Intrathoracic gastric perforation secondary to corrosive ingestion: a rare complication
Introduction
This case report describes a rare and serious case of acid ingestion in a 50-year-old man who developed necrosis and perforation of gastric fundus and posterolateral aspect of diaphragm with extension of air and fluid collection in the thorax. To the best of our knowledge, this complication has not been described so far in the literature.
Case presentation
A 50-year-old male patient presented with history of accidental ingestion of acid while drinking alcohol, 20 days back. Exact amount of acid consumed was not quantified. Patient also had history of hematemesis (small amount 5-10 mL daily) and dysphagia to solids. Treatment history revealed admission to a private hospital, where endoscopy was done showing evidence of eschar in lower esophagus and fundus of stomach. Chest radiograph taken at that time was normal. But later he developed dyspnoea and on repeat radiograph diagnosis of pyopneumothorax (due to aspiration pneumonia with superimposed infection) was made by the private practitioner.
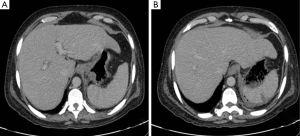
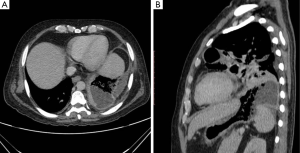
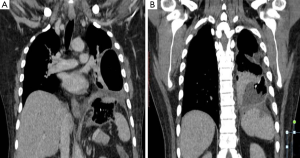
Patient was then admitted in our institute. On examination, patient had decreased air entry on the left side. Contrast enhanced computed tomography (CECT) of chest and upper abdomen was done, which showed non-enhancing wall of gastric fundus (Figure 1) with a collection containing air, fluid and gastric contents extending from fundus to left hemithorax with a defect in the diaphragm (Figures 2,3). There was also collapse consolidation of left lower lobe of lung (Figures 2B,3). Additionally, there was evidence of extraluminal air and fluid in the perisplenic space (Figures 1B,3B). Differential diagnoses of intrathoracic gastric perforation (in extrapleural space) along with the diaphragmatic perforation versus gastropleural fistula due to gastric perforation were given.
Patient was taken for surgery. Peroperatively, wall of gastric fundus was gangrenous with multiple perforations (Figure 4) and there was evidence of collection extending from fundus to left thoracic cavity with associated defect in the left hemidiaphragm. Parietal pleura was normal. Total gastrectomy was done. Histopathological examination of resected stomach showed necrosis of gastric fundus with candida infection. Postoperatively, patient succumbed to acute respiratory distress syndrome likely due to fungal sepsis.
Discussion
Caustic injury due to acid ingestion is an important public health problem occurring in young children or in adults attempting suicide. Acids, in contrast to alkali substances, usually involve stomach sparing the esophagus (in 80% of cases) and cause inflammation and coagulation necrosis of the mucosa that forms an eschar. Early complications include ulceration, bleeding and perforation (due to sloughing of overlying eschar) and late ones are fibrosis and gastric outlet obstruction. The extent of the injury depends on the specifics of the ingestion (volume, concentration and nature of the acid) along with the gastric contents at the time of injury and duration of mucosal contact. With more devastating injuries burns can be found in small bowel, transverse colon, liver, biliary tree, pancreas, spleen and diaphragm (1-3). Though intrathoracic gastric perforation has been described after laparoscopic fundoplication (4) and in cases of diaphragmatic hernia with compromised vascularity, but never has been described as a complication of acid ingestion (5). We hypothesised acid causing necrosis and perforation of gastric fundus and diaphragm as the cause of intrathoracic perforation in our case. The other probable explanation could have been that patient had asymptomatic diaphragmatic hernia and ingestion of acid led to perforation of stomach in the thorax. But, it was not likely as on imaging and peroperatively, the stomach was present beneath the diaphragm and only the collection was extending in the chest.
Symptoms range from burns to lip, mouth and oropharynx to nonspecific complaints like nausea, vomiting, hematemesis, dysphagia, odynophagia and drooling. Patients with severe burns and perforation may present with substernal/abdominal/back pain with rigidity (1).
Investigations include erect chest radiograph with upper abdomen (to detect free air in the mediastinum or under the diaphragm due to esophageal or gastric perforation respectively) and flexible endoscopy (to look for extent of stomach and duodenal injury). Though timing of endoscopy is still controversial, many authors recommend the procedure between 12–48 hours of the ingestion. Computed tomography (CT) is a non-invasive modality, which is particularly helpful to look for abnormalities of esophageal, gastric and duodenal walls and any signs of perforation (extraluminal fluid, pneumomediastinum, pneumoperitoneum and pneumoretroperitoneum). Gangrene should be suspected if normally enhancing mucosa, submucosal and muscular layers are not evident (1,2).
Treatment consists of correction of metabolic disturbances and coagulopathy. Conservative management with nasogastric tube and stent placement is done in mild cases and surgery (like partial or total gastrectomy) is required in cases of perforation or gangrene (1-3).
Conclusions
Intrathoracic perforation of stomach is a rare and potentially fatal complication of acid ingestion. Familiarity with it is essential for both radiologists and surgeons for early diagnosis and management of these high risk cases.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Lupa M, Magne J, Guarisco JL, Amedee R. Update on the diagnosis and treatment of caustic ingestion. Ochsner J 2009;9:54-9. [PubMed]
- Kanne JP, Gunn M, Blackmore CC. Delayed gastric perforation resulting from hydrochloric acid ingestion. AJR Am J Roentgenol 2005;185:682-3. [Crossref] [PubMed]
- Muñoz Muñoz E, García-Domingo MI, Rodríguez Santiago J, Veloso Veloso E, Marco Molina C. Massive necrosis of the gastrointestinal tract after ingestion of hydrochloric acid. Eur J Surg 2001;167:195-8. [Crossref] [PubMed]
- Johansson B, Glise H, Hallerbäck B. Thoracic herniation and intrathoracic gastric perforation after laparoscopic fundoplication. Surg Endosc 1995;9:917-8. [PubMed]
- Sharma S, Gopal SC. Gastric volvulus with perforation in association with congenital diaphragmatic hernia. Indian J Pediatr 2004;71:948. [PubMed]



