A comparative analysis of ECG-gated steady state free precession magnetic resonance imaging versus transthoracic echocardiography for evaluation of aortic root dimensions
Introduction
The aortic root forms a bridge between the left ventricular outflow tract (LVOT) and ascending thoracic aorta and functions as a support structure for the aortic valve. Its walls are formed by three focal expansions called the sinuses of Valsalva which are hollow spaces bounded medially by the aortic valve cusps (1). Aortic root dilatation can be idiopathic or occur in association with a number of pathological conditions including collagen vascular disorders (e.g., Marfan syndrome), connective tissue diseases and bicuspid aortic valve (2). Accurate and reproducible measurement of aortic root dimensions is essential to inform clinical decision making regarding the need for long term imaging surveillance or referral for aortic root and/or valve replacement surgery (3).
Transthoracic echocardiography (TTE) has for many years formed the cornerstone of aortic root assessment but TTE has a number of well recognized limitations. In particular TTE has a limited field of view and potential for restricted acoustic windows (especially in patients who are obese or have emphysema) which can create difficulty getting a precise line of measurement across the widest diameter of the aortic root. Cardiac magnetic resonance imaging (MRI) is increasingly used to evaluate the aortic root and related structures and has a number of advantages over TTE. In particular MRI has an unrestricted field of view and is omniplanar allowing any desired imaging plane to be selected. MRI is considered the “gold standard” technique for assessment of cardiac morphology including the aortic root and recently detailed normal MRI reference ranges for aortic root dimensions have been published (4). In many institutions TTE remains the first line test for cardiac morphological assessment and acts as a gatekeeper for MRI whereby the finding of a dilated aortic root would lead to an MRI aortic study whereas a normal TTE aortic root dimension would not require any further imaging work-up. This strategy is completely dependent upon the accuracy of the TTE measurement to avoid both unnecessary expensive MRI studies and to avoid “missing” patients with a dilated aorta who would benefit from MRI and require long term imaging surveillance. Therefore the purpose of this study was to retrospectively compare aortic root measurements obtained from TTE with those derived from cardiac MRI.
Methods
Study population
A retrospective search of our institutions computerised radiology information system identified all patients that attended for a cardiac MRI study between January 2011 and January 2012 (n=290). The case files of these patients were then reviewed to identify which patients had also undergone a TTE within 4-month of the cardiac MRI study (n=71) which formed the study cohort. The MRI examinations and TTE reports of all these patients were retrospectively reviewed.
The study received institutional review board approval. Informed consent was not required as this is a retrospective observational study and all investigations were carried out as part of routine clinical practice.
MRI protocol
All MRI examinations were performed on a 1.5-T clinical MRI system (Ingenia; Philips Healthcare, Best, The Netherlands) using a 5-channel torso phased array coil. All data were acquired during breath-hold in held end expiration.
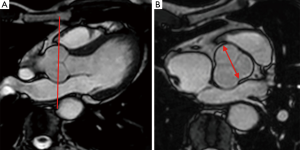
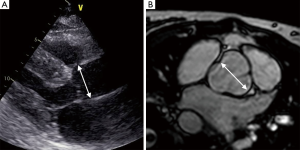
Standardized assessment of the aortic root was performed using a cine bright blood prepared steady state free precession (SSFP) sequence (TR/TE 4/2; flip angle 55°, 8 mm slice thickness, 2 mm interslice gap, matrix size 256×256) acquired in an “optimized” LVOT view (analogous to the parasternal long axis TTE view). This was achieved by selecting a plane through the long axis of the aortic root (planned from a basal short axis slice at the level of the mitral annulus) which was then angulated to transect the left ventricular apex, mid aortic valve and mid-mitral valve. This was followed by a contiguous high-resolution (voxel size 1.7 mm × 1.7 mm × 5 mm, field of view 340 mm × 340 mm, matrix size 320×320) cine-SSFP sequence perpendicular to the aortic root and through the true cross sectional plane of the aortic valve (5) (Figure 1).
Transthoracic echocardiogram (TTE)
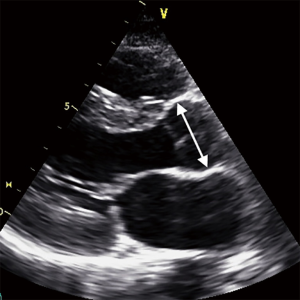
All TTE examinations were performed using a Philips iE33 system (Philips Healthcare, Best, The Netherlands). Using a parasternal long axis window a line of insonation through the mid-portion of the Valsalva sinuses was selected passing through the anterior wall of the right coronary cusp and the posterior wall at the level of the commissure (Figure 2) as per consensus guidelines (6).
Cardiac MRI data analysis
All cardiac MRI datasets were evaluated offline on a dedicated MRI workstation (View Forum; Philips Healthcare, Best, The Netherlands) in consensus by two radiologists with 9 and 8 years experience with cardiovascular MRI who were blinded to the patient’s clinical information.
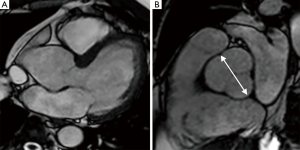
The aortic root dimension was taken through the mid-portion of the Valsalva sinuses from the high resolution cross sectional through plane SSFP images in end-diastole. The maximal cusp-commissure dimension measured from inside wall to inside wall in end-diastole was recorded. These dimensions were then cross-referenced according to patient age with normative MRI aortic root data to categorise the aortic root as either “normal” or “dilated” (if dimension exceeded normative mean + 2SD) (4).
Statistical analysis
Continuous variables are expressed as mean (range), and categorical variables are expressed as percentages. Pearson correlation coefficients and a paired t-test have been used for statistical analysis. All data are expressed as mean ± SD. P values less than 0.05 were considered to indicate statistically significant differences.
Results
Study population
A total of 71 patients had both cardiac MRI and TTE imaging performed within 4-month (mean interval 62 days, range, 5-122 days). Following review of the cardiac MRI datasets three patients were excluded as the MRI studies were not analyzable (incomplete examination due to claustrophobia n=2, heavily degraded image quality precluding proper measurement n=1). The final study population consisted of 68 patients (40 males; 28 females; average age 60; range, 22-86 years).
Aortic root dimensions in all patients
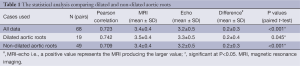
For all 68 patients the mean aortic root dimension measured by TTE was 3.2±0.5 cm and with MRI it was 3.4±0.4 cm (Table 1). The Pearson correlation coefficient was >0.7 indicating a good correlation between the two measurements.
Full table
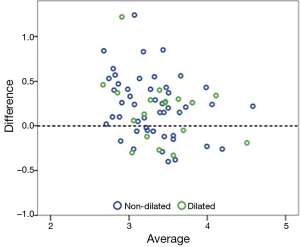
A paired t-test showed the mean difference between TTE and MRI was 0.2±0.3 (P<0.001) which indicates a significant difference (P<0.05) between the two modalities with MRI producing an aortic root dimension consistently higher than TTE by 0.2 cm. This point is also demonstrated on the Bland-Altman plot where the points above the dotted line are where MRI produces a larger measurement (Figure 3).
The patient population was sub-divided into those with aortic root dilatation (n=19) and those with a non-dilated aortic root (n=49) based on the MRI data referenced to the normative ranges.
In four patients with a dilated aortic root by MRI the TTE measurement was considered within the normal reference range (MRI measurement 4.2±0.4 cm vs. TTE measurement 4.0±0.3 cm) (Figure 4).
Patients with a dilated aortic root
In those with a dilated aortic root the mean difference between the MRI and TTE measurements was 0.2±0.4 cm (P=0.045) which was statistically significant (P<0.05) using a paired t-test. MRI consistently measured the aortic root dimension larger compared with TTE (Figure 5).
Patients with a non-dilated aortic root
In those with a non-dilated aortic root the mean difference between the MRI and TTE measurements was 0.2±0.3 cm (P<0.01), which was statistically significant (P<0.05) using a paired t-test. MRI consistently measured the aortic root dimension larger compared with TTE.
Discussion
The present study has shown that TTE consistently underestimates aortic root dimension using MRI as the “gold standard” reference. Although the degree of underestimation is small (0.2±0.3) there is potential for under diagnosis of mild aortic root dilatation with TTE. We used a standard ECG-gated SSFP MRI pulse sequence which is the most commonly used “bright blood” prepared cine imaging technique and upon which the normative data ranges are based (4). The SSFP sequence uses a very short time to repeat (TR) and segmented k-space filling which gives high intrinsic contrast between the blood pool and aortic wall even when local blood velocities are low, without the requirement for administration of exogenous contrast agent (7).
The present study used the Valsalva sinus level as this is typically the region of greatest aortic root diameter and the measurement most often used for clinical decision making (3). In particular the cusp-commissure Valslava sinus dimension used in our study has been shown as the most reproducible measure on MRI and the measure most closely mirroring the American Society of Echocardiography guidelines for TTE measurement which specify a line of insonation passing through the anterior wall of the right coronary cusp and the posterior wall at the level of the commissure on the parasternal long axis view (6). In practice parasternal TTE acoustic windows can be limited and the exact line of insonation may not be achievable in all patients. Also in some patients the Valsalva sinuses are slightly asymmetrical which can also affect the TTE measurement with potential for underestimation when using the right coronary cusp to posterior commissure measurement (4). This in particular may explain the consistent underestimation of aortic root diameter with TTE compared with MRI. Under estimation of aortic root size by TTE may result in a mildly dilated aortic root being labeled as “normal” which is important as such patients may be lost to clinical follow-up, experience progressive root dilatation and not be afforded timely medial and/or surgical interventions (2-4).
Accurate and reproducible measurement of the aortic root has important clinical implications. Aortic root enlargement is the most common definable cause of aortic regurgitation (causing stretching of the aortic annulus and poor cusp coaptation) and root dilatation is also a risk factor for development of aortic dissection and aortic rupture (8).
A large study by Palmieri et al. involving 2,457 patients showed a strong association between the degree of aortic root dilatation and the severity of aortic regurgitation (9). Roman et al. showed aortic root dilatation as the sole cause of aortic regurgitation in up to 30% of patients and a more frequent cause of aortic regurgitation than primary valvular pathology alone (8). Accurate determination of aortic root dimensions is also important for pre-operative planning in those patients undergoing surgery for aortic regurgitation as this will guide the surgical repair technique. If the patient has a dilated ascending aorta but a normal root, a supracoronary graft repair can be performed, whereas a dilated ascending aorta and dilated root require the use of an aortic tube graft with or without valve replacement (2). MRI has particular advantage over TTE for this purpose due to its wide volume coverage and ability to accurately assess the entire ascending thoracic aorta which is usually not possible with TTE scan planes.
The present study is the first to specifically compare MRI with TTE derived measurements. Multi-detector computed tomography (MDCT) angiography derived aortic root measurements have previously been compared with TTE by Ocak et al. These authors showed that TTE measurements were substantially lower or even normal in patients found to have dilated aortic roots by MDCT angiography (10). They also showed a greater variability of TTE measurement compared with MDCT in patients with a dilated aortic root (10).
Limitations
A limitation of our study is the lack of surgical validation for the TTE and MRI measurements; however none of the patients in the cohort were scheduled to undergo aortic surgery during the study period. Concerning the use of MRI as the “gold standard” reference for aortic root measurement this is presumptive and based on consensus guidelines and published literature; comparison of TTE with both MRI and surgical measurements would be required to prove that MRI is the more accurate technique. Finally the TTE and MRI measurements were recorded on different days with potential for some interval change; however the longest interval was 122 days and this is unlikely to have significantly affected our results.
Conclusions
In conclusion this retrospective study has shown a high level of correlation between TTE and MRI derived aortic root measurements at the Valsalva sinus level. It has shown that MRI consistently measures the aortic root dimension higher than TTE which suggests that TTE may under diagnose patients with a mildly dilated aortic root and MRI should be considered as an arbitrator in equivocal cases. Further investigation is required to properly integrate MRI into imaging assessment algorithms in patients with suspected aortic root disease.
Disclosure: The authors declare no conflict of interest.
References
- Ho SY. Structure and anatomy of the aortic root. Eur J Echocardiogr 2009;10:i3-10. [PubMed]
- Hoey ET, Ganeshan A, Nadar SK, Gulati GS. Evaluation of the aortic root with MRI and MDCT angiography: spectrum of disease findings. AJR Am J Roentgenol 2012;199:W175-86. [PubMed]
- Cozijnsen L, Braam RL, Waalewijn RA, Schepens MA, Loeys BL, van Oosterhout MF, Barge-Schaapveld DQ, Mulder BJ. What is new in dilatation of the ascending aorta? Review of current literature and practical advice for the cardiologist. Circulation 2011;123:924-8. [PubMed]
- Burman ED, Keegan J, Kilner PJ. Aortic root measurement by cardiovascular magnetic resonance: specification of planes and lines of measurement and corresponding normal values. Circ Cardiovasc Imaging 2008;1:104-13. [PubMed]
- Kramer CM, Barkhausen J, Flamm SD, Kim RJ, Nagel E; Society for Cardiovascular Magnetic Resonance Board of Trustees Task Force on Standardized Protocols. Standardized cardiovascular magnetic resonance imaging (CMR) protocols, society for cardiovascular magnetic resonance: board of trustees task force on standardized protocols. J Cardiovasc Magn Reson 2008;10:35. [PubMed]
- Bonow RO, Carabello BA, Chatterjee K, de Leon AC Jr, Faxon DP, Freed MD, Gaasch WH, Lytle BW, Nishimura RA, O'Gara PT, O'Rourke RA, Otto CM, Shah PM, Shanewise JS. 2006 Writing Committee Members; American College of Cardiology/American Heart Association Task Force. 2008 Focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation 2008;118:e523-661. [PubMed]
- Krombach GA, Kühl H, Bücker A, Mahnken AH, Spüntrup E, Lipke C, Schröder J, Günther RW. Cine MR imaging of heart valve dysfunction with segmented true fast imaging with steady state free precession. J Magn Reson Imaging 2004;19:59-67. [PubMed]
- Roman MJ, Devereux RB, Niles NW, Hochreiter C, Kligfield P, Sato N, Spitzer MC, Borer JS. Aortic root dilatation as a cause of isolated, severe aortic regurgitation. Prevalence, clinical and echocardiographic patterns, and relation to left ventricular hypertrophy and function. Ann Intern Med 1987;106:800-7. [PubMed]
- Palmieri V, Bella JN, Arnett DK, Roman MJ, Oberman A, Kitzman DW, Hopkins PN, Paranicas M, Rao DC, Devereux RB. Aortic root dilatation at sinuses of valsalva and aortic regurgitation in hypertensive and normotensive subjects: The Hypertension Genetic Epidemiology Network Study. Hypertension 2001;37:1229-35. [PubMed]
- Ocak I, Lacomis JM, Deible CR, Pealer K, Parag Y, Knollmann F. The aortic root: comparison of measurements from ECG-gated CT angiography with transthoracic echocardiography. J Thorac Imaging 2009;24:223-6. [PubMed]


