Hepatic artery aneurysm causing obstructive jaundice
Case presentation
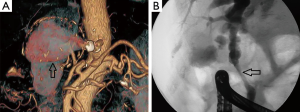
A 76-year-old man with a previous history of ischemic stroke was presented with painless jaundice. Physical examination on admission was unremarkable, his total serum bilirubin was 288 mmol/L with no other significant abnormal laboratory findings. Abdominal ultrasound showed cystic-appearing, hypoechoic mass at the hepatic hilum (Figure 1A) and dilatation of the intrahepatic bile ducts. A subsequent computed tomography (CT) confirmed the presence of a cyst-like lesion at the hepatic hilum, which was filled with contrast in the early arterial phase (Figure 1B,C). A virtual CT-angiography demonstrated 64 mm large hepatic artery aneurysm and circumferential calcification of the common hepatic artery at its origin (Figure 2A). A compression of the common bile duct from the aneurysm was considered as the cause of the jaundice, and was confirmed by endoscopic retrograde cholangiography (Figure 2B). Endoscopic stenting of common bile duct was performed and the jaundice relieved. The patient declined further management of the aneurysm by surgery or interventional radiology and received only ursodeoxycholic acid as a maintenance therapy. At follow-up 12 months later, the patient had no symptoms.

Hepatic artery aneurysms (HAA) are rare and represent 14-20% of all visceral artery aneurysms (1,2). The vast majority of HAA are single and are located extrahepatically (3). Nowadays about half of the HAA are iatrogenic, as a consequence of the widespread use of interventional diagnostic and therapeutic biliary procedures. Abdominal trauma, infection, inflammation and atherosclerosis are other common predisposing factors (1,4). The presence of multiple HAA and non-atherosclerotic origin of the aneurysm were identified as risk factors for rupture (2). Most of the HAA are asymptomatic, and 60-80% of the patients are diagnosed when the aneurysm has complicated (5) with rupture and bleeding (haemobilia/gastrointestinal, intraabdominal or retroperitoneal), or as in our case with painless obstructive jaundice due to external bile duct compression. However jaundice can be also caused by rupture of the HAA into the biliary tree with clots occluding the lumen, which represents clinically with Quinke’s triad (abdominal pain, gastrointestinal bleeding and jaundice). Unusual presentation of HAA as cholangitis and portal hypertension are also reported (6). Irrespective of clinical presentation the diagnosis of HAA is always based on imaging studies.
There are several options to treat HAA with surgery and/or interventional radiology (2,7), and they should be considered individually bearing in mind both general condition of the patient and multiple local factors (location and size of the aneurysm, presence of collateral circulation to the liver, local infection, rupture). There is still no single treatment modality considered as best treatment option for all patients having aneurysm of hepatic artery.
Disclosure: The authors declare no conflict of interest.
References
- Jana M, Gamanagatti S, Mukund A, Paul S, Gupta P, Garg P, Chattopadhyay TK, Sahni P. Endovascular management in abdominal visceral arterial aneurysms: A pictorial essay. World J Radiol 2011;3:182-7. [PubMed]
- Abbas MA, Fowl RJ, Stone WM, Panneton JM, Oldenburg WA, Bower TC, Cherry KJ, Gloviczki P. Hepatic artery aneurysm: factors that predict complications. J Vasc Surg 2003;38:41-5. [PubMed]
- Hulsberg P, Garza-Jordan Jde L, Jordan R, Matusz P, Tubbs RS, Loukas M. Hepatic aneurysm: a review. Am Surg 2011;77:586-91. [PubMed]
- O’Driscoll D, Olliff SP, Olliff JF. Hepatic artery aneurysm. Br J Radiol 1999;72:1018-25. [PubMed]
- Sheldon DM, Crawford M, Mihrshahi S, Gallagher J, Storey D. Therapeutic considerations in obstructive jaundice due to hepatic artery aneurysm. HPB (Oxford) 2006;8:74. [PubMed]
- Noor MT, Dutta U, Appasani S, Kochhar R, Singh K. Hepatic artery aneurysm: a rare presentation as cholangitis and portal hypertension. Gastrointest Endosc 2012;75:190; discussion 190-1. [PubMed]
- Nagaraja R, Govindasamy M, Varma V, Yadav A, Mehta N, Kumaran V, Gupta A, Nundy S. Hepatic artery pseudoaneurysms: a single-center experience. Ann Vasc Surg 2013;27:743-9. [PubMed]


