A case of lower-neck cystic lymphangioma: correlative US, CT and MR imaging findings
Introduction
Cystic lymphangioma is a rare malformation characterized by cystic structure deriving from detachment of lymph sacs from venous drainage systems (1). The cystic variant of lymphangioma is included in the general classification of lymphangiomas according to Landing and Farber (2) enclosing the capillary and venous variant, characterized respectively by dilatation of capillary and sinusoidal lymphatic vessels (the latter with continued growth of the stromal component) which remain connected to the lymphatic network; The cystic variant instead is unconnected with the lymphatic network, characterized by several spaces filled with proteinaceous and chylous material which contains lymphocytes and sometimes red blood cells (3). Patients suffering from cystic lymphangioma of the neck and mediastinum are often asymptomatic, but because of lesion growth they may present cough, respiratory disorders, dysphagia, or vascular compression syndromes. Complications arising from non-surgical resection include haemorrhages and infections (3).
We report a case of a 26-year-old woman suffering from cystic lymphangioma of the lower neck and mediastinal aditus diagnosed during clinical-instrumental diagnostic work-up for chronic neutropenia and dysphagia, in which ultrasonography (US), computed tomography (CT) and MR images clearly described lesion features suggesting pathological process type.
Case report
A 26-year-old woman with a family history of lymphoproliferative disorders was admitted to the department of Hematology of University of Naples “Federico II” to investigate a chronic neutropenia and a slight dysphagia. Pathological blood values found during hospitalization were as follows: white blood cells, 2.8×103/mm3 (N.V.: 4.0-10.0); neutrophils, 1.42×103/mm3 (N.V.: 1.6-7.0). The other routine laboratory examinations were unremarkable.
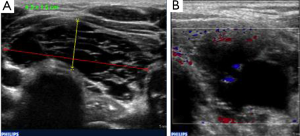
For patient dysphagia, US of the neck region was performed showing a hypo-anechoic mass of about 4.5 cm × 1.5 cm, with no significant vascular signal at color-Doppler, at the level of the lower neck; The lesion was inhomogeneous showing internal septa (Figure 1).
To confirm US findings the patient underwent CT of the neck and chest using a 64-rows scanner (Toshiba, Aquilion 64, Japan). The CT acquisitions were performed before and 70 s after the intravenous bolus administration of 120 cc iodinated non-ionic contrast agent. The CT images showed a hypodense mediastinal mass, 3 cm in diameter, in contact with the left upper dorsal tracheal wall; the lesion had regular borders and spontaneous low density with minimal enhancement after administration of contrast medium (Figure 2).

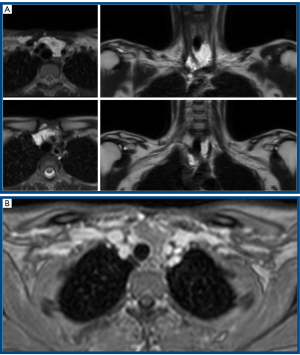
As additional diagnostic examination Magnetic Resonance Imaging (MRI) of the chest was performed using a 1.5 TMR device (Philips, Achieva, Netherlands) before and after intravenous administration of gadopentetate dimeglumine (120 cc). The MR images confirmed the presence of a cystic mass, surrounding the trachea for a longitudinal extension of about 5 cm, interposing among epiaortic vessels and having posteriorly relations with the cervical esophagus, marking it; The mass showed internal sepimentations and late minimal peripheral contrast enhancement (Figure 3).
US guided fine needle aspiration of the microcystic lesion was performed. Cytological examination documented the presence of massive infiltrate of lymphoid cells; Cytofluorimetric examination documented a population made up almost exclusively of non-clonal T lymphocytes, ruling out B and T cell lymphoma disorders. These results together with imaging findings were diagnostic for lymphangioma or cystic hygroma of the neck. Although surgical resection was the recommended treatment, the patient refused to undergo surgery.
Discussion
Cystic lymphangioma or cystic hygroma is a low-flow vascular malformation, developing where the lymph sacs are separated from the venous drainage system. The most common location is the neck region (75%), especially in the posterior triangle and in the back cervical cavity, but it can be also found in axillary region (20%) and infrequently in the retroperitoneum, mesentery, omentum, colon, pelvis, groin, bone, skin, scrotum and spleen (4); Only 1% of cystic lymphangiomas has mediastinal localization and in this case the most frequent locations are the anterior and upper mediastinum (50-60%), while the middle and posterior mediastinum occur more rarely (20%). In literature are described cases of cystic lymphangioma of the mediastinum localized in the right paratracheal (1,5,6), paracardiac (7), anterior (8) and posterior mediastinal (9-11) regions.
Our case deals with a cystic hygroma that from the lower neck reaches the upper mediastinum and extends in antero-posterior direction from the retrosternal region to the anterior face of the esophagus, crossing the epiaortic vessels. Approximately 70% of cystic hygromas is already present at birth and more than 90% gives clinical manifestations within the first 2 years of life; Symptoms depend primarily on the location of the lesion and the possibility for the mass to grow rapidly for the onset of haemorrhages or infections. Patients with lymphangioma of the neck and mediastinum are usually asymptomatic but they may present chest pain, cough, dyspnea, dysphagia, or vascular compression syndromes if the lesion reaches dimensions large enough to cause compression of adjacent structures. Just for the tendency to expand locally and for the risk of complications surgical resection is the treatment of choice for cystic. In our case the patient had dysphagia due to the posterior extension of the lesion, while the neutropenia was not related to the presence of the lymphangioma. Even if cystic lymphangioma can occur with atypical findings, such as heterogeneous content, irregular borders and calcification, the diagnosis may be obvious in cases of typical features, such as fluid content and regular margins. Imaging has a fundamental role in the detection and characterization of the cystic component, in the diagnosis of cystic lymphangioma either with US and CT as well as with MR. Moreover, imaging can help in the differential diagnosis between cystic lymphangioma and other cystic masses including cystic thymoma, cystic teratoma, hematomas, necrotic tumors and abscess (1,3). US is the first level study to investigate a suspected mass of the lower-neck because of its non-invasiveness, low cost and non-use of ionizing radiation. In our case the lesion was correctly characterized by US with demonstration of fluid content and internal sepimentations without significant vascularization.
However, US needs to be integrated with CT and MR scans because of its non panoramic view and for obtaining more information about structural features and internal as well as peripheral enhancement patterns. CT scan is currently performed with multi-slice technique that allows volumetric acquisition of the selected anatomic region with multi-planar reconstruction using different methods (MPR, MIP, SSD, VR); However, CT imaging is performed with radiation exposure. Conversely, MR can give specific information about the fluid content even when the CT shows greater intralesional attenuation values for the presence of proteinaceous material; Moreover, MR is helpful in surgical planning for its multiplanarity and high contrast resolution. In our case MR gave us further details about the nature of cystic-sepimented lesion, it defined its anatomic extension with adjacent structures; In particular, the close proximity to the brachial-cephalic and common carotid arteries was detected; MR better evaluated the enhancement after contrast administration that was not significant, late and peripheral. The lesion was clearly hyperintense on T2-weighted images compared to muscular tissues as well as epiaortic vessels, being thus easily identified and characterized as mainly a fluid mass; T1-weighted sequences after contrast administration were also used, but pre-contrast T2-weighted images were already diagnostic. The definitive diagnosis of cystic lymphangioma is histological after surgical resection; however, the percutaneous needle biopsy was considered conclusive in cases of retroperitoneal localization (12). In our case, the patient refused to undergo surgery but the results of cytologic exam and cyto-fluorimetry obtained by using FNAB were concordant in terms of a diagnosis for cystic lymphangioma.
In conclusion, integrated as well as correlative diagnostic imaging is useful in evaluation of cystic lymphangioma clearly demonstrating lesion structure and morphology; In particular, US and MRI, avoiding CT radiation exposure, should be preferred since patients need repeated scans before surgery or during the follow-up when surgical treatment is refused or post-poned; Furthermore, the tridimensional imaging evaluation using advanced modalities is fundamental to assess lesion anatomy and local spread.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Correia FM, Seabra B, Rego A, et al. Cystic lymphangioma of the mediastinum. J Bras Pneumol 2008;34:982-4. [PubMed]
- Khobta N, Tomasini P, Trousse D, et al. Solitary cystic mediastinal lymphangioma. Eur Respir Rev 2013;22:91-3. [PubMed]
- Shaffer K, Rosado-de-Christenson ML, Patz EF Jr, et al. Thoracic lymphangioma in adults: CT and MR imaging features. AJR Am J Roentgenol 1994;162:283-9. [PubMed]
- Mohammadi A, Ghasemi-rad M, Abassi F. Asymptomatic lymphangioma involving the spleen and mediastinum in adults. Med Ultrason 2013;15:154-6. [PubMed]
- Misthos P, Sepsas E, Kokotsakis I, et al. Asymptomatic solitary mediastinal cystic lymphangioma: a rare entity. Asian Cardiovasc Thorac Ann 2006;14:476-8. [PubMed]
- Hunt I, Eaton D, Dalal P, et al. Minimally invasive excision of a mediastinal cystic lymphangioma. Can J Surg 2009;52:E201-2. [PubMed]
- Conte G, Aldrovandi A, Reverberi C, et al. Mediastinal cystic lymphangioma. J Am Coll Cardiol 2011;57:e207. [PubMed]
- Bossert T, Gummert JF, Mohr FW. Giant cystic lymphangioma of the mediastinum. Eur J Cardiothorac Surg 2002;21:340. [PubMed]
- Yildirim E, Dural K, Kaplan T, et al. Cystic lymphangioma: report of two atypical cases. Interact Cardiovasc Thorac Surg 2004;3:63-5. [PubMed]
- Oshikiri T, Morikawa T, Jinushi E, et al. Five cases of the lymphangioma of the mediastinum in adult. Ann Thorac Cardiovasc Surg 2001;7:103-5. [PubMed]
- Kanzaki M, Kikkawa T, Obara T, et al. Successful excision of an isolated mediastinal cystic lymphangioma with bilateral thoracoscopic surgery. Ann Thorac Cardiovasc Surg 2011;17:570-2. [PubMed]
- Sarno RC, Carter BL, Bankoff MS. Cystic lymphangiomas: CT diagnosis and thin needle aspiration. Br J Radiol 1984;57:424-6. [PubMed]


