonary computed tomography angiography: comparison of 100- and 80-kVp protocols. Invest Radiol 2008;43:871-6. [PubMed]
- The Phantom Laboratory. Capthan ® Manual. 2005. Available online: http://www.phantomlab.com/products/catphan.php
- British Thoracic Society Standards of Care Committee Pulmonary Embolism Guideline Development Group. British Thoracic Society guidelines for the management of suspected acute pulmonary embolism. Thorax 2003;58:470-83. [PubMed]
- Hayashino Y, Goto M, Noguchi Y, Fukui T. Ventilation-perfusion scanning and helical CT in suspected pulmonary embolism: meta-analysis of diagnostic performance. Radiology 2005;234:740-8. [PubMed]
- Guilabert JP, Manzur DN, Tarrasa MJ, Llorens ML, Braun P, Arques MP. Can multislice CT alone rule out reliably pulmonary embolism? A prospective study. Eur J Radiol 2007;62:220-6. [PubMed]
- Brenner DJ, Hall EJ. Computed tomography--an increasing source of radiation exposure. N Engl J Med 2007;357:2277-84. [PubMed]
- Fazel R, Krumholz HM, Wang Y, Ross JS, Chen J, Ting HH, Shah ND, Nasir K, Einstein AJ, Nallamothu BK. Exposure to low-dose ionizing radiation from medical imaging procedures. N Engl J Med 2009;361:849-57. [PubMed]
- Bahner ML, Bengel A, Brix G, Zuna I, Kauczor HU, Delorme S. Improved vascular opacification in cerebral computed tomography angiography with 80 kVp. Invest Radiol 2005;40:229-34. [PubMed]
- Szucs-Farkas Z, Verdun FR, von Allmen G, Mini RL, Vock P. Effect of X-ray tube parameters, iodine concentration, and patient size on image quality in pulmonary computed tomography angiography: a chest-phantom-study. Invest Radiol 2008;43:374-81. [PubMed]
- Szucs-Farkas Z, Schaller C, Bensler S, Patak MA, Vock P, Schindera ST. Detection of pulmonary emboli with CT angiography at reduced radiation exposure and contrast material volume: comparison of 80 kVp and 120 kVp protocols in a matched cohort. Invest Radiol 2009;44:793-9. [PubMed]
- De Zordo T, von Lutterotti K, Dejaco C, Soegner PF, Frank R, Aigner F, Klauser AS, Pechlaner C, Schoepf UJ, Jaschke WR, Feuchtner GM. Comparison of image quality and radiation dose of different pulmonary CTA protocols on a 128-slice CT: high-pitch dual source CT, dual energy CT and conventional spiral CT. Eur Radiol 2012;22:279-86. [PubMed]
- Viteri-Ramírez G, García-Lallana A, Simón-Yarza I, Broncano J, Ferreira M, Pueyo JC, Villaueva A, Bastarrika G. Low radiation and low-contrast dose pulmonary CT angiography: Comparison of 80 kVp/60 ml and 100 kVp/80 ml protocols. Clin Radiol 2012;67:833-9. [PubMed]
- Leipsic J, Nguyen G, Brown J, Sin D, Mayo JR. A prospective evaluation of dose reduction and image quality in chest CT using adaptive statistical iterative reconstruction. AJR Am J Roentgenol 2010;195:1095-9. [PubMed]
- Singh S, Kalra MK, Gilman MD, Hsieh J, Pien HH, Digumarthy SR, Shepard JA. Adaptive statistical iterative reconstruction technique for radiation dose reduction in chest CT: a pilot study. Radiology 2011;259:565-73. [PubMed]
- Sun Z, Al Moudi M, Cao Y. CT angiography in the diagnosis of cardiovascular disease: a transformation in cardiovascular CT practice. Quant Imaging Med Surg 2014;4:376-96. [PubMed]
- McLaughlin PD, Liang T, Homiedan M, Louis LJ, O’Connell TW, Krzymyk K, Nicolaou S, Mayo JR. High pitch, low voltage dual source CT pulmonary angiography: assessment of image quality and diagnostic acceptability with hybrid iterative reconstruction. Emerg Radiol 2015;22:117-23. [PubMed]
- Lu GM, Luo S, Meinel FG, McQuiston AD, Zhou CS, Kong X, Zhao YE, Zheng L, Schoepf UJ, Zhang LJ. High-pitch computed tomography pulmonary angiography with iterative reconstruction at 80 kVp and 20 mL contrast agent volume. Eur Radiol 2014;24:3260-8. [PubMed]
- Bae KT, Seeck BA, Hildebolt CF, Tao C, Zhu F, Kanematsu M, Woodard PK. Contrast enhancement in cardiovascular MDCT: effect of body weight, height, body surface area, body mass index, and obesity. AJR Am J Roentgenol 2008;190:777-84. [PubMed]
- Bae KT, Tao C, Gürel S, Hong C, Zhu F, Gebke TA, Milite M, Hidelbolt CF. Effect of patient weight and scanning duration on contrast enhancement during pulmonary multidetector CT angiography. Radiology 2007;242:582-9. [PubMed]
- Bae KT. Intravenous contrast medium administration and scan timing at CT: considerations and approaches. Radiology 2010;256:32-61. [PubMed]
- Holmquist F, Hansson K, Pasquariello F, Bjork J, Nyman U. Minimizing contrast medium doses to diagnose pulmonary embolism with 80-kVp multidetector computed tomography in azotemic patients. Acta Radiol 2009;50:181-93. [PubMed]


