Transcervical excision combined with uniportal VATS for apical ganglioneuroma: a case report
Introduction
Masses in the posterior mediastinum are commonly encountered by thoracic surgeons. Neurogenic tumors are the most common of these entities (1). A review of systems may identify symptoms of mass effect, including pain, dysphagia, dyspnea, stridor, cough, or Horner’s syndrome. Ganglioneuroma is a clinically uncommon benign tumor arising from the neural crest with further terminal neuronal differentiation into ganglion cells (2). It can occur at any age but is most commonly found in adults. Surgical resection without additional therapy is usually curative (3). Ganglioneuroma can occupy the whole thoracic outlet to the neck. The resection of such tumors should be carefully deliberated upon to avoid injuring the surrounding structures.
Case report
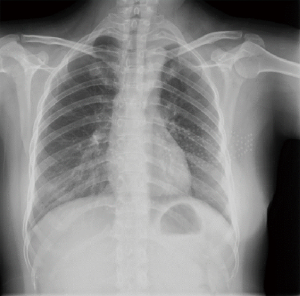
A female patient, 35 years old, was admitted to the hospital for a progressively aggravating left eyelid ptosis lasting 1 month. Since she was already suffering from Down’s syndrome, her symptoms were initially ignored, but after admission and the completion of examinations, she was diagnosed with Horner’s syndrome. Laboratory tests were unremarkable. Further contrast-enhanced computed tomography (CT) scan showed a 7×8 cm2 tumor located in the left apical chest (Figure 1), adjacent to the subclavian artery, with a suspected thin branch arising from the subclavian artery passing superior to the tumor.

Since the patient could not tolerate noise from magnetic resonance imaging (MRI), she was unable to complete an MRI examination. Combined with the patient’s symptoms and imaging findings, a preliminary diagnosis of ganglioneuroma originating from the sympathetic trunk was made. Since this type of tumor usually has a hard texture and the tumor body is relatively large, if the patient undergoes intrathoracic management, we face the risk of injuring the thin branch arising from the subclavian artery. It is very difficult to expose the artery and control the bleeding through the thoracic incision. Moreover, considering that this tumor is benign, it is not advisable to make a large incision. For this reason, we decided to ask the hand surgery department to collaborate on this surgery to add a transcervical incision to isolate the subclavian artery, vein, and brachial plexus nerves.
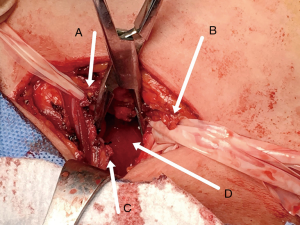
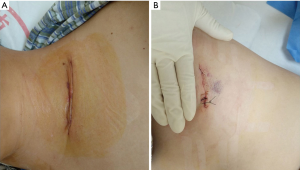
After the insertion of a double-lumen endobronchial tube and the administration of general anesthesia, the patient was first placed in the supine position. Then, an incision was made on the left neck posterior to the clavicle; thereafter, the incision was gradually dissected to expose the left apical thorax. First, we isolated the subclavian artery and explored under the artery to determine the upper margin of the tumor, which had a relatively hard texture. Then, we carefully looked for the thin branch arising from the subclavian artery. The branch was found to be leaching into the upper margin of the tumor, and it was removed after ligation of the proximal and distal ends. Next, a ribbon was used to pull back the subclavian artery, and the separation of C5–T1 nerve roots was performed (Figure 2). A ribbon was used to separate and expose each nerve root. Then, fingers were used to perform a blunt separation of the upper margin of the tumor, which was pushed inside the thoracic cavity. At this point, the upper margin of the tumor, the large vessels in the thoracic outlet, and the brachial plexus nerves had been completely isolated. Next, the patient was positioned in the right lateral position to undergo video-assisted thoracoscopic surgery (VATS). The neck and thorax were sterilized, and an incision was made in the fifth intercostal space at the anterior axillary line (Figure 3). After entering the thoracic cavity, the tumor was freed by pulling it downwards with one hand and transcervically using the other hand for blunt dissection to push it intrathoracically. Next, complete resection of the tumor was performed intrathoracically, and the tumor was removed from the incision on the fifth intercostal space (Figure 4). One drainage tube was placed into the thoracic cage through the fifth intercostal incision and was removed the day after surgery because of no air leakage and minimal drainage. The patient was discharged 2 days after surgery. During the follow-up, her Horner’s syndrome had slightly improved, and chest X-ray showed pleural thickening in the thoracic outlet (Figure 5).

Discussion
Apical thoracic masses have always been a great challenge in thoracic surgery, which is why robotic surgery is a good option for ganglioneuromas in this region (3). It allows for fine manipulation in a narrow space; however, not all centers have such good hardware conditions. In recent years, the application of a cervical incision has been increasing in thoracic surgery departments. Apart from thymus surgery via a cervical incision (4), an incision on one side of the neck can be used for a lobectomy (5,6). In this case, the presence of an arterial branch arising from the subclavian artery poses a potential threat for intrathoracic surgery. Moreover, dissection under direct vision with a transcervical incision is safer because it greatly decreases the possibility of damage to vessels in the apical thorax or nerves in the brachial plexus. At the same time, we made sure to use blunt dissection to separate the nerve canals, or sometimes bipolar coagulation hemostasis was used, because this ensured minimal energy damage to the nerves. In summary, regardless of whether a traditional posterolateral incision or traditional thoracoscopic surgery is performed, the duration of energy device usage is significantly longer in an intrathoracic operation towards the apical thorax than a transcervical operation under direct vision. Indeed, there is an increased potential risk of damaging nerves when dealing with the apical lobe. Therefore, operation difficulty is greatly reduced if the first cervical incision and dissection are performed to pull the tumor from this region into the thoracic cavity, followed by an intrathoracic operation where rapid resection of the tumor can be performed under thoracoscopy. In her postoperative follow-up, the patient showed no signs of aggravated Horner’s syndrome, and postoperative radiologic findings were also satisfactory.
Conclusions
For thoracic surgery centers that do not own robotic surgery equipment, and if the tumor occupies the thoracic outlet, the two-step method of transcervical incision followed by intrathoracic resection is a safe and effective method. In detail, transcervical dissection and separation of the tumor from its surrounding nerves and vessels should be performed first to pull the tumor into the thoracic cavity. Finally, intrathoracic dissection and finally resection of the tumor under thoracoscopy are carried out.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Reeder LB. Neurogenic tumors of the mediastinum. Semin Thorac Cardiovasc Surg 2000;12:261-7. [Crossref] [PubMed]
- Mora J, Gerald WL. Origin of neuroblastic tumors: clues for future therapeutics. Expert Rev Mol Diagn 2004;4:293-302. [Crossref] [PubMed]
- Linnik YA, Hoegemann Savellano D, Phillips JD, Black CC. A. 49-year-old woman with right apical thoracic mass. Chest 2017;152:e133-8. [Crossref] [PubMed]
- Kumazawa S, Ishibashi H, Takahashi K, Okubo K. Transcervical excision of thymoma and video-assisted thoracoscopic extended thymectomy (VATET) for ectopic cervical thymoma with myasthenia gravis: report of a case. Gen Thorac Cardiovasc Surg 2016;64:752-4. [Crossref] [PubMed]
- Zieliński M, Nabialek T, Pankowski J. Transcervical uniportal pulmonary lobectomy. J Vis Surg 2018;4:42. [Crossref] [PubMed]
- Zieliński M, Rybak M, Solarczyk-Bombik K, Wilkojc M, Czajkowski W, Kosinski S, Fryzlewicz E, Nabialek T, Pankowski J. Uniportal transcervical video-assisted thoracoscopic surgery (VATS) approach for pulmonary lobectomy combined with transcervical extended mediastinal lymphadenectomy (TEMLA). J Thorac Dis 2017;9:878-84. [Crossref] [PubMed]