
Traumatic ectopic dislocation of testis: an easily overlooked occurrence of blunt injury in polytrauma patients
Introduction
Blunt scrotal injuries are more and more frequent (1-5). Testicular dislocation is an uncommon complication, often due to a direct trauma to the fuel tank in motorcycle accident (6-9). Currently, there is no consensus in radiological, medical and surgical management of such a setting. We report a case of pubic testicular dislocation in a high velocity highway motorcycle accident. Although theoretically accessible to clinical diagnosis, the intensive care of these polytrauma patients often lead to a dramatic diagnosis delay. Early recognition of the radiological signs of testicular dislocation is essential to allow an emergency surgical management, necessary to preserve the normal spermatogenic function in the dislocated testis.
Case presentation
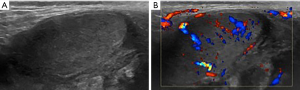
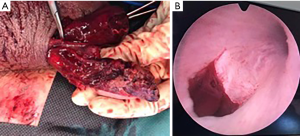
A 35-year-old man involved in a high-kinetic motorcycle accident was referred to our radiology department in a context of acute alcohol abuse. At admission, the patient was hemodynamically stable, and complained about diffuse pelvic pain. The clinical examination revealed a urethrorrhagia. The whole body computed tomography (CT) scan systematically done for high energy trauma was completed with an additional late excretory urogram which showed a horseshoe kidney with no complication and two non-displaced fractures of the ilio-pubic branches. Lower slices of the abdominopelvic CT scan showed an empty right hemiscrotum (Figure 1). The enhancement of the right spermatic cord revealed its curvature, ending in contact with a median and pre-pubic ovoid mass with soft tissue density and peripheral fat stranding (Figure 1). These findings were suspicious for a traumatic pubic testicular dislocation. A complementary ultrasound (US) examination was performed and revealed a large right scrotal hematocele. The dislocated testis was slightly heterogeneous, hypoechoic, and had finely irregular contours (Figure 2). The Doppler US study found a homogeneous vascularization, with resistive index of intrascrotal arteries systematically measured between 0.56 and 0.60. In spite of the US findings, a rupture of the tunica albuginea was evoked. The patient was treated urgently by surgery. It allowed, on one hand, to confirm the testicular dislocation with complete rupture of the tunica albuginea, the externalization of the pulp, and the rupture of the epididymis and vas deferens; on the other hand, it revealed a pre-membranous urethral lesion responsible for the urethral bleeding (Figure 3). A unilateral orchidectomy through a scrotal approach had to be performed with simple operative follow-up.

Discussion
Testicular dislocation is defined as an abnormal displacement of the testis outside the scrotum due to blunt trauma. Since its first description in 1809 by Claubry et al. (1), traumatic testicular dislocation remains a rare entity with only a hundred cases reported to date in the literature (1-11).
It occurs in more than 80% of cases in motorcycle accidents, in young patients (2,3). Compression of the scrotum and perineum against the fuel tank would be responsible for the scrotal hyperpressure necessary to dislocate the testis. According to Alyea et al. (4), the dislocated testis could then be displaced along a circle within the radius of the spermatic cord centered on the external inguinal ring. These hypothetic locations and their reported frequency have been described by Schwartz et al. (5). Superficial inguinal dislocations account for more than half of all cases (6). At the other end of the spectrum, intra-canalicular abdominal and inguinal dislocations are exceptional and almost always associated with pre-existing inguinal hernias (7,8).
Once the testicular dislocation diagnosis is made, prompt treatment should be established (7-9). In case of early diagnosis of superficial inguinal dislocation, some authors recommend a manual reduction attempt (2,5,6,10). If not possible, short-term complications are numerous and include important inflammatory reaction responsible for pain and adhesions, infection of the hematocele, and twisting or necrosis of the testis (10). On the long-term, cases of hypofertility due the appearance of anti-spermatozoal antibodies secondary to the contact between the germinal cells and the immune system have also been described (11-13). Regarding traumatic testicular dislocation in the public position, only 7 cases have been reported to date in the literature (2,14,15). The diagnosis was immediately made in 5 cases, including 3 on the CT scan. For the other 2 patients, the initial CT scan was considered normal because overlooked, resulting in a 12- and 60-day diagnosis delay. The first one underwent surgical reduction requiring adhesiolysis, and the second one got orchidectomy due to a necrosis of the dislocated testis caused by an outdated twist. In the present case, the diagnosis was evoked on the whole-body CT scan and immediately confirmed by an US examination. Discrete US abnormalities in B mode led to an early surgical exploration. This revealed an important discrepancy between the initial suspicious US findings and the final severity of the lesions identified intraoperatively, leading to an orchidectomy in a non-adherent environment because of non-repairable lesions. The post-operative follow-up was simple without any complications and with short hospital discharge. Overall, out of the 8 cases of pubic traumatic testicular dislocation, only 2 could be reduced manually (2). Testicular pubic dislocations are therefore more frequently complicated, and should be discussed for emergency surgical exploration.
Conclusions
Traumatic testicular dislocation is rare but not exceptional. The delay for diagnosis, which is the rule in these polytrauma patients, can lead to irreversible testicular damage. However, cross-sectional imaging and especially whole body-CT scan usually allows an early diagnosis. The analysis of the scrotal content in the polytrauma patient must therefore be systematic, and particularly for high velocity motorcycle accident victims. Among traumatic testicular dislocations, pubic location is unfrequent but appears more often associated with traumatic testicular lesions. According to these findings, pubic traumatic testicular dislocation should motivate emergent surgical exploration in order to guide the appropriate therapeutic management.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Claubry E. Observation sur une rétrocession subite des deux testicules dans l’abdomen, à la suite d’une violente compression de la partie inférieure de la paroi abdominale par une roue de charette. J Gen Med Chir Pharm 1818;64:325.
- Zavras N, Siatelis A, Misiakos E, Bagias G, Papachristos V, Machairas A. Testicular dislocation after scrotal trauma: a case report and brief literature review. Urol Case Rep 2014;2:101-4. [Crossref] [PubMed]
- Kochakarn W, Choonhaklai V, Hotrapawanond P, Muangman V. Traumatic testicular dislocation a review of 36 cases. J Med Assoc Thai 2000;83:208-12. [PubMed]
- Alyea EP. Disolcation of testis. Surg Gynecol Obstet 1929;49:600-16.
- Schwartz SL, Faerber GJ. Dislocation of the testis as a delayed presentation of scrotal trauma. Urology 1994;43:743-5. [Crossref] [PubMed]
- Bromberg W, Wong C, Kurek S, Salim A. Traumatic bilateral testicular dislocation. J Trauma 2003;54:1009-11. [Crossref] [PubMed]
- Munter DW, Faleski EJ. Blunt scrotal trauma: emergency department evaluation and management. Am J Emerg Med 1989;7:227-34. [Crossref] [PubMed]
- Morgan A. Traumatic luxation of the testis. Br J Surg 1965;52:669-72. [Crossref] [PubMed]
- Feder M, Sacchetti A, Myrick S. Testicular dislocation following minor scrotal trauma. Am J Emerg Med 1991;9:40-2. [Crossref] [PubMed]
- Madden JF. Closed reduction of a traumatically dislocated testicle. Acad Emerg Med 1994;1:272-5. [Crossref] [PubMed]
- Ko SF, Ng SH, Wan YL, Huang CC, Lee TY, Kung CT, Liu PP. Testicular dislocation. Ann Emerg Med 2004;43:371-5. [Crossref] [PubMed]
- Nagler HM, White RD. The effect of testicular torsion on the contralateral testis. J Urol 1982;128:1343-8. [Crossref] [PubMed]
- Hayami S, Ishigooka M, Suzuki Y, Sasagawa I, Nakada T, Mitobe K. Pathological changes of traumatic dislocated testis. Urol Int 1996;56:129-32. [Crossref] [PubMed]
- Neistadt A. Bilateral traumatic dislocation of the testis. J Urol 1967;97:1057-8. [Crossref] [PubMed]
- Edson M, Meek JM. Bilateral testicular dislocation with unilateral rupture. J Urol 1979;122:419-20. [Crossref] [PubMed]


