A modified technique for real time ultrasound guided pediatric percutaneous renal biopsy: the angled tangential approach
Introduction
Percutaneous renal biopsy (PRB) has become one of the fundamental diagnostic techniques in nephrology since its introduction in 1951 (1-4). As for the pediatric population, PRB is a valuable procedure for the diagnosis of renal disease, and is often helpful in guiding medical therapy and establishing prognosis. Biopsy device and guidance methods have been refined progressively during the past two decades with the use of surface anatomic landmarks for guidance superseded by ultrasonography (US).
PRB is a safe and practical procedure that provides important information to the pediatric nephrologist in establishing the diagnosis, evaluating the acuteness and severity of the disease, monitoring disease progression, and assessing the response to therapy (3,4). However, pediatric renal biopsy may result in serious hemorrhagic complications, requiring additional diagnostic procedures, blood transfusion, vascular interventions, and prolongation of hospitalization. When performing a renal biopsy, the principle is to remove the minimum amount of tissue necessary for accurate diagnosis by obtaining the maximum amount of diagnostic tissue per biopsy, while minimizing the risk of major hemorrhagic complications. In the past, PRB was performed blindly after using sonography to mark the lower pole of the kidney on the skin. During the recent years, real-time ultrasound-guided renal biopsy using an automated biopsy gun, has been adopted as the standard of care by many nephrologists (1-4).
In this study, we aimed to propose the angled tangential approach technique for real-time ultrasound-guided pediatric percutaneous renal biopsy. The biopsy method described was assessed for utility in consecutive patients requiring renal biopsy.
Materials and methods
We retrospectively reviewed consecutive pediatric patients who had undergone real time ultrasound guided renal biopsy with angled tangential approach from June 2004 to May 2009. Ethical Committee approval was obtained. The study protocol conformed to the Helsinki declaration.
After obtaining informed consent from parents, subjects were screened with systemic arterial blood pressure, complete blood count, coagulation parameters, and urine analysis. PRB procedure was delayed after the management of uncontrolled hypertension, treatment of coagulopathy and urinary tract infection.
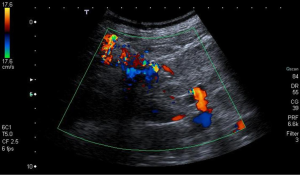
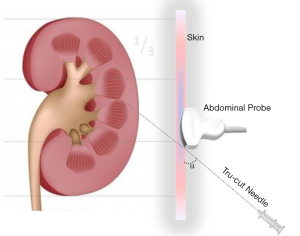
All procedures were performed under sedation with midazolam (0.03 mg/kg, IV), ketamine (1 mg/kg, IV) and locally administrated prilocaine (4 mL, 2%) combination due to the rapid effect, effective sedation and strong analgesia by the same radiologist (E.C.) (5). All ultrasound examinations were performed with a high-resolution ultrasound scanner (Toshiba Nemio 20; Toshiba Medical Systems Co, Ltd, Tokyo, Japan) equipped with a 3.5 to 5 MHz convex probe. Renal biopsies were performed utilizing an 18-gauge, 15 mm biopsy needle with a spring-loaded biopsy gun (Pro-Mag; Manan Medical Product, Northbrook, IL, USA). Core biopsy materials were obtained in prone position from the left kidney at least twice. The main characteristic of this technique is that the biopsy needle route with angle between 45-60 degrees with reference to the renal capsule or base line of the convex probe as much as possible with the tip of the needle directed away from the renal hilum into the corticomedullary region (Figure 1). This tract passed from the ‘Brödel’s line’ (a relatively avascular line between the anterior and posterior segmental branches of the renal artery) which is located posterior to the lateral convex border of the kidney (Figure 2) (6). We also used color Doppler mode imaging to avoid major vascular structures on the needle pathway. The central echogenic hilum was avoided (Figure 3). In the postprocedural follow-up, patients were instructed to remain in bed with a sandbag at back for 24 h following the biopsy. Vital signs were measured at half hour intervals for the first two hours and hourly for a day thereafter. Each urine sample voided was examined for gross hematuria for a day. Follow-up hemoglobin measurements were performed 2-4 and 6-12 h after biopsy. Doppler US examination of the punctured kidney has been performed in all patients on the next day and the patients were discharged after 24 h if there was no complication. Patients who developed macroscopic hematuria were followed up until the bleeding stopped. Patients with perirenal hematomas were discharged but US has been repeated at a two-week interval in outpatient clinics until hematomas resolved.
Complications have been classified as “major” and “minor”. Major complications are those which require a clinical intervention or invasive procedure, whether transfusions of blood components, the formation of an obstruction of the urinary tract with subsequent acute renal insufficiency, septicemia, or the death. Minor complications are those which do not require a clinical intervention beyond simple observation, such as transient macrohematuria, mild lumbar pain at the biopsy location, or a small perirenal hematoma (<5 cm) that will resorb spontaneously without the need for any intervention (1,2,7).
All biopsy specimens were studied by light microscopy and immunofluorescence microscopy at the Pathology Department of our hospital. Biopsy samples were subjected to preliminary evaluation under light microscope and in regions containing glomeruli; tissue was separated for immunofluorescence examination and frozen with liquid nitrogen. Biopsy material containing at least ten glomeruli has been considered as adequate for proper diagnosis.
Results
The biopsy method detailed herein was attempted in 166 patients (82 males, 84 females; mean age 8.1±3.0 years). Among cases indicated for biopsy, clinical presumptive diagnosis were as follows: 75 (45.2%) nephrotic syndrome, 39 (23.5%) nephritic syndrome, 24 (14.5%) hematuria and/or proteinuria, 23 (13.8%) renal failure (acute and chronic) with unknown reason, and 5 (3%) macroscopic hematuria.
According to the histopathological results, 38 (22.9%) cases were diagnosed with focal segmental glomerulosclerosis (FSGS), 29 (17.5%) with minimal change disease; 32 (19.3%) with Henoch Schönlein nephritis, 13 (7.8%) with membrano-proliferative glomerulonephritis (MPGN), 15 (9%) with acute post infectious nephropathy, 9 (5.4%) with amyloidosis; 9 (5.4%) with congenital nephrotic syndrome, 9 (5.4%) with hemolytic uremic syndrome, 6 (3.6%) with chronic nephropathy, and 2 (1.2%) with hereditary nephropathy. In three cases, renal biopsies revealed normal renal tissue. One case (0.6%) was not established any diagnosis due to inadequate material.
Recognized complications of PRB including pain that necessitated medical treatment or hospital admission, bleeding, blood transfusion, clinical hematoma, pneumothorax, or post-biopsy infection were not observed in the present study.
In patients who underwent surgery, there was no sign that biopsy either complicated the nephrectomy. The most frequently occurring minor complication was macroscopic hematuria, which occurred at the rate of 9.6%. Hematoma was detected in three cases and regressed spontaneously in all cases.
Discussion
Renal biopsy in children is considered technically more difficult than in adults (2,4). In May 2004, a consensus meeting among radiology, pathology and pediatric nefrology clinicians were performed for a better approach to decrease the rate of nondiagnostic biopsies and pediatric PRB was standardized for passing through Broödel’s line, which involved the angled tangential approach. In the present study, biopsy material was obtained from the posterolateral area. The speciality feature of the defined technique is that the biopsy needle route with angle between 45 and 60 degrees with reference to the renal capsule or base line of convex probe as much as possible with the tip of the needle directed away from the renal hilum for recieving into the corticomedullary region. The preferred site of the renal biopsy is the inferior pole of the left kidney because the renal pelvis and large caliber vessels are relatively far from this level (7-9). The superiority of angled tangential approach technique defined in this study over tangential technique defined by Patel et al. is that it increases rates of adequacy, and accuracy of the examination of the biopsy material in diseases involving only distal tubule and loop of Henle, rather than proximal nephron. In the study by Patel et al. adequacy of the biopsy material was quite improved in glomerular diseases. However, in diseases which involve components of distal nephron (distal tubuli, and loop of Henle) theoretically decrease the rates of accuracy, and adequacy. Since it is possible to obtain biopsy material from both proximal and distal components of nephron, procedural sensitivity and specificity will increase in all disease states independent of the diseased location of the nephron. The technique presented in this report mainly let the physician to get the biopsy samples from the appropriate site of the kidney with avoiding hilum.
Indication for renal biopsy was nephrotic syndrome, accounting for approximately 42-47% of patients (10,11). In the present study, the most frequent indication for PRB was also nephrotic syndrome (45.2%) which was followed by nephritic syndrome (23.5%).
The use of an automated gun for puncture under real-time ultrasound observation combines a noninvasive method of renal localization to a precise and fast system of PRB. This association of techniques improves the chance of yielding renal fragments with larger content of glomeruli and higher adequacy for histological analysis than those obtained by free hand, with potential reduction of the procedure’s inherent complications (12,13). In the present study, no renal tissue was obtained from one patient and the rate of inadequate material obtained was 0.6 percent. The most frequent histopathological group of diseases found in studies in the literature is primary glomerulonephritis in both children and adult patients (14,15). IgA nephropathy is the most frequent glomerulopathy in adults whereas MPGN and FSGS are the most common in children (14,15). In the present study, the most frequent histopathological finding was focal segmental glomerulosclerosis (22.9%). Histopathologically adequate tissue sampling was reported to be at the rate of 96% in literature, while in the present study the corresponding rate was 99.4% (16).
The frequency of major complications of PRB has varied substantially in different reports, being less than 1% in some reports and 5.6-6.6% in other series (8). The reasons for these differences are not readily apparent, but may be related to the patient population, method of renal biopsy, or operator experience. Walker et al. found that less than 1% of those with macroscopic hematuria require blood transfusion (17). Mortality is reported at the rate of 0.1% (4). The complication rate associated with the performance of PRB has significantly decreased in recent years as a result of the technological advances applied to the procedure. The use of automatic biopsy needles with guidance of US to localize the biopsy site and to visualize the needle trace for the execution of a safe procedure (1-3,7,8). In the present study, minor complications (including perirenal hematoma and macroscopic hematuria) occurred in 16 cases (9.6%) and no major complications were observed. To decrease the risk of hemorrhagic complications, we used color Doppler US guiding. The lower risk of major hemorrhagic complications with the ultrasound-guided technique may be attributable to the use of smaller biopsy needle (18-gauge) in the present study.
The main limitation of our study includes the retrospective design. In addition, some details of history and factors that may influence the outcome may not be completely documented. Due to these restrictions, associations should be interpreted with caution.
We have found the technique to work well under a variety of clinical conditions (that is. renal size, patient size, and underlying disease). Our complication rate and success rate in obtaining adequate renal tissue for diagnosis are comparable to that reported with the traditional techniques. Angled tangential approach may be considered for pediatric renal biopsies.
Acknowledgements
Disclosure: The authors declare no conflicts of interest.
References
- Patel MD, Phillips CJ, Young SW, et al. US-guided renal transplant biopsy: efficacy of a cortical tangential approach. Radiology 2010;256:290-6. [PubMed]
- Kersnik Levart T, Kenig A, Buturović Ponikvar J, et al. Real-time ultrasound-guided renal biopsy with a biopsy gun in children: safety and efficacy. Acta Paediatr 2001;90:1394-7. [PubMed]
- Tang S, Li JH, Lui SL, et al. Free-hand, ultrasound-guided percutaneous renal biopsy: experience from a single operator. Eur J Radiol 2002;41:65-9. [PubMed]
- Fogo A. Renal Pathology. In: Barratt TM, Avner ED, Harmon WE. eds. Pediatric Nephrology, fourth edition. Baltimore: Lippincott Williams&Wilkins, 1999:391-413.
- Astuto M, Disma N, Crimi E. Two doses of oral ketamine, given with midazolam, for premedication in children. Minerva Anestesiol 2002;68:593-8. [PubMed]
- Sampaio F, Uflacker R. eds. Renal anatomy applied to urology, endourology, and interventional radiology. New York: Thieme Medical Publishers, Inc, 1993.
- Uppot RN, Harisinghani MG, Gervais DA. Imaging-guided percutaneous renal biopsy: rationale and approach. AJR Am J Roentgenol 2010;194:1443-9. [PubMed]
- Hussain F, Watson AR, Hayes J, et al. Standards for renal biopsies: comparison of inpatient and day care procedures. Pediatr Nephrol 2003;18:53-6. [PubMed]
- Whittier WL, Korbet SM. Timing of complications in percutaneous renal biopsy. J Am Soc Nephrol 2004;15:142-7. [PubMed]
- Sumboonnanonda A, Srajai K, Vongjirad A, et al. Percutaneous renal biopsy in children. J Med Assoc Thai 2002;85 Suppl 2:S755-61. [PubMed]
- Carvalho E, do Sameiro Faria M, Nunes JP, et al. Renal diseases: a 27-year renal biopsy study. J Nephrol 2006;19:500-7. [PubMed]
- Cozens NJ, Murchison JT, Allan PL, et al. Conventional 15 G needle technique for renal biopsy compared with ultrasound-guided spring-loaded 18 G needle biopsy. Br J Radiol 1992;65:594-7. [PubMed]
- Kumar A, Mitchell MJ, Aggarwal S, et al. Ultrasonography-directed native renal biopsy: comparison of an automated biopsy device with a needle system. Can Assoc Radiol J 1992;43:359-63. [PubMed]
- Li LS, Liu ZH. Epidemiologic data of renal diseases from a single unit in China: analysis based on 13,519 renal biopsies. Kidney Int 2004;66:920-3. [PubMed]
- Chen H, Tang Z, Zeng C, et al. Pathological demography of native patients in a nephrology center in China. Chin Med J (Engl) 2003;116:1377-81. [PubMed]
- Melk A. Tool for renal tissue analysis. In: Geary DF, Schaefer F. eds. Comprehensive pediatric nephrology. Philadelphia: Mosby Elsevier, 2008:55-61.
- Walker PD. The renal biopsy. Arch Pathol Lab Med 2009;133:181-8. [PubMed]