Pleural effusion?—Trust your gut
Case presentation
A 16-year-old Caucasian male was referred to the acute medical unit by his general practitioner for suspected community acquired pneumonia. He described a 3-week history of cough productive of white-yellow sputum but denied shortness of breath, chest pain and fever. He was a non-smoker with a past medical history of type 2 diabetes mellitus and Asperger’s syndrome. Notably, he had been diagnosed with irritable bowel syndrome due to longstanding abdominal discomfort and abnormal bowel habits. His vital signs were within normal limits and blood tests were unremarkable. Chest examination revealed equal chest expansion, a central trachea, dullness to percussion and reduced breath sounds at the left lung base. His abdomen was soft and non-tender.
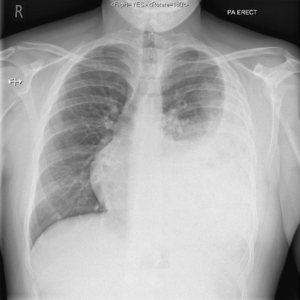
Erect chest radiograph revealed what appeared to be a left pleural effusion (Figure 1). The differential diagnoses were para-pneumonic effusion and malignancy, the latter being unlikely in a young patient with no suggestive symptoms or risk factors.
A thoracic ultrasound scan was performed to confirm the presence of pleural fluid and guide potential aspiration. Surprisingly, it revealed no evidence of pleural effusion but showed diffuse pleural thickening. Consequently, he underwent a thoracic computed tomography scan. This showed almost complete occupation of the left pleural cavity with small bowel, pancreas and large bowel, indicative of a Bochdalek hernia (Figure 2). The patient is awaiting review by the cardiothoracic surgeons for elective surgical repair of the hernia.
Discussion
Bochdalek hernias are congenital diaphragmatic hernias, which result from incomplete fusion of the posterolateral diaphragmatic foramina during development. It was first described in 1848 by Czech anatomist Vincent Alexander Bochdalek (1).
The majority of Bochdalek hernias manifest in the neonatal period on either side of the diaphragm or bilaterally. Most are left sided and contain only fat and omentum. However, herniation of multiple organs has been noted (2,3).
Most patients are asymptomatic throughout their lifetime but a minority present with chronic non-specific symptoms. These range from abdominal pain, postprandial fullness and vomiting, to respiratory symptoms of dyspnea and chest pain (4). Complications include organ strangulation and incarceration, which can present acutely. Chest radiography is not diagnostic in most cases, with varied findings including evidence of a gas filled bowel or soft tissue masses in the lung fields (5). Computed tomography remains the gold standard investigation to reduce misdiagnosis that can occur through radiological mimicry.
If conservative management is unsatisfactory, surgical repair can be considered. The abdominal contents are reduced and the defect repaired either by laparotomy or thoracotomy. Laparoscopic and thoracoscopic repairs have been successful (4).
This case highlights the importance of confirmatory imaging prior to invasive procedures in patients with suspected pleural effusion. Recent guidance from the British Thoracic Society recommends the use of thoracic ultrasound scans to reduce the risk of organ puncture and increase the success rate of pleural fluid aspiration. Bochdalek hernias are common but rarely present in adulthood with non-specific signs and symptoms. If diagnostic imaging is not utilised appropriately, patient safety and standard of care may be inadvertently compromised.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Gedik E, Tuncer MC, Onat S, Avci A, Tacyildiz I, Bac B. A review of Morgagni and Bochdalek hernias in adults. Folia Morphol (Warsz) 2011;70:5-12. [PubMed]
- Hamid KS, Rai SS, Rodriguez JA. Symptomatic Bochdalek hernia in an adult. JSLS 2010;14:279-81. [Crossref] [PubMed]
- Mullins ME, Stein J, Saini SS, Mueller PR. Prevalence of incidental Bochdalek’s hernia in a large adult population. AJR Am J Roentgenol 2001;177:363-6. [Crossref] [PubMed]
- Laaksonen E, Silvasti S, Hakala T. Right-sided Bochdalek hernia in an adult: a case report. J Med Case Rep 2009;3:9291. [Crossref] [PubMed]
- Hung YH, Chien YH, Yan SL, Chen MF. Adult Bochdalek hernia with bowel incarceration. J Chin Med Assoc 2008;71:528-31. [Crossref] [PubMed]