
“Sixteen syndrome”—a new pontine ophthalmo-neurological syndrome within the one-and-a-half syndrome spectrum of disorders: case report and literature review
Introduction
The one-and-a-half syndrome is a term originally proposed by Fisher to describe a syndrome with ocular dyskinesia, exhibiting ipsilateral conjugate gaze palsy and ipsilateral internuclear ophthalmoplegia (INO) (1). The underlying pathological lesion is frequently at the level of the unilateral tegmentum, affecting the paramedian pontine reticular formation (PPRF), abducens nucleus, and medial longitudinal fasciculus (MLF). The lesion is mainly caused by cerebrovascular disease leading to ponto-cerebral infarction. After the first report of the one-and-a-half syndrome, several numbered ophthalmo-pontine neurological syndromes have been reported with the clinical features of the one-and-a-half syndrome appearing in all subsequent reports. Accordingly, the clinical features of the numbered ophthalmo-pontine syndromes are indicative of the precise locus of the lesion, highlighting the clinical significance. We here report a case of “sixteen syndromes”, which we believe to be the first case of its kind to be reported in the literature.
Case presentation
A 52-year-old male presented with dizziness, diplopia, salivation, and mild weakness in the right limb for 3 days. He had poorly controlled hypertension and diabetes, with a nearly 30-year history of smoking and drinking, suggesting a cerebrovascular etiology. Blood pressure at hospital admission was 162/88 mmHg. Neurological examination revealed a complete inability to adduct the left eye and incomplete mild abduction. The right eye was completely incapable of adduction, and there was diplopia in both the left and right vision. The vertical movement of both eyes was normal. The bilateral frontal lines were shallow, the eyes could not close completely, the mouth angle was drooping, and the patient had the difficulty of blowing his cheeks with hydrostomia salivation. A bilateral peripheral facial nerve (cranial nerve VII) paralysis was suspected based on the observed clinical features. The right upper and lower limbs were mildly weak, and the right side was positive for Babinski reflex.
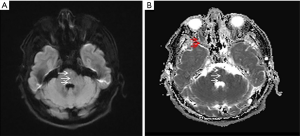
Laboratory tests showed an increase in fasting blood glucose (10.02 mmol/L) and glycated hemoglobin (8.1%). Urine routine glucose (4+), low-density lipoprotein cholesterol (2.49 mmol/L), and homocysteine levels were normal. Magnetic resonance diffusion-weighted imaging (DWI) and apparent diffusion coefficient (ADC) showed bilateral pontine tegmentum and pars basilaris intrusion, as evident from the distinct abnormal signals along the arrow pointing to a continuous linear anomaly signal (Figure 1). Magnetic resonance angiography (MRA) did not show evidence of significant aortic lesions.
After admission, he was given dual antiplatelet, statin, antihypertensive, and antidiabetic therapy. After 2 days, the right limb weakness completely disappeared, but positive Babinski reflex continued. He was discharged after 10 days with significant improvement in dizziness, but improvements in peripheral facial paralysis and diplopia symptoms were not obvious. After 1 month of follow-up, diplopia disappeared, leaving only a slight peripheral facial paralysis on the left side. There was a slight persistence of left side peripheral facial paralysis after 3 and 6 months of follow-up.
Discussion
Pontine vascular lesions are relatively rare in comparison to cerebral hemorrhage. Owing to the close anatomical proximity of the cranial nerve nuclei to the pontine nuclei, pontine vascular lesions affect the cranial nuclei, leading to distinct clinical symptoms (2). The specific symptoms correlate well with the affected cranial nerve, which is most often revealed by radiological imaging (3,4). The first reported pontine vascular lesion causing specific clinical features is the-one-and-a-half syndrome characterized by a horizontal movement disorder of the eyeballs, presenting as ipsilateral conjugate horizontal gaze palsy (one) and ipsilateral internuclear ophthalmoplegia (INO) (a half) (1). Subsequently, a series of pontine vascular lesions with the involvement of additional cranial nerves leading to distinct clinical symptoms were reported and grouped as the one-and-a-half syndrome spectrum of disorders (5). In all the reported cases, horizontal gaze palsy and ipsilateral INO were conserved, and the diagnosis relies on clinical symptoms and imaging technologies (6).
The other numerically named syndromes related to the one-and-a-half syndrome include the eight-and-a-half syndrome (7) (one-and-a-half syndrome + damaged ipsilateral nerve; a lesion located on the ipsilateral PPRF, MLF, or facial nucleus; or an injured ipsilateral abducens nucleus, MLF, facial nucleus, or nerve bundle), nine syndrome (6) (eight-and-a-half + contralateral hemiplegia/sensory disorder/ataxia due to the expansion of the lesion to the surrounding tissue), thirteen and-a-half syndrome (8) [eight-and-a-half syndrome + impaired ipsilateral trigeminal nerve (cranial nerve V)], fifteen-and-a-half syndrome (one-and-a-half syndrome + bilateral facial nerve palsy) (9), sixteen-and-a-half syndrome (eight-and-a-half syndrome + impaired ipsilateral auditory nerve (cranial nerve VIII)) (10), twenty-and-a-half syndrome (fifteen-and-a-half syndrome + ipsilateral trigeminal nerve palsy) (11), and twenty-four-and-a-half syndrome [bilateral facial nerve palsy, bilateral horizontal gaze, and contralateral sensorineural hearing deficit (7+7+1+1+8)] (2) .
Among the numerically named syndromes, the-eight-and-a-half syndrome is the most frequently reported in the literature. The first report of the eight-and-a-half syndrome by Eggenberger et al. was based only on clinical symptoms without radiological confirmation (3). The naming and presumptive identification was later substantiated by Nandhagopal and Krishnamoorthy in a diabetic patient, and the lesion was located in the lower pontine tegmentum affecting the right abducens nucleus, right medial longitudinal fasciculus, and right facial nucleus/fascicle. In most of the reported cases, the reason for the pontine lesion was infarction of the perforating artery, which was identified in all the cases by radiological imaging (4). With respect to the naming convention, the nine syndromes were the first syndrome to provide grading to hemiparesis (half), and the subsequently reported disorders provided half a grading point for hemiparesis. In addition to tegmentum, ventromedial parts of the pons were also affected, leading to additional clinical symptoms (hemiparesis) (12).
The most recent addition to the one-and-a-half syndrome spectrum of disorders is the twenty-and-a-half syndrome (1.5+7+7+5), reported in an Indian patient, affecting both the facial and trigeminal nerves. Radiological imaging revealed infarction in the posterolateral pons and medulla, and a small vessel disease of the brain was suspected. Contrary to most other reports, the patient was not diabetic and did not have any known risk factors for cerebrovascular disease (11).
We described a patient with a horizontal gaze palsy with clinical features suggestive of ipsilateral internuclear ophthalmoplegia (one-and-a-half syndrome). We also observed clinical neurological symptoms indicating bilateral facial nerve palsy (cranial nerve VII + VII) with partial hemiparesis. We named the syndrome sixteen syndrome keeping in line with the other named numerical neuro-ophthalmological syndromes (6,12).
In this case, the axons of internuclear neurons from the abductor nucleus were affected nearly as they passed through the midline in the medial longitudinal bundle (MLF) rising up to the level of the oculomotor subnucleus that controls the medial rectus. Hence, the patient’s bilateral eyeballs had no adduction. Further, the left abductor nerve was slightly damaged, affecting the abduction of the left eye, which was incomplete. This constitutes the one-and-a-half syndrome (1.5). Moreover, the bilateral facial nerve nucleus was damaged (7+7), resulting in bilateral peripheral facial paralysis. The weakness of the right limb (0.5), lasted 5 days with positive Babinski reflex.
The relevant literature indicates that the clinically similar fifteen-and-a-half syndrome may be caused by bilateral dominance of the basilar artery or the long circulatory artery to the distal variability, suggestive of vascular damage. However, there is no previous imaging evidence (9). In our case, the arrows in the DWI and ADC of the patient mark the lesion area, indicating the paramedian artery, which directly proves the vascular origin of the lesion.
In general, it has been observed that patients with the previous fifteen-and-a-half syndrome were associated with hypertension and diabetes, which are symptomatic of vascular disease. Our case was no exception. No obvious stenosis and plaque were observed on MRA, although high-resolution magnetic resonance imaging was not performed. However, from the distribution characteristics of the lesions, it could be a case of small vessel disease. To conclude, this kind of case is extremely rare, and it further expands the landscape of ophthalmo-pontine disorders. Knowledge of the clinical features will help in identifying the lesion locus in the brain and in turn, improve clinical practice and standard of care.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Fisher CM. Some neuro-ophthalmological observations. J Neurol Neurosurg Psychiatry 1967;30:383-92. [Crossref] [PubMed]
- Karadan U, Supreeth RN, Manappallil RG, Jayakrishnan C. Twenty-Four Syndrome: An Untold Presentation of Pontine Hemorrhage. J Stroke Cerebrovasc Dis 2018;27:e73-4. [Crossref] [PubMed]
- Eggenberger E. Eight-and-a-half syndrome: One-and-a-half syndrome plus cranial nerve VII palsy. J Neuroophthalmol 1998;18:114-6. [Crossref] [PubMed]
- Nandhagopal R, Krishnamoorthy SG. Neurological picture. Eight-and-a-half syndrome. J Neurol Neurosurg Psychiatry 2006;77:463. [Crossref] [PubMed]
- Xue F, Zhang L, Zhang L, Ying Z, Sha O, Ding Y. One-and-a-half syndrome with its spectrum disorders. Quant Imaging Med Surg 2017;7:691-7. [Crossref] [PubMed]
- Mahale RR, Mehta A, John AA, Javali M, Abbas MM, Rangasetty S. "Nine" syndrome: A new neuro-ophthalmologic syndrome: Report of two cases. Ann Indian Acad Neurol 2015;18:335-7. [Crossref] [PubMed]
- Almutlaq A, Richard A. Eight-and-a-half syndrome: one-and-a-half syndrome with peripheral facial nerve palsy. CMAJ 2018;190:E510. [Crossref] [PubMed]
- Allbon DS, Hood B, La . Thirteen-and-a-half syndrome. J Neuroophthalmol 2016;36:191-2. [Crossref] [PubMed]
- Li M, Li X, Liu L, Zhu M, Lu D, Wang P. A case report of the rare fifteen-and-a-half syndrome. Medicine (Baltimore) 2019;98:e14553. [Crossref] [PubMed]
- Borgman CJ, Jackson AM. Sixteen-and-a-half syndrome: a variant in the spectrum of Fisher's one-and-a-half syndrome. Clin Exp Optom 2019;102:94-6. [Crossref] [PubMed]
- Dube M, Dani R, Dubey A, Chouksey D. Twenty-and-a-half syndrome: a case report. J Med Case Rep 2019;13:35. [Crossref] [PubMed]
- Rosini F, Pretegiani E, Guideri F, Cerase A, Rufa A. Eight and a half syndrome with hemiparesis and hemihypesthesia: the nine syndrome? J Stroke Cerebrovasc Dis 2013;22:e637-8. [Crossref] [PubMed]


