Primary intraosseous Kaposi’s sarcoma of the maxilla in AIDS: a case report
Introduction
Kaposi’s sarcoma (KS), first reported by Moritz Kaposi in 1872, is a neoplasm that occurs rarely in Asians (1). With the onset of the acquired immunodeficiency syndrome (AIDS) epidemic, KS became recognized as the most common malignancy in AIDS patients, and an AIDS-defining condition (2). KS can involve virtually any organs such as mucocutaneous tissues, lymph nodes, and visceral organs are the most frequently affected locations. Of intraosseous lesion, KS of maxilla is extremely rare, with only seven previously reported cases involving the maxilla, including one primary intraosseous KS of maxilla in an HIV-infected patient (3-7). We present an additional case of primary intraosseous KS of the maxilla in an AIDS patient. To our knowledge, this is the first case report of maxilla KS in a Chinese AIDS patient.
Case report
A 44-year-old Chinese male with serological evidence of HIV infection was referred to our hospital. His main chief complaint was mild swelling on the left-side face for more than one year and lasting pain at the same location for the past two weeks. The patient had no cutaneous lesions consistent with KS on his trunk. His risk factor for HIV infection was homosexuality, with no history of intravenous drug use or blood product transfusion. His CD4 T-lymphocyte count was 107 cells/mm3 and this qualified him for the diagnosis of AIDS. The patient didn’t start any antivirul therapy before his admission, and his past medical record was unremarkable.
Clinical examination showed mild swelling on patient’s left face, and skin tenderness was positive at the same location, but no skin pigmentation. No external nasal deformity was found. No bilaterally cervical lymph node enlargement was palpated. There was inferior turbinates swelling bilaterally. Bilateral tonsils showed neither enlargement nor red surface appearance. Bilateral external auditory canals were clear and tympanic membrane integrity was intact without perforation.
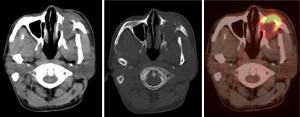
After physical examination a maxillary sinus computed tomography (CT) scan was performed at the same day when the patient was admitted. The CT scan revealed that the subcutaneous soft tissue surrounding left maxillary sinus was mild swollen, the left maxillary sinus was filled with soft tissue, and there were osteolytic lesions in anterior, posterior and basal walls of the left maxillary sinus (Figure 1). No intravenous contrast media was used when CT scan was performed.
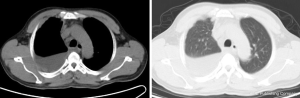
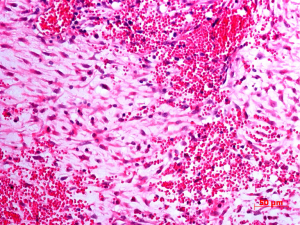
At the same time chest X-ray showed right-side pleural effusion. After that chest CT was performed revealing mediastinal adenopathy and right basilar atelectasis because of pleural effusion (Figure 2). Abdominal US revealed slightly hepatosplenomegaly and portal vein dilation with a 1.5 cm diameter. A biopsy of maxillary sinus was performed. The histological features of removal tissue were consistent with AIDS-associated KS (Figure 3).
Because of neoplasm found at the maxillary sinus and multiple mediastinal adenopathy at the chest CT, a whole body F-18 fluorodeoxyglucose positron emission tomography and computed tomography (PET/CT) was performed for detecting other metastasis. PET/CT showed a high metabolic lesion in the left maxilla. The standard uptake value (SUV), measured in the region of interest placed on this lesion, was 9.2, and the lesion was confirmed to involve the bony walls and adjacent soft tissues (Figure 1). Also considered metastases were nodular and line-shaped lesions, with a maximum SUV of 10.9, on the right pleura. Multiple lymph nodes metastases were detected in bilateral sternocleidomastoid muscle regions, bilateral axillary fossa, right hilum, mediastineum, paraaortic region and bilateral inguinal areas.
Discussion
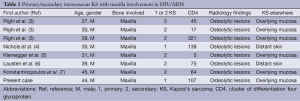
In 1872, Moritz Kaposi, an Austrian dermatologist, first reported this unusual vascular neoplasm found on the lower extremities of eastern European men. He described multiple macules and plaques of dark pigmented skin lesions (1). In the past, KS was thought to be an aged-related cutaneous disease in European men, while the onset of AIDS has shifted much of the incidence of KS development toward the head and neck. The incidence of intraoral mucosal involvement has been reported to be as high as 50% (4). Other maxillofacial sites less frequently affected include the lips, masseter muscle, and the parotid gland (8,9). Although KS can occur in many organs, but osseous lesion is rarely observed in KS. The first KS with osseous involvement was recognized in 1899, often in the bones of hand, leg, foot, and vertebrae, prior to the AIDS epidemic (9). Patients with osseous KS usually have concomitant nonosseous KS lesions eroding into underlying bones, particularly those with AIDS. Very few cases have had primary intra-osseous KS (10,11). KS involving the maxilla in HIV/AIDS is more rarely seen. To date, there have been seven reported cases of KS involving the maxilla, including one case with primary intraosseous involvement (Table 1) (3-7). Nichols et al. (4) described a maxillary KS lesion protruding from the anterior maxillary region and extending into the mucobuccal fold. A poorly defined radiolucency accompanied by tooth sensitivity and mobility was present. The patient was reported to be disease-free 20 months after initial KS diagnosis.
Radiology may play an important role in early diagnosis and treatment planning in this population, in whom clinical and laboratory findings are commonly equivocal and nonspecific. KS-related osseous lesion manifested as rarefaction, cystic lesions, or complete bone destruction, mainly were osteolytic, and rarely was there an associated periosteal reaction (12-14). We noted that all the osseous lesions of KS at maxilla had an osteolytic appearance radiologically (see Table 1). Usually intraosseous KS can be identified in plain radiographs as a radiolucent area consistent with osteolysis, however the bone destruction occurrence of KS in any of atypical sites such as maxilla may prove difficult to diagnose on plain X-ray films, particularly if patients are asymptomatic, lesions often go unrecognized on routine imaging studies.
Full table
Computed tomography scanning is helpful in detecting and assessing the involvement of deep tissue planes and the extent of disease. On CT scan, KS appears as homogeneous, hypodense osseous lesions with little surrounding edema and minimal mass effect. CT gives a more detailed characterization of lytic bone changes. Konstantinopoulos PA et al. (7) reported a case of KS of the hard palate which invaded the underlying maxillary bone. Coronal maxillofacial CT showed erosion of the floor of the left maxillary sinus and thickening of the left maxillary sinus mucosa. On occasions, radiographic evaluation of intraosseous KS lesions of the maxilla notes root absorption of the involved teeth (4).
Because of its direct multiplanar capability and superior tissue differentiation, magnetic resonance imaging (MRI) can be very helpful in evaluating neoplasms of the sinonasal region, whereas CT and plain radiographs may be more limited in defining soft tissue planes. MRI is outstanding in depicting bone marrow abnormalities, as seen in lymphoma or infection, and can be more sensitive for detecting the involvement of spongy bone (15). There were some reports about MRI findings of KS in other locations but rarely were about the maxilla (13). As for PET scanning of KS, the results of our case show high metabolic in the left maxilla with SUV as high as 9.2, and many other high metabolic lesions which were considered to be metastasis were revealed, such as pleura and lymph nodes. PET was helpful in revealing and localizing lesions. In most cases, Radiography, CT, and MR imaging are complementary in the evaluation of KS as the cause of osseous lesion in HIV-infected and AIDS patients. Nevertheless, biopsy is necessary for definitive diagnosis.
The etiology of KS remains unknown. Literatures suggested that human herpesvirus 8 (HHV-8, another name of Kaposi sarcoma herpes virus) is involved in the development of AIDS associated KS. For the intraosseous lesion of jaw, infectious etiologic agents such as atypical mycobacteria, cytomegalovirus, anaerobic organisms, and fungi may cause radiolucent jaw lesions. In AIDS patients the decrease in the body’s defense mechanisms secondary to HIV infection predisposes these individuals to a variety of complications that can affect the bones, including various opportunistic infections, immune-related neoplasm and osteoporosis. The underlying mechanisms leading to these diseases are complex and not fully understood but are thought to be multi-factorial.
The differential diagnosis of maxillary bone destruction in an HIV-seropositive patient includes periodontal abscess, lymphoma, necrotising ulcerative periodontitis, opportunistic infections caused by atypical mycobacteria or fungi, and neoplasia. Non-Hodgkin’s lymphoma (e.g., plasmablastic lymphoma) is probably the most common malignancy associated with involvement of the maxilla or mandible (7). Another differential disease is bacillary angiomatosis. Osteolytic lesions are a relatively common feature of bacillary angiomatosis in patients with HIV infection. Older articles have suggested that the presence of bone lesions helps differentiate bacillary angiomatosis from AIDS-related KS, which has similar cutaneous abnormalities but usually no associated bone lesions. Although bacillary angiomatosis is still the most likely cause of osseous lesions in a patient with AIDS, it behooves the clinician to be cognizant that KS can have a similar presentation.
In summary, KS is a common opportunistic neoplasm of patients with AIDS, typically arising on the skin and mucosa, while rare cases have been reported arising in the maxilla. This case represents the first known instance of primary maxilla KS with cutaneous involvement in a Chinese AIDS patient. It is important for the radiologists to be familiar with the different types of osseous lesion in HIV-infected and AIDS patients so that an appropriate differential diagnosis can be established from the images obtained in these individuals.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Kaposi M. Idiopathic multiple pigmented sarcomas of skin Arch Dermatol Syph 1872;3:265-73.
- Safai B, Diaz B, Schwartz J. Malignant neoplasms associated with human immunodeficiency virus infection. CA Cancer J Clin 1992;42:74-95. [PubMed]
- Righi P, Pierleoni L, Ficarra G. Bone involvement of the jaws in AIDS-related Kaposi’s sarcoma Minerva Stomatol 1994;43:521-4. [PubMed]
- Nichols CM, Flaitz CM, Hicks MJ. Primary intraosseous Kaposi’s sarcoma of the maxilla in human immunodeficiency virus infection: review of literature and report of case. J Oral Maxillofac Surg 1995;53:325-9. [PubMed]
- Kleinegger CL, Sarubin D. Intraoral Kaposi’s sarcoma associated with alveolar bone erosion. Miss Dent Assoc J 1996;52:14-5. [PubMed]
- Lausten LL, Ferguson BL, Barker BF, et al. Oral Kaposi sarcoma associated with severe alveolar bone loss: case report and review of the literature. J Periodontol 2003;74:1668-75. [PubMed]
- Konstantinopoulos PA, Goldsztein H, Dezube BJ, et al. Acquired immunodeficiency syndrome related Kaposi’s sarcoma eroding the maxillary bone. J Laryngol Otol 2008;122:993-7. [PubMed]
- Ficarra G, Berson AM, Silverman S Jr, et al. Kaposi’s sarcoma of the oral cavity: a study of 134 patients with a review of the pathogenesis, epidemiology, clinical aspects, and treatment. Oral Surg Oral Med Oral Pathol 1988;66:543-50. [PubMed]
- Lee Morgan C, Gehweiler JA Jr. Kaposi’s sarcoma in bone: a case report with unusual radiographic findings and an abnormal radioisotope scan. Rev Interam Radiol 1976;1:37-41. [PubMed]
- Bhandari M, Kempin S, Aziz MS. AIDS-related osseous Kaposi sarcoma. AIDS Read 2007;17:202-3, 205. [PubMed]
- Omeis I, Siems AL, Harrington W, et al. Spinal Kaposi sarcoma presenting without cutaneous manifestations. Case report. J Neurosurg Spine 2007;7:558-61. [PubMed]
- Thanos L, Mylona S, Kalioras V, et al. Osseous Kaposi sarcoma in an HIV-positive patient. Skeletal Radiol 2004;33:241-3. [PubMed]
- Restrepo CS, Martínez S, Lemos JA, et al. Imaging manifestations of Kaposi sarcoma. Radiographics 2006;26:1169-85. [PubMed]
- Caponetti G, Dezube BJ, Restrepo CS, et al. Kaposi sarcoma of the musculoskeletal system: a review of 66 patients. Cancer 2007;109:1040-52. [PubMed]
- Restrepo CS, Martínez S, Lemos JA, et al. Imaging manifestations of Kaposi sarcoma. Radiographics 2006;26:1169-85. [PubMed]


