Cerebral CT angiography and CT perfusion in acute stroke detection: a systematic review of diagnostic value
Introduction
Early detection of acute stroke helps to reduce mortality rate since rapid treatment decision can be made by clinicians (1). Computed tomography angiography (CTA) and CT perfusion (CTP) of the brain are two imaging procedures which are reported to be of paramount importance in the evaluation of acute stroke apart from unenhanced CT for emergency situation (2-7). With the introduction of intravenous contrast material, the exact site of occlusion in the cerebral vessels can be determined clearly through the vascular assessment of CTA (5,8,9). Reconstructed CTA images are available in various formats for visualization of anatomical details such as maximum intensity projection (MIP), shaded surface display (SSD), multi-planar reformation (MRP) and volume rendering technique (VRT) (5,10-12). Moreover, reconstructed images of CTA provide sufficient diagnostic information which enables the CTA to replace MRI, and this could be an advantage for patients unfit for the MRI examination (9).
Studies have reported that the grade of stenosis at a vessel lumen over 50% was likely to cause mild stroke (13-15). In addition, it is also confirmed that at least 30% of patients with more than 70% occluded vessel lumens were detected with stroke (15). Several studies had reported that the multimodal CT evaluation of cerebral vasculature such as a combination of unenhanced CT with CTP and CTA will increase the diagnostic accuracy in the detection of infarction, ischemia and the origin of occluded vessels’ lumen in stroke patients (5,6,16). Kloska et al. stated that the multimodal CT provides sensitivity of 78.9% which is much higher than that of single CT approach with unenhanced CT (55.3%), CTA (57.9%) and CTP (76.3%) (16). Although multimodal CT techniques offer better evaluation of ischemia, infarction and site of occlusion, the radiation dose received by the patient during the procedure is a major concern.
Since the diagnostic value of CTA and CTP in the detection of acute stroke has not been systematically studied, therefore, the purpose of this review was to analyse the diagnostic performance of CTA and CTP in terms of sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and accuracy based on a systematic review of the current literature.
Materials and methods
Seven databases were searched to identify studies of CTA and CTP which were used in the diagnosis of stroke over a period of 20 years (from 1993 to 2013). The search was completely done only on English literature which was included in Highwire, PubMed, Science Direct, Ovid, SpringerLink, Mdconsult and Oxfords journals. The keywords used for identification of references were ‘CTA stroke accuracy’, ‘cerebral CTA in detecting acute stroke’, ‘CTP stroke and accuracy’, ‘CTA brain scan and accuracy’, ‘CTP brain scan and accuracy’ and ‘cerebral CTP in detecting acute stroke’. The search was limited to human subjects, severity of stenosis more than 50% and the value of sensitivity, specificity, PPV, NPV and accuracy must also be reported. Studies conducted on phantom or animals, reported in foreign languages, case reports and review articles were excluded from this study.
Data extraction and analysis
The data were recorded and extracted independently by two authors based on the selection criteria. Information included (I) year of publication; (II) patient demographics such as number of patients and age; (III) types of scanners and (IV) technical parameters such as scan duration and scan delay time were extracted. The other parameters such as sensitivity, specificity, PPV, NPV and accuracy were also extracted in order to analyse the diagnostic value of cerebral CTA and CTP.
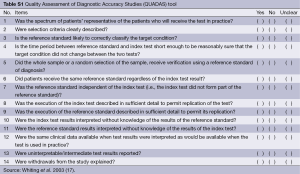
Relevant results were further assessed with Quality Assessment of Diagnostic Accuracy Studies (QUADAS) tool which is a validated consensus method containing 14 checklists for study characteristics investigation of the diagnostic accuracy of the selected chosen studies (Table S1) (17). QUADAS is a screening tool used in the assessment of systematic reviews to avoid the potential for bias, lack of applicability in order to sustain the quality literature report (17).
Full table
Statistical analysis
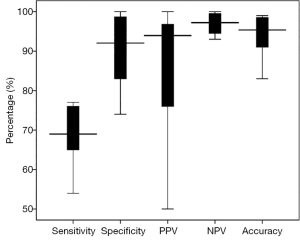
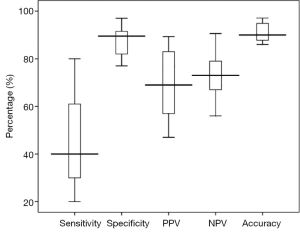
Data were analysed using the Statistical Package for Social Sciences for window version 19.0 (SPSS Inc, Chicago, IL, USA). The diagnostic values in each study was extracted and analysed using multivariate analysis for multifactorial mean comparisons in CTA and CTP. A P value of <0.05 was considered statistically significant difference. Box plots were performed for sensitivity, specificity, PPV, NPV and accuracy for both CTA and CTP techniques.
Assessment of image quality in each study was extracted and analysed with analysis of variance (ANOVA) for multifactorial mean comparisons
Results
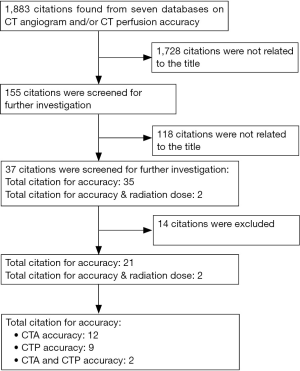
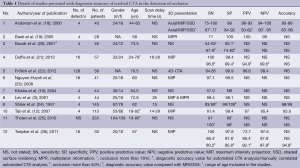
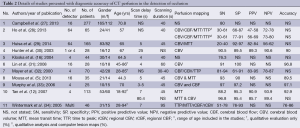
A total of 1,883 citations were identified from all seven databases, of which 21 articles met the inclusion criteria and were included in this analysis. The flow chart of the searched citations is shown in Figure 1. Moreover, the data from selected articles were extracted and tabulated in Table 1 and Table 2 corresponding to CTA and CTP of brain, respectively. As a result, both authors (AS and CS) agreed on a total of 988 patients with mean age of 62.8 years old (range from 19-92 years old) were included in 12 CTA studies (12,16,18-26,35). On the other hand, 896 patients with mean age of 62.8 years old (ranging from 18-94 years old) were included in 11 CTP studies (5,12,16,27-34). The mean scan duration during both procedures were 49 seconds and ranged from 30 to 60 seconds and 35 to 95 seconds corresponding to CTP and CTA, respectively. Disagreements on the final results were resolved by consensus.
Full table
Full table
Analysis of diagnostic performance of CTA and CTP
In the analysis of 12 CTA studies, the mean sensitivity, specificity, PPV, NPV and accuracy were 83.2% (95% CI: 57.9-100%), 95.0% (95% CI: 74.4-100%), 84.1% (95% CI: 50.0-100%), 97.1% (95% CI: 94.0-100%) and 94.0% (95% CI: 83.0-99.0%), respectively, while in the CTP studies, the corresponding values were 69.9% (95% CI: 20.0-97.0%), 87.4% (95% CI: 61.0-100%), 76.4% (95% CI: 48.0-95.4%), 78.2% (95% CI: 55.8-93.9%) and 89.8% (95% CI: 75.7-97.1%), respectively. The detailed comparison for both CTA and CTP diagnostic quality criteria were presented in the boxplot (Figures 2 and 3).
Of CTA studies, the diagnostic performance was divided into two groups consisting of the degree of stenosis more than 70% and stenosis of between 50% and 70%. Among 12 CTA studies, only four studies showed high diagnostic value for stenosis of more than 70% (18,23,32,35) which resulted in the sensitivity, specificity, PPV and NPV of 73.6% (95% CI: 54.2-91.0%), 91.8% (95% CI: 84.0-99.0%), 62.1% (95% CI: 50-86.4%) and 95.2% (95% CI: 93.0-97.6%), respectively.
In the remaining eight studies, it was reported that the diagnostic value of stenosis between 50% and 70% was as follows: mean sensitivity, specificity, PPV and NPV were 89.7% (95% CI: 66.7-100%), 91.5% (95% CI: 74.4-99.5%), 98.7% (95% CI: 97.9-99.6%) and 98.8% (95% CI: 97.9-99.6%), respectively. However, the occlusion which was reported with less than 50%, were not analysed due to the small number of cases.
In the CTP studies, the diagnostic value of sensitivity, specificity, PPV and PPV was calculated based on patients with symptoms suggestive of acute ischemic stroke, transient ischemic attack (TIA) and non-stroke mimics. Therefore, cerebral blood volume (CBV) and cerebral blood flow (CBF) of colour map signals, other than mean transit time (MTT) or time to peak (TTP) of perfusion study were performed to obtain the diagnostic accuracy of the study which leads to the early detection of ischemic and infarct tissue of the brain. Only 9 out of 11 studies reported the CBV which was used to measure the stroke with the sensitivity, specificity, PPV and NPV values being 75.4% (95% CI: 45.5-96.8%); 89.4% (95% CI: 76-100%); 78.9% (95% CI: 52.5-90.9%) and 80.9% (95% CI: 74.5-93.9%), respectively (5,12,28-34).
Based on the multivariate analysis, the results showed that the differences in diagnostic values were variable depending on CTA and CTP. The accuracy and PPV were not found statistically significant between CTA and CTP with P value of 0.227 and 0.276, respectively. The remaining diagnostic values between CTA and CTP were not significantly different.
Quality assessment
QUADAS assessment was performed in both CTA and CTP studies. A 100% score was achieved for questions 1, 13 and 14 in CTA studies, followed by 92.9% score being achieved for questions 2 and 8, 85.7% score was received for questions 3, 4, 5, 7, 10, 11 and 12 (Appendix I). However, questions 6 and 9 were only scored with 78.6%. Moreover, results of the CTP studies were found to have 100% in 10 questions and in the remaining 4 questions they were only scored at 90.9%.
Discussion
This systematic review provides a comparative analysis of the mean sensitivity, specificity, PPV, NPV and accuracy between CTA and CTP procedures in the detection of stroke. Firstly, the analysis shows that overall diagnostic performance of CTA was higher than that in CTP. Secondly, both CTA and CTP procedures are likely to be more specific rather than sensitive in the detection of stroke especially with the stenosis more than 70%. Moreover, CTA procedure provides high diagnostic accuracy for detection of the site of occlusion and determines its severity while CTP procedure offers high diagnostic accuracy to detect ischemic lesion of brain tissue and distinguish between infarcted and ischemic penumbra. In fact, the ability to precisely evaluate the sub-group of ischemia and infarction definitely helps to suggest the decision making in performing thrombolytic therapy (4).
According to the analysis of CTA studies, the type of CT scanner is not only important in providing diagnostic quality of the scan, but also plays an important role in providing the diagnosis of stroke in terms of sensitivity, specificity, NPV, PPV and accuracy. Since most of the studies analysed in this review included the CTA examinations which were performed with older generation of CT scanners, our analysis also showed that the diagnostic accuracy of CTA in the highly severe stenosis (>70%) was significantly lower than that in the lower degree of stenosis (<50%) (20,25,26). This is supported by Bucek et al.’s study (20) which used 4-slice CT and was reported to have the lowest sensitivity value in the detection of stroke compared to another study with 16-slice CT which resulted in 86.4% of sensitivity in the detection of stenosis of more than 70% (20,26). Although 4-slice CT was found to contribute to lower sensitivity compared to the latest generation of CT scanners, the sensitivity value can be improved from 54.2% to 62.5% if the automated CTA analysis was manually corrected (20). Thus, it could be explained that the available updated software could potentially improve the diagnostic accuracy in the detection of stenosis.
Measurement tools in CTA which are used to measure the vessels lumen in the stroke assessment also contribute to the effectiveness of the procedure. This was supported by Nguyen-Huynh et al. (23) with the sensitivity and specificity being reported to be at 97.1% and 99.5% in detecting occlusion of more than 50%. Moreover, the digital callipers were used in the measurement of stenosis in their study which leads to improving the value of sensitivity and specificity (23).
In this review, the mean sensitivity for CTP in the detection of ischemia and infarct was reported to be as low as 67.0% (95% CI: 20.0-97.0%). This is due to the fact that two out of 11 studies reported the lowest sensitivity value in CBV mapping with 20% (29) and 30% (28) respectively. This low score was reflected by the small ischemic volume proportion included in these studies. On the other hand, several studies reported high value of sensitivity in CTP stroke detection ranging from 89% to 93% (31,32,34). The results were based on studies using MTT in perfusion mapping to diagnose acute stroke. Moreover, diffusion-weighted imaging (DWI) was performed to confirm the diagnosis in patients with large hemispheric stroke. MTT in perfusion mapping provides accurate prediction of ischemic core compared to CBV and CBF (12,28,29,34). However, the combined perfusion mapping techniques definitely provide greater sensitivity as reported in the previous studies (89-97%) (5,12,27-34).
Other studies reported that CTP technique was able to demonstrate the site of occlusion using MTT perfusion mapping with high value of sensitivity, specificity, PPV, NPV and accuracy at 88.2%, 95.3%, 90.9%, 93.9% and 92.9%, respectively (12,28,29). Moreover, a combination of perfusion mapping techniques such as MTT, CBV and CBF would be able to give conclusive information of severity of the ischemic lesion which also helps in the management of strokes (28,29,32,34,36).
Nevertheless, the major concern in the evaluation of acute stroke using either CTA or CTP technique is the ionizing radiation exposed to the patient. Several techniques have been developed with the recent multi slice CT technology in order to reduce radiation dose inclusive of short time of acquisition (7,24), early arterial phase mode which reduces the interruption of venous contamination during MIP, complete evaluation of intracranial arteries (5,12) and able to widen the coverage of the entire brain with single acquisition during CTP (5,29). Thus, optimisation of CTA or CTP protocols is necessary to minimise radiation exposure to patients without compromising diagnostic images which is parallel to the ‘as low as reasonably achievable (ALARA)’ principle. The diagnostic accuracy of acute stroke evaluation can be increased with implementation of both CTA and CTP procedures. In this case, the application of dose reduction techniques is of paramount importance to minimize the radiation dose.
Some limitations exist in this review. A small number of studies are included in the analysis. This is due to the fact that most of the articles reviewed did not provide the quantitative diagnostic accuracy for CTA and CTP distinctively. Furthermore, some studies provided information about mixed values of quantitative diagnostic accuracy in their reports with a combination of several protocols such as CTP with DWI, CTP with MR perfusion and other protocols. Therefore, we have to exclude it from our analysis. Finally, radiation dose was not analysed and compared in this analysis as the dose information was only provided in one study.
In conclusion, this systematic review shows that CTA provides high diagnostic value in the detection of occlusion in high degree of stenosis whereas CTP provides high specificity in the detection of ischemia and infarct tissue of brain. However, the most accurate assessment for acute stroke involving the site of occlusion, infarction core and salvageable brain tissue is a combination of different CT procedures involving CTA and CTP.
Acknowledgements
We would like to thank Associate Professor Dr. Jemaima Che Hamzah, Professor Dr. Suzana Shahar and Professor Dr. Bariah Mohd Ali for their contribution to the proof-read of the article.
Author contributions: Sabarudin, A. designed the overall study with contributions from Subramaniam, C. The data were collected by Subramaniam, C. and the data were processed and analyzed by Sabarudin, A. and Subramaniam, C. This manuscript was written by Sabarudin, A. and Subramaniam, C while Sun, Z. discussed and edited the manuscript.
Disclosure: The authors declare no conflict of interest.
References
- Grotta JC, Chiu D, Lu M, Patel S, Levine SR, Tilley BC, Brott TG, Haley EC Jr, Lyden PD, Kothari R, Frankel M, Lewandowski CA, Libman R, Kwiatkowski T, Broderick JP, Marler JR, Corrigan J, Huff S, Mitsias P, Talati S, Tanne D. Agreement and variability in the interpretation of early CT changes in stroke patients qualifying for intravenous rtPA therapy. Stroke 1999;30:1528-33. [PubMed]
- Aviv RI, Shelef I, Malam S, Chakraborty S, Sahlas DJ, Tomlinson G, Symons S, Fox AJ. Early stroke detection and extent: impact of experience and the role of computed tomography angiography source images. Clin Radiol 2007;62:447-52. [PubMed]
- Lev MH, Farkas J, Rodriguez VR, Schwamm LH, Hunter GJ, Putman CM, Rordorf GA, Buonanno FS, Budzik R, Koroshetz WJ, Gonzalez RG. CT angiography in the rapid triage of patients with hyperacute stroke to intraarterial thrombolysis: accuracy in the detection of large vessel thrombus. J Comput Assist Tomogr 2001;25:520-8. [PubMed]
- Schramm P. CT angiography and perfusion CT in acute stroke: principles and applications. Imaging Decisions MRI 2003;7:31-41.
- Mousa AE, Elrakhawy MM, Zaher AA. Multimodal CT assessment of acute ischemic stroke. Egypt J Radiol Nuc Med 2013;44:71-81. Available online: http://www.sciencedirect.com/science/article/pii/S0378603X12001234
- Scharf J, Brockmann MA, Daffertshofer M, Diepers M, Neumaier-Probst E, Weiss C, Paschke T, Groden C. Improvement of sensitivity and interrater reliability to detect acute stroke by dynamic perfusion computed tomography and computed tomography angiography. J Comput Assist Tomogr 2006;30:105-10. [PubMed]
- Cohnen M, Wittsack HJ, Assadi S, Muskalla K, Ringelstein A, Poll LW, Saleh A, Mödder U. Radiation exposure of patients in comprehensive computed tomography of the head in acute stroke. AJNR Am J Neuroradiol 2006;27:1741-5. [PubMed]
- Rai AT, Raghuram K, Carpenter JS, Domico J, Hobbs G: Pre-intervention cerebral blood volume predicts outcomes in patients undergoing endovascular therapy for acute ischemic stroke. J Neurointerv Surg 2013;5 Suppl 1:i25-32. [PubMed]
- Katz DA, Marks MP, Napel SA, Bracci PM, Roberts SL. Circle of Willis: evaluation with spiral CT angiography, MR angiography, and conventional angiography. Radiology 1995;195:445-9. [PubMed]
- Leclerc X, Godefroy O, Lucas C, Benhaim JF, Michel TS, Leys D, Pruvo JP. Internal carotid arterial stenosis: CT angiography with volume rendering. Radiology 1999;210:673-82. [PubMed]
- Puchner S, Popovic M, Wolf F, Reiter M, Lammer J, Bucek RA. Multidetector CTA in the quantification of internal carotid artery stenosis: value of different reformation techniques and axial source images compared with selective carotid arteriography. J Endovasc Ther 2009;16:336-42. [PubMed]
- Tan JC, Dillon WP, Liu S, Adler F, Smith WS, Wintermark M. Systematic comparison of perfusion-CT and CT-angiography in acute stroke patients. Ann Neurol 2007;61:533-43. [PubMed]
- Marquardt L, Kuker W, Chandratheva A, Geraghty O, Rothwell PM. Incidence and prognosis of > or = 50% symptomatic vertebral or basilar artery stenosis: prospective population-based study. Brain 2009;132:982-8. [PubMed]
- Buskens E, Nederkoorn PJ, Buijs-Van Der Woude T, Mali WP, Kappelle LJ, Eikelboom BC, Van Der Graaf Y, Hunink MG. Imaging of carotid arteries in symptomatic patients: cost-effectiveness of diagnostic strategies. Radiology 2004;233:101-12. [PubMed]
- North American Symptomatic Carotid Endarterectomy Trial Collaborators. Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. N Engl J Med 1991;325:445-53. [PubMed]
- Kloska SP, Nabavi DG, Gaus C, Nam EM, Klotz E, Ringelstein EB, Heindel W. Acute stroke assessment with CT: do we need multimodal evaluation? Radiology 2004;233:79-86. [PubMed]
- Whiting P, Rutjes AW, Reitsma JB, Bossuyt PM, Kleijnen J. The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med Res Methodol 2003;3:25. [PubMed]
- Anderson GB, Ashforth R, Steinke DE, Ferdinandy R, Findlay JM. CT angiography for the detection and characterization of carotid artery bifurcation disease. Stroke 2000;31:2168-74. [PubMed]
- Bash S, Villablanca JP, Jahan R, Duckwiler G, Tillis M, Kidwell C, Saver J, Sayre J. Intracranial vascular stenosis and occlusive disease: evaluation with CT angiography, MR angiography, and digital subtraction angiography. AJNR Am J Neuroradiol 2005;26:1012-21. [PubMed]
- Bucek RA, Puchner S, Kanitsar A, Rand T, Lammer J. Automated CTA quantification of internal carotid artery stenosis: a pilot trial. J Endovasc Ther 2007;14:70-6. [PubMed]
- Duffis EJ, Jethwa P, Gupta G, Bonello K, Gandhi CD, Prestigiacomo CJ. Accuracy of computed tomographic angiography compared to digital subtraction angiography in the diagnosis of intracranial stenosis and its impact on clinical decision-making. J Stroke Cerebrovasc Dis 2013;22:1013-7. [PubMed]
- Frölich AM, Psychogios MN, Klotz E, Schramm R, Knauth M, Schramm P. Angiographic reconstructions from whole-brain perfusion CT for the detection of large vessel occlusion in acute stroke. Stroke 2012;43:97-102. [PubMed]
- Nguyen-Huynh MN, Wintermark M, English J, Lam J, Vittinghoff E, Smith WS, Johnston SC. How accurate is CT angiography in evaluating intracranial atherosclerotic disease? Stroke 2008;39:1184-8. [PubMed]
- Shrier DA, Tanaka H, Numaguchi Y, Konno S, Patel U, Shibata D. CT angiography in the evaluation of acute stroke. AJNR Am J Neuroradiol 1997;18:1011-20. [PubMed]
- Tholen AT, de Monyé C, Genders TS, Buskens E, Dippel DW, van der Lugt A, Hunink MG. Suspected carotid artery stenosis: cost-effectiveness of CT angiography in work-up of patients with recent TIA or minor ischemic stroke. Radiology 2010;256:585-97. [PubMed]
- Toepker M, Mahabadi AA, Heinzle G, Hofmann W, Mathies R, Schuster A, Cejna M. Accuracy of MDCT in the determination of supraaortic artery stenosis using DSA as the reference standard. Eur J Radiol 2011;80:e351-5. [PubMed]
- Campbell BC, Weir L, Desmond PM, Tu HT, Hand PJ, Yan B, Donnan GA, Parsons MW, Davis SM. CT perfusion improves diagnostic accuracy and confidence in acute ischaemic stroke. J Neurol Neurosurg Psychiatry 2013;84:613-8. [PubMed]
- Ho CY, Hussain S, Alam T, Ahmad I, Wu IC, O’Neill DP. Accuracy of CT cerebral perfusion in predicting infarct in the emergency department: lesion characterization on CT perfusion based on commercially available software. Emerg Radiol 2013;20:203-12. [PubMed]
- Huisa BN, Neil WP, Schrader R, Maya M, Pereira B, Bruce NT, Lyden PD. Clinical use of computed tomographic perfusion for the diagnosis and prediction of lesion growth in acute ischemic stroke. J Stroke Cerebrovasc Dis 2014;23:114-22. [PubMed]
- Hunter GJ, Silvennoinen HM, Hamberg LM, Koroshetz WJ, Buonanno FS, Schwamm LH, Rordorf GA, Gonzalez RG. Whole-brain CT perfusion measurement of perfused cerebral blood volume in acute ischemic stroke: probability curve for regional infarction. Radiology 2003;227:725-30. [PubMed]
- Lin K, Rapalino O, Law M, Babb JS, Siller KA, Pramanik BK. Accuracy of the Alberta Stroke Program Early CT Score during the first 3 hours of middle cerebral artery stroke: comparison of noncontrast CT, CT angiography source images, and CT perfusion. AJNR Am J Neuroradiol 2008;29:931-6. [PubMed]
- Mayer TE, Hamann GF, Baranczyk J, Rosengarten B, Klotz E, Wiesmann M, Missler U, Schulte-Altedorneburg G, Brueckmann HJ. Dynamic CT perfusion imaging of acute stroke. AJNR Am J Neuroradiol 2000;21:1441-9. [PubMed]
- Murphy BD, Fox AJ, Lee DH, Sahlas DJ, Black SE, Hogan MJ, Coutts SB, Demchuk AM, Goyal M, Aviv RI, Symons S, Gulka IB, Beletsky V, Pelz D, Hachinski V, Chan R, Lee TY. Identification of penumbra and infarct in acute ischemic stroke using computed tomography perfusion-derived blood flow and blood volume measurements. Stroke 2006;37:1771-7. [PubMed]
- Wintermark M, Fischbein NJ, Smith WS, Ko NU, Quist M, Dillon WP. Accuracy of dynamic perfusion CT with deconvolution in detecting acute hemispheric stroke. AJNR Am J Neuroradiol 2005;26:104-12. [PubMed]
- Lev MH, Nichols SJ. Computed tomographic angiography and computed tomographic perfusion imaging of hyperacute stroke. Top Magn Reson Imaging 2000;11:273-87. [PubMed]
- Koenig M, Kraus M, Theek C, Klotz E, Gehlen W, Heuser L. Quantitative assessment of the ischemic brain by means of perfusion-related parameters derived from perfusion CT. Stroke 2001;32:431-7. [PubMed]


