
Some radiographically ‘occult’ osteoporotic vertebral fractures can be evidential if we look carefully
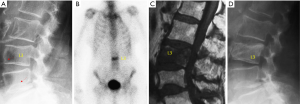
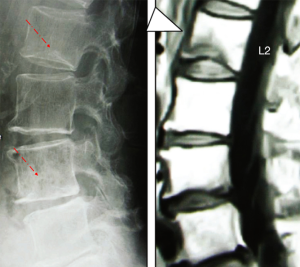
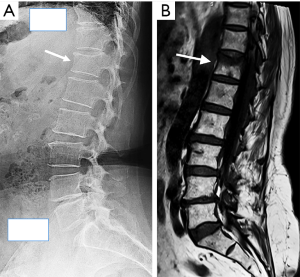
It has been well documented that acute osteoporotic vertebral fractures (OVF) can have no visible deformation of vertebral body, and these OVFs are commonly termed as radiographically ‘occult’ (1-4). Magnetic resonance imaging (MRI) can help the diagnosis of these occult OVFs. However, some of these ‘occult’ OVF are actually radiographically evidential if we look carefully.
Though vertebral endplate depression and anterior cortex buckling have been noted as signs of OVF (5-11), their significance may not have been well recognized by all spine radiograph readers (radiologists, orthopedic surgeons, rheumatologists, etc.). OVF is generally considered to be associated with vertebral body height loss; however, it is not always the case, particularly at the early phase. In our recent analysis of radiological reports for spine radiograph referred due to back pain, it was noted that osteoporotic ECF (endplate and/or cortex fracture) without vertebral body height loss was commonly missed (12). On the other hand, no singular moderate/severe OVF (one OVF in one patient) was missed; though OVFs at multiple levels were often under-reported, i.e., not all OVFs were precisely reported (12).
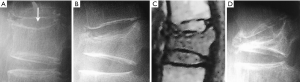
Hereby we present a few cases of OVFs in the literatures (Figures 1-3), which were originally considered to be ‘occult’ OVF. Thus, the prevalence of ‘occult’ OVF may have been over-estimated. These cases illustrate the importance of recognizing ECF. Note the relevance of ECF has been emphasized in Genant’s original paper on OVF semi-quantitative grading (5), as well as many following articles (6-11,13,14). In some cases, acute ECF with minimal vertebral deformity can quickly progress to vertebral collapse (Figure 4). For radiograph of elderly female patients with a history of acute back pain in a setting of possible osteoporosis, close attention should be paid to look at vertebral endplate depression and anterior cortex buckling, particularly for vertebral levels with OVF high risk (10,11,15,16). With adequate training, radiologists can play a unique role in correctly interpreting the fine details of spine radiograph, and contribute to the clinical care for patients with OVF (17).
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Kanchiku T, Taguchi T, Kawai S. Magnetic resonance imaging diagnosis and new classification of the osteoporotic vertebral fracture. J Orthop Sci 2003;8:463-6. [Crossref] [PubMed]
- Pham T, Azulay-Parrado J, Champsaur P, Chagnaud C, Legré V, Lafforgue P. "Occult" osteoporotic vertebral fractures: vertebral body fractures without radiologic collapse. Spine (Phila Pa 1976) 2005;30:2430-5. [Crossref] [PubMed]
- Terakado A, Orita S, Inage K, Kubota G, Kanzaki T, Mori H, Shinohara Y, Nakamura J, Matsuura Y, Aoki Y, Furuya T, Koda M, Ohtori S. A Clinical Prospective Observational Cohort Study on the Prevalence and Primary Diagnostic Accuracy of Occult Vertebral Fractures in Aged Women with Acute Lower Back Pain Using Magnetic Resonance Imaging. Pain Res Manag 2017;2017:9265259.
- Marongiu G, Congia S, Verona M, Lombardo M, Podda D, Capone A. The impact of magnetic resonance imaging in the diagnostic and classification process of osteoporotic vertebral fractures. Injury 2018;49 Suppl 3:S26-31. [Crossref] [PubMed]
- Genant HK, Wu CY, van Kuijk C, Nevitt MC. Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 1993;8:1137-48. [Crossref] [PubMed]
- Yoshida T, Nanba H, Mimatsu K, Kasai T. Treatment of osteoporotic spinal compression fractures. Conservative therapy and its limitation. Clin Calcium 2000;10:53-8.
- Jiang G, Eastell R, Barrington NA, Ferrar L. Comparison of methods for the visual identification of prevalent vertebral fracture in osteoporosis. Osteoporos Int 2004;15:887-96. [Crossref] [PubMed]
- Ito Z, Harada A, Matsui Y, Takemura M, Wakao N, Suzuki T, Nihashi T, Kawatsu S, Shimokata H, Ishiguro N. Can you diagnose for vertebral fracture correctly by plain X-ray? Osteoporos Int 2006;17:1584-91. [Crossref] [PubMed]
- Wáng YXJ, Che-Nordin N. Informed communication with study subjects of radiographically detected osteoporotic vertebral deformity. Quant Imaging Med Surg 2018;8:876-80. [Crossref] [PubMed]
- Wáng YXJ, Santiago RF, Deng M, Nogueira-Barbosa MH. Identifying osteoporotic vertebral endplate and cortex fractures. Quant Imaging Med Surg 2017;7:555-91. [Crossref] [PubMed]
- Wáng YXJ, Deng M, He LC, Che-Nordin MN, Santiago RF. Osteoporotic vertebral endplate and cortex fractures: a pictorial review. J Orthop Translat 2018;15:35-49. [Crossref] [PubMed]
- Du MM, Che-Nordin N, Ye PP, Qiu SW, Yan ZH, Wang YX. Underreporting characteristics of osteoporotic vertebral compressive fracture in back pain clinic patients of a tertiary hospital in China. J Orthop Translat 2020. [Crossref]
- Lentle BC, Berger C, Probyn L, Brown JP, Langsetmo L, Fine B, Lian K, Shergill AK, Trollip J, Jackson S, Leslie WD, Prior JC, Kaiser SM, Hanley DA, Adachi JD, Towheed T, Davison KS, Cheung AM, Goltzman D. CaMos Research Group. Comparative Analysis of the radiology of osteoporotic vertebral fractures in women and men: cross-sectional and longitudinal observations from the Canadian Multicentre Osteoporosis Study (CaMos). J Bone Miner Res 2018;33:569-79. [Crossref] [PubMed]
- Wáng YXJ, Che-Nordin N, Deng M, Leung JCS, Kwok AWL, He LC, Griffith JF, Kwok TCY, Leung PC. Osteoporotic vertebral deformity with endplate/cortex fracture is associated with higher further vertebral fracture risk: the Ms. OS (Hong Kong) study results. Osteoporos Int 2019;30:897-905. [Crossref] [PubMed]
- Lentle B, Trollip J, Lian K. The radiology of osteoporotic vertebral fractures redux. J Clin Densitom 2016;19:40-7. [Crossref] [PubMed]
- Che-Nordin N, Deng M, Griffith JF, Leung JCS, Kwok AWL, Zhu YQ, So RHY, Kwok TCY, Leung PC, Wáng YX. Prevalent osteoporotic vertebral fractures more likely involve the upper endplate than the lower endplate and even more so in males. Ann Transl Med 2018;6:442. [Crossref] [PubMed]
- Guglielmi G, Balzano RF, Cheng X. What is changed in the diagnosis of osteoporosis: the role of radiologists. Quant Imaging Med Surg 2018;8:1-4. [Crossref] [PubMed]


