
Brain magnetic resonance imaging of Joubert syndrome: case presentation in a child
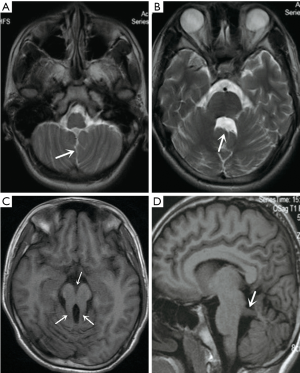
A 16-year-old boy was admitted to our hospital due to sudden pale face and chest pain for half-an-hour. He could not express properly because of hypophrenia. Other examinations revealed congenital cataract in the right eye, as well as nystagmus and generalized hypotonia. He had signs of ataxia, and, though without deformity in any limb, was unable to complete the straight-line walking test. Five years ago, the boy was abandoned to a welfare home. The caretaker of the welfare home complained that the boy had several times of episodic hyperpnea, every 1–2 h, each lasting for about 10–40 s, during the night sleep. Ultrasonography of liver, cholecyst, pancreas, spleen, kidney and heart showed no abnormal findings. Electrocardiogram showed sinus arrhythmia. Magnetic resonance imaging (MRI) of the brain showed a cerebrospinal fluid line between the bilateral cerebellar hemispheres (Figure 1A), enlarged fourth ventricle with abnormality in shape (Figure 1B), and bilaterally elongated superior cerebellar peduncles with deep interpeduncular fossa (Figure 1C), as well as horizontally oriented cerebellar peduncles on sagittal T1 weighted image (Figure 1D).
Joubert syndrome (JS) was first described by Joubert in 1969 as an autosomal recessive inherited disorder with defective development of cerebellar vermis and brainstem (1). JS mostly occurs in male children. Hypotonia and ataxia are the most common characteristic signs of JS, and most of the children with JS have cognitive dysfunction (2). Other findings of JS include cystic kidney disease, retinal dystrophy, hepatic fibrosis, and polydactyly, colobomas (3). JS is characterized by the key imaging abnormality of the cerebellum and the brainstem, which is known as the “molar tooth sign” (MTS) (3). The MTS has been identified in a group of disorders termed JS and related disorders (JSRDs) that are associated with a number of systemic congenital abnormalities (4).
Saraiva et al. in 1992 have suggested the following diagnostic criteria for JS: vermis hypoplasia, developmental delay, hypotonia, abnormal breathing and/or abnormal eye movements. These reports confirmed the MTS as the fundamental diagnostic imaging attribute (2,4,5). MTS is a cerebellar vermis hypoplasia that resulted from an abnormally deep interpeduncular fossa, and thickened, elongated cerebellar peduncles (6). In addition, the fourth ventricle appears as a “bat-wing” (6). The partial or complete absence of cerebellar vermis results in the separation of bilateral cerebellar hemispheres at the midline, allowing fine-line cerebrospinal fluid. Both clinical and radiographic examination confirmed that the case had diagnostic criteria of JS.
Over the past several decades, increasing attention has been paid to the genetic basis of JS. In the year 2013 Romani et al. identified 21 causative genes (7). Moreover, in the year of 2017, Vilboux et al. claimed that there were more than 30 genes (NPHP1, OFD1, TCTN2, TCTN3, TMEM138, TMEM216, TMEM231 and so on) associated with JS (8). Till now, more than 35 genes have been confirmed to be the cause of JS by mutating in an autosomal-recessive or X-linked manner (9). This suggests that there are more and more causative genes that need to be identified by innovative technologies. The rapid rate of genetic discoveries plays an important role in addressing the issue on genetic counseling and is expected to bridge the gap in the identification of potential targets for treating JS (7).
Acknowledgments
Funding: This work was supported by Medical and Health Science and Technology Planning Project of Zhejiang Province in 2019, China (No. 2019319609).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and accompanying images.
References
- İpek Ö, Akyolcu Ö, Bayar B. Physiotherapy and Rehabilitation in a Child with Joubert Syndrome. Case Rep Pediatr 2017;2017:8076494. [Crossref] [PubMed]
- Poretti A, Snow J, Summers AC, Tekes A, Huisman TAGM, Aygun N, Carson KA, Doherty D, Parisi MA, Toro C, Yildirimli D, Vemulapalli M, Mullikin JC. NISC Comparative Sequencing Program, Cullinane AR, Vilboux T, Gahl WA, Gunay-Aygun M. Joubert syndrome: neuroimaging findings in 110 patients in correlation with cognitive function and genetic cause. J Med Genet 2017;54:521-9. [Crossref] [PubMed]
- Kroes HY, Monroe GR, van der Zwaag B, Duran KJ, de Kovel CG, van Roosmalen MJ, Harakalova M, Nijman IJ, Kloosterman WP, Giles RH, Knoers NV, van Haaften G. Joubert syndrome: genotyping a Northern European patient cohort. Eur J Hum Genet 2016;24:214-20. [Crossref] [PubMed]
- Bin Dahman HA, Bin Mubaireek AH, Alhaddad ZH. Joubert syndrome in a neonate: case report with literature review. Sudan J Paediatr 2016;16:53-7. [PubMed]
- Buke B, Canverenler E, İpek G, Canverenler S, Akkaya H. Diagnosis of Joubert syndrome via ultrasonography. J Med Ultrason (2001) 2007;44:197-202. [Crossref] [PubMed]
- Awais M, Husen Y, Rehman A. A Molar Tooth Brainstem With A Bat-Wing Fourth Ventricle: Joubert Syndrome. J Ayub Med Coll Abbottabad 2018;30:313-4. [PubMed]
- Romani M, Micalizzi A, Valente EM. Joubert syndrome: congenital cerebellar ataxia with the molar tooth. Lancet Neurol 2013;12:894-905. [Crossref] [PubMed]
- Vilboux T, Doherty DA, Glass IA, Parisi MA, Phelps IG, Cullinane AR, Zein W, Brooks BP, Heller T, Soldatos A, Oden NL, Yildirimli D, Vemulapalli M, Mullikin JC. Nisc Comparative Sequencing Program, Malicdan MCV, Gahl WA, Gunay-Aygun M. Molecular genetic findings and clinical correlations in 100 patients with Joubert syndrome and related disorders prospectively evaluated at a single center. Genet Med 2017;19:875-82. [Crossref] [PubMed]
- Alkanderi S, Molinari E, Shaheen R, Elmaghloob Y, Stephen LA, Sammut V, Ramsbottom SA, Srivastava S, Cairns G, Edwards N, Rice SJ, Ewida N, Alhashem A, White K, Miles CG, Steel DH, Alkuraya FS, Ismail S, Sayer JA. ARL3 mutations cause Joubert syndrome by disrupting ciliary protein composition. Am J Hum Genet 2018;103:612-20. [Crossref] [PubMed]


